Abstract
Purpose
To estimate annual health care and productivity loss costs attributable to overweight or obesity in working asthmatic patients.
Materials and Methods
This study was conducted using the 2003–2013 Medical Expenditure Panel Survey (MEPS) in the United States. Patients aged 18 to 64 years with asthma were identified via self-reported diagnosis, a Clinical Classification Code of 128, or a ICD-9-CM code of 493.xx. All-cause health care costs were estimated using a generalized linear model with a log function and a gamma distribution. Productivity loss costs were estimated in relation to hourly wages and missed work days, and a two-part model was used to adjust for patients with zero costs. To estimate the costs attributable to overweight or obesity in asthma patients, costs were estimated by the recycled prediction method.
Results
Among 11670 working patients with a diagnosis of asthma, 4428 (35.2%) were obese and 3761 (33.0%) were overweight. The health care costs attributable to obesity and overweight in working asthma patients were estimated to be $878 [95% confidence interval (CI): $861–$895] and $257 (95% CI: $251–$262) per person per year, respectively, from 2003 to 2013. The productivity loss costs attributable to obesity and overweight among working asthma patients were $256 (95% CI: $253–$260) and $26 (95% CI: $26–$27) per person per year, respectively.
Conclusion
Health care and productivity loss costs attributable to overweight and obesity in asthma patients are substantial. This study's results highlight the importance of effective public health and educational initiatives targeted at reducing overweight and obesity among patients with asthma, which may help lower the economic burden of asthma.
The prevalence of asthma in the United States has increased significantly over the last decade, and an estimated 24 million persons in the US were diagnosed with asthma in 2014.12 Asthma increases medical costs and may be associated with activity limitations, inability to work, increased number of sick days, and unemployment.34 The total incremental cost of asthma is estimated at $67–$75 billion (2015 dollars).56 Prescription drugs represent the biggest component of asthma medical costs, and job loss is estimated to account for 61% of the indirect costs attributable to asthma.7 Estimated missed work days attributable to asthma have been associated with an estimated $301 for each worker per year (2015 dollars).5
Obese individuals incur substantially greater medical costs, compared to normal-weight persons;89 per capita healthcare costs attributable to obesity are estimated at $1889–$4380 (2015 dollars), which is significantly higher than costs incurred by normal weight individuals.1011 Furthermore, obesity also significantly increases absenteeism costs,12 and concurrent obesity exacerbates the impact of chronic diseases on medical expenditures, missed work days, and lost productivity.13
Body mass index (BMI) has been shown to be negatively associated with various lung volume measures, and obesity has been correlated with lower lung function and more comorbidities among asthma patients.14 Increasing BMI has been found to be significantly associated with worsening asthma severity,15 greater asthma symptoms, poorer asthma control,1617 more activity limitations, worse general physical health status, more missed workdays, and more medication use and hospitalization.151819 Compared to normal-weight patients with asthma, overweight or obese patients tend to have more asthma-related hospitalizations, more emergency department visits, and more unscheduled urgent care visits, regularly scheduled visits, and follow-up visits for an asthma episode.1920 Studies conducted among non-elderly and elderly asthma patient cohorts have demonstrated a significant impact of obesity on healthcare costs.1021
Although previous studies have consistently shown the significant economic impact of asthma or obesity on medical costs and lost productivity, the total incremental costs of obesity among patients with asthma have not been estimated. The objective of this study was to estimate the annual health care and productivity loss costs attributable to overweight or obesity in working asthma patients in the US from 2003 to 2013 using the Medical Expenditures Panel Survey (MEPS).
The data source for this study was the 2003–2013 MEPS, which has been conducted annually since 1996 under the sponsorship of the Agency for Healthcare Research and Quality and the National Center for Health Statistics.22 The MEPS survey provides nationally representative estimates of health care use, expenditures, sources of payment, and health insurance coverage for the US civilian non-institutionalized population. The panel design of the survey, comprising five rounds of interviews covering two full calendar years, allows for the examination of person-level changes in expenditures, health insurance coverage, and health status. Eight years of pooled MEPS-HC data were merged with the full-year consolidated file using unique identifiers to ensure sufficient sample size and produce estimates with high reliability.22 For the pooled analysis, survey weights provided by MEPS were used to generate nationally representative results.
Patients with an asthma diagnosis were identified using International Classification of Diseases, 9th Revision (ICD-9) codes (493.xx), the Clinical Classification Code (CCC) (128), or a MEPS self-report of asthma. To estimate productivity loss costs, the study population was limited to working patients aged 18 to 64 years, who were selected if they answered yes to the question "are you currently employed or employed" during the reference period (i.e., time period between the date of the previous round's interview and the date of the current round's interview)" at least once for the employment status question in each round. Exclusion criteria included a diagnosis of malignancy (ICD-9 code: 140–239, CCC: 011–045, or if they answered "yes" to "Have you ever been diagnosed as having cancer or a malignancy of any kind?"), pregnancy (ICD-9 code: 633–650 or CCC: 177–196), kidney dialysis (ICD-9 code: V56 or CCC: 158), human immunodeficiency virus (ICD-9 code: 042, 043, 996, V08, V42, V43, V49, or CCC: 005), or BMI <18.5 kg/m2.
Study outcomes included treatment costs and productivity loss costs. All-cause health care costs were derived from the sum of expenditures associated with medical services (e.g., hospitalizations, office-based/outpatient visits, and emergency department visits) and prescription drugs. These expenditures in MEPS were defined as the sum of the direct payments for care provided during the year, including out-of-pocket payments and payments through private insurance, Medicaid, Medicare, and other sources. Payments for over-the-counter drugs and alternative care services were excluded.22
Productivity loss costs were estimated based on missed work days due to illness, injury, or mental or emotional problems during the reference period, and were valued using the average hourly wage by occupation, obtained from the Unites States Bureau of Labor Statistics in 2015.23 Since the number of work days lost were provided in MEPS as ≥0.5 days, we could not distinguish half versus full days missed; one missed day was considered to be 6 hours, consistent with previous studies using MEPS.24 Annual missed work days were calculated using the reference period (the period of time during which the data for each person were collected).
To examine the impact of overweight and obesity on costs, asthma patients were classified into three groups based on BMI calculated using self-reported height and weight from MEPS: normal (18.5 kg/m2 ≤BMI <25 kg/m2), overweight (25 kg/m2 ≤BMI <30 kg/m2), and obese (BMI ≥30 kg/m2).2526 Self-reported patient characteristics were also evaluated to adjust for factors that may potentially confound the association between BMI status and study outcomes, including patient age, gender, race/ethnicity, insurance status, smoking status, marital status, income, and occupation. Insurance status was categorized into public, private, both public and private, or uninsured types. Smoking status was categorized into former/never smoker and current smoker types.
Comorbidities included the following: cardiovascular disease [ICD-9-CM code: 410–417, 428, 429, 798; CCC: 101–104, 108; or if they answered "yes" to "Have you ever been diagnosed as having heart disease (coronary heart disease, angina, angina pectoris, heart attack, myocardial infarction, or any other kind of heart disease or condition)?"]; cerebrovascular disease (ICD-9-CM code: 430–438, CCC: 109–113, or if they answered "yes" to "Have you ever been diagnosed as having had a stroke or transient ischemic attack?"); hypertension (ICD-9-CM code: 401–405, CCC: 98–99, or if they answered "yes" to "Have you ever been diagnosed as having high blood pressure?"); diabetes (ICD-9-CM code: 250, CCC: 49–50, or if they answered "yes" to "Have you ever been diagnosed with diabetes?"); hyperlipidemia (ICD-9-CM code: 272, 440, 445; CCC: 53, 114, 116; or if they answered "yes" to "Have you ever been diagnosed as having high cholesterol?"); mental disorder (ICD-9-CM code: 295, 296, 300, 311; CCC: 657, 659, 670; or if they answered "yes" to "Have you ever been diagnosed as having attention deficit hyperactivity disorder or attention deficit disorder?"); and a respiratory disease other than asthma (ICD-9-CM code: 460–492, 494–516; CCC: 122–127, 134; or if they answered "yes" to "Have you ever been diagnosed as having emphysema or chronic bronchitis?").
Differences in demographic and clinical characteristics stratified by BMI category were compared using the chi-squared test and analysis of variance test. Unadjusted average all-cause annual medical costs and productivity loss costs were calculated, and a 95% confidence interval (CI) was obtained using bootstrap methods with 1000 iterations, since these costs did not follow a normal distribution.527
A generalized linear model (GLM) with log link function and a gamma distribution was used to identify the significant factors associated with medical costs in asthma patients and to estimate regression coefficients.352829 The dependent variable in the model was patient BMI, classified as either overweight, obese or normal-weight, and independent variables included age, gender, race/ethnicity, insurance status, marital status, income, and comorbidities. To estimate health care costs attributable to overweight or obesity, the recycled prediction method was used.29303132 Using the calculated coefficients of the study covariates, costs were estimated by assuming that everybody was obese (i.e., by treating the indicator variable as equal to 1), and then re-estimated by assuming that everybody was normal (i.e., by treating the indicator variable as equal to 0). The mean difference between the two estimated costs was calculated to reflect the costs attributable to obesity in asthma patients. The same process was used to estimate the medical costs attributable to overweight in asthma patients.
Productivity loss costs were calculated using the two-part model
since many patients incurred zero productivity loss costs.53033 In the first part of the two-part model, a logistic model was used to predict the probability of any costs, and in the second part, a GLM with a log link function and a gamma distribution was used to predict productivity loss costs for positive costs only. In both models, costs were estimated adjusting for age, gender, race/ethnicity, insurance status, marital status, income, occupation, and comorbidities. Productivity loss costs attributable to overweight or obesity in asthma patients were estimated using the same methodology as for medical costs described above.
For all analyses, MEPS sampling and variance adjustment weights were considered to reflect the survey design structure for the estimation of national representative values. All costs were converted to 2015 US dollars using the consumer price index (CPI).34 Data were analyzed using SAS 9.2 (SAS Institute, Cary, NC, USA) and STATA 10.1 (STATA Corporation, College Station, TX, USA).
Among 381682 subjects in MEPS from 2003 to 2013, 11670 workers were identified as asthma patients aged 18 to 64 years based on study selection criteria. Of these patients, 3761 (33.0%) were overweight, and 4428 (35.2%) were obese. Demographic characteristics of asthma patients stratified by BMI category are shown in Table 1. Obese patients with asthma were significantly more likely to be older, female, and non-Hispanic white. Obese patients with asthma were more likely to have cardiovascular disease, hypertension, hyperlipidemia, and other respiratory disease as comorbidities.
Obese patients with asthma incurred significantly higher annual medical costs across all service categories than normal-weight and overweight asthma patients (Table 2). An unadjusted average annual medical costs for obese patients with asthma were $5412 (95% CI: $4899–$5817) per patient, 40% higher than overweight patients ($3873; 95% CI: $3395–$4226) and 60% higher than normal-weight patients ($3385; 95% CI: $2527–$4191). Furthermore, regardless of BMI category, outpatient visits accounted for the highest proportion of treatment costs, followed by prescription drugs, inpatient visits, and ED visits.
Obese patients with asthma also had higher productivity loss costs than overweight or normal-weight patients (Table 2). The unadjusted average annual productivity loss costs for obese patients were $745 (95% CI: $664–$826) per patient, 72% higher than those of overweight ($434; 95% CI: $381–$487) and over two times those of normal weight ($353; 95% CI: $312–$393). The increasing productivity loss costs by BMI category resulted from the increasing effect of BMI on missed work days. Total missed work days averaged 2.7 (95% CI: 2.4–3.0) in normal-weight patients, 3.3 days (95% CI: 2.9–3.7) in overweight patients, and 5.6 days (95% CI: 5.0–6.3) in obese patients. Obese and overweight patients experienced an additional mean of 2.9 and 0.6 days lost from work per year, respectively, compared to normal-weight patients.
Average annual medical costs for working asthma patients increased with patient age (Fig. 1), and the increasing effect of BMI on average annual medical costs was consistent across all age groups. Average annual productivity loss costs increased for the 41 to 50 years age group but declined for the 51 to 64 years age group, suggesting a lower labor force participation rate in the latter age group among the general population (Fig. 2).
Annual total treatment costs for working asthma patients increased significantly when patients were obese, older, female, or had comorbid cardiovascular disease, hypertension, or hyperlipidemia (Table 3). Obese patients with asthma had significantly higher treatment costs (cost ratio: 1.20; 95% CI: 1.04–1.39) than normal-weight patients after adjusting for the study variables. Obese patients with asthma had productivity loss costs 46% higher (cost ratio: 1.46; 95% CI: 1.24–1.72) than those of normal-weight patients after adjusting for the study variables.
Fig. 3 depicts the treatment costs and productivity loss costs attributable to obesity and overweight in working asthma patients. The average total costs attributable to obesity were $1103 (95% CI: $1085–$1122), nearly four times the costs attributable to overweight (mean: $280; 95% CI: $274–$286).
In this study, we estimated that 68.2% of asthma patients were overweight or obese, which is comparable to the age-adjusted prevalence of overweight and obesity (68%) in the general US adult population.25 Mean annual all-cause health care costs for obese asthma patients were $5412 per patient, 40% higher than those for overweight ($3873) and 60% higher than those for normal weight ($3385) patients. Furthermore, mean annual productivity loss costs of obese asthma patients were $745 per patient, 72% higher than those of overweight ($434) and over two times those of normal weight ($353) patients. Health care costs attributable to obesity and overweight in working asthma patients were estimated to be $878 and $257 per person per year, respectively, and productivity loss costs attributable to obesity and overweight among working asthma patients were $256 and $26 per person per year, respectively.
In the current study, mean annual all-cause health care costs for asthma patients were $4260 per patient. Of these treatment costs, in our estimation, outpatient visits and prescription drugs were the largest components, accounting for 40.6% and 32.0% of total treatment costs, respectively. Previous studies have estimated the annual incremental health care costs associated with asthma: estimates per person range from $2340 (2015 US dollars) to $9337 (2015 US dollars) in adults and $3876 (2015 US dollars) in both adults and children.34535 Kamble and Bharmal3 also reported that prescription medications and physician office visits were the major drivers of total asthma-related expenditures, constituting 49% of the total incremental costs of asthma in adults. Similarly, Sullivan, et al.4 found that prescription drugs represented the largest contributor to all-cause health care expenditures for asthma patients, followed by hospitalization. While these previous studies provided valuable insight into the economic burden of asthma, they did not account for the possibility that the BMI status of asthma patients can also influence the direct medical costs associated with asthma.
We estimated the direct and indirect costs attributable to overweight and obesity in patients with asthma at $280 and $1103 (in 2015 dollars), respectively, suggesting that excessive weight in asthma patients can have an incrementally substantial economic consequence on asthma treatment costs. While the total incremental cost of overweight/obesity among patients with asthma has not previously been studied, Sarpong10 estimated that if younger adult obese patients with asthma were normal weight, total all-cause healthcare expenditures (including prescription medications) would be expected to be decreased by $2066 (2015 US dollars) and $4378 (2015 US dollars) respectively. The incremental cost of obesity among older adult asthmatic patients was estimated at $6204 (2015 US dollars) in all-cause health care costs.21
In addition to direct medical costs, asthma patients suffered productivity loss at the rate of four missed work days per year per patient on average, and these costs increased with increasing BMI. The average productivity loss cost for obese patients with asthma was estimated at $745 per patient per year, more than twice the cost of productivity loss for normal-weight asthma patients ($434). Our estimates of productivity loss costs, even for normal-weight patients, were greater than was the estimate ($353) of the value of additional days lost due to asthma calculated by Barnett and Nurmagambetov5 Moreover, our estimates of incremental productivity loss costs for obesity ($256) relative to normal weight were greater than the costs of absenteeism associated with obesity and morbid obesity estimated by Cawley, et al.,12 which were $152 (2015 dollars) and $314 (2015 dollars) per worker, respectively, regardless of disease.
Although this study found that concurrent obesity in asthma patients had a strongly negative impact on productivity loss, further research is needed to examine how the incremental negative consequences of obesity on productivity among asthma patients compare to the other segments of the population. Our findings suggest that the benefits of weight reduction in asthma patients could be substantial, especially when the effort is focused on those with higher BMI. In fact, it is well-documented that weight reduction can offer potential clinical benefits to asthma management.36 Weight reduction among obese patients with asthma through low-calorie dieting was associated with a reduction in airway obstruction and peak expiratory flow variability in one study.37 Another randomized weight reduction program among obese people with asthma improved lung function variables such as forced vital capacity (FVC) and forced expiratory volume in one second (FEV1) and the improved lung function was sustained even after the program ended.38 Additionally, the weight reduction was shown to be beneficial in reducing the number of asthma symptoms that obese asthmatic people experienced and improving physical activities that had previously been limited by breathlessness.
While our study provides valuable information on the total incremental cost of obesity in asthma using advanced estimation methods that have not previously been used, our findings must be interpreted in light of several study limitations. We examined the economic impact of comorbid obesity in asthma patients, but could not determine the causality between obesity and costs due to the cross-sectional nature of the study. Asthma patients were identified based on self-reported diagnosis or the Clinical Classification or ICD-9 code used by physicians rather than on confirmed diagnoses of asthma through pulmonary function tests. The unavailability of pulmonary function data also precluded the consideration of asthma severity in this study. In addition, this study may have underestimated the costs attributable to obesity or overweight in asthma patients, as we did not include caregiver time costs and mortality costs. Premature mortality associated with obesity can incur increased indirect costs to employers through increased life insurance premiums and to employees through lost earnings.39 Finally, the prevalence of obesity in asthma patients may have been underestimated since BMI was based on self-reported height and weight, as suggested by other studies.40
In conclusion, the direct and indirect costs attributable to overweight and obesity in patients with asthma are substantial. This study's findings highlight the importance of targeted public health interventions for obese patients with asthma to reduce the economic burden of asthma. Public health programs to promote weight reduction and weight management among obese and overweight patients with asthma may play an important role in curbing the economic burden of asthma.
Figures and Tables
Fig. 3
Costs attributable to overweight or obesity in working asthma patients. All costs were converted to 2015 US dollars. Dollars in the parenthesis represents 95% confidence interval (CI) calculated using bootstrapping method with 1000 iterations.

Table 1
Characteristics of Asthma Patients by Body Mass Index
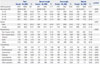
Table 2
Average Annual Treatment Costs and Productivity Loss Costs in Asthma Patients by BMI*

Table 3
Factors Influencing Treatment Costs or Productivity Loss Costs in Working Asthma Patients

ACKNOWLEDGEMENTS
The preliminary abstract of this study were presented and this study was chosen to receive the Best Research Poster Award at the International Society of Pharmacoeconomics and Outcomes (ISPOR) 14th Annual European Congress, November, 2011 in Madrid, Spain. The authors would like to thank In-Myung Song, Ph.D. for contribution with manuscript preparation. This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI13C1480). No authors has a conflict of interest with the work contained within this article.
References
1. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Summary Health Statistics for U.S. Children: National Health Interview Survey, 2012. 2013. accessed on 2016 March 15. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_258.pdf.
2. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Summary Health Statistics for U.S. Adults: National Health Interview Survey, 2012. 2014. accessed on 2016 March 15. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_260.pdf.
3. Kamble S, Bharmal M. Incremental direct expenditure of treating asthma in the United States. J Asthma. 2009; 46:73–80.

4. Sullivan PW, Ghushchyan VH, Slejko JF, Belozeroff V, Globe DR, Lin SL. The burden of adult asthma in the United States: evidence from the Medical Expenditure Panel Survey. J Allergy Clin Immunol. 2011; 127:363–369.

5. Barnett SB, Nurmagambetov TA. Costs of asthma in the United States: 2002-2007. J Allergy Clin Immunol. 2011; 127:145–152.

6. Jang J, Gary Chan KC, Huang H, Sullivan SD. Trends in cost and outcomes among adult and pediatric patients with asthma: 2000-2009. Ann Allergy Asthma Immunol. 2013; 111:516–522.

7. Cisternas MG, Blanc PD, Yen IH, Katz PP, Earnest G, Eisner MD, et al. A comprehensive study of the direct and indirect costs of adult asthma. J Allergy Clin Immunol. 2003; 111:1212–1218.

8. Trogdon JG, Finkelstein EA, Feagan CW, Cohen JW. State- and payer-specific estimates of annual medical expenditures attributable to obesity. Obesity (Silver Spring). 2012; 20:214–220.

9. Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. Obes Rev. 2011; 12:131–141.

10. Sarpong EM. The impact of obesity on medication use and expenditures among nonelderly adults with asthma. J Health Care Poor Underserved. 2014; 25:1245–1261.

11. Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009; 28:w822–w831.

12. Cawley J, Rizzo JA, Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. J Occup Environ Med. 2007; 49:1317–1324.

13. Sullivan PW, Ghushchyan V, Ben-Joseph RH. The effect of obesity and cardiometabolic risk factors on expenditures and productivity in the United States. Obesity (Silver Spring). 2008; 16:2155–2162.

14. Pakhale S, Doucette S, Vandemheen K, Boulet LP, McIvor RA, Fitzgerald JM, et al. A comparison of obese and nonobese people with asthma: exploring an asthma-obesity interaction. Chest. 2010; 137:1316–1323.

15. Taylor B, Mannino D, Brown C, Crocker D, Twum-Baah N, Holguin F. Body mass index and asthma severity in the National Asthma Survey. Thorax. 2008; 63:14–20.

16. Saint-Pierre P, Bourdin A, Chanez P, Daures JP, Godard P. Are overweight asthmatics more difficult to control? Allergy. 2006; 61:79–84.

17. Peters-Golden M, Swern A, Bird SS, Hustad CM, Grant E, Edelman JM. Influence of body mass index on the response to asthma controller agents. Eur Respir J. 2006; 27:495–503.

18. Lavoie KL, Bacon SL, Labrecque M, Cartier A, Ditto B. Higher BMI is associated with worse asthma control and quality of life but not asthma severity. Respir Med. 2006; 100:648–657.

19. Rodrigo GJ, Plaza V. Body mass index and response to emergency department treatment in adults with severe asthma exacerbations: a prospective cohort study. Chest. 2007; 132:1513–1519.

20. Mosen DM, Schatz M, Magid DJ, Camargo CA Jr. The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol. 2008; 122:507–511.

21. Shah R, Yang Y. Health and economic burden of obesity in elderly individuals with asthma in the United States. Popul Health Manag. 2015; 18:186–191.

22. Agency for Healthcare Research and Quality. MEPS HC-163: 2013 Full Year Consolidated Data File. 2015. accessed on 2016 March 31. Available at: http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h163/h163doc.pdf.
23. United States Bureau of Labor Statistics. May 2015 national occupational employment and wage estimates United States. accessed on 2016 March 15. Available at: http://www.bls.gov/oes/current/oes_nat.htm.
24. Sullivan PW, Ghushchyan V, Wyatt HR, Wu EQ, Hill JO. Productivity costs associated with cardiometabolic risk factor clusters in the United States. Value Health. 2007; 10:443–450.

25. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010; 303:235–241.

26. Valerio MA, Gong ZM, Wang S, Bria WF, Johnson TR, Clark NM. Overweight women and management of asthma. Womens Health Issues. 2009; 19:300–305.

27. Honeycutt AA, Segel JE, Hoerger TJ, Finkelstein EA. Comparing cost-of-illness estimates from alternative approaches: an application to diabetes. Health Serv Res. 2009; 44:303–320.

28. Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004; 23:525–542.
29. Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001; 20:461–494.

30. Duan N, Manning WG Jr, Morris CN, Newhouse JP. A comparison of alternative models for the demand for medical care. J Bus Econ Stat. 1983; 1:115–126.

31. Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005; 6:93–109.

32. Basu A, Arondekar BV, Rathouz PJ. Scale of interest versus scale of estimation: comparing alternative estimators for the incremental costs of a comorbidity. Health Econ. 2006; 15:1091–1107.

33. Mullahy J. Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ. 1998; 17:247–281.

34. United States Bureau of Labor Statistics. Consumer price indexes. accessed on 2016 March 31. Available at: http://www.bls.gov/cpi/.
35. Carrier E, Cunningham P. Medical cost burdens among nonelderly adults with asthma. Am J Manag Care. 2014; 20:925–932.
36. Maniscalco M, Zedda A, Faraone S, Cerbone MR, Cristiano S, Giardiello C, et al. Weight loss and asthma control in severely obese asthmatic females. Respir Med. 2008; 102:102–108.

37. Hakala K, Stenius-Aarniala B, Sovijärvi A. Effects of weight loss on peak flow variability, airways obstruction, and lung volumes in obese patients with asthma. Chest. 2000; 118:1315–1321.

38. Stenius-Aarniala B, Poussa T, Kvarnström J, Grönlund EL, Ylikahri M, Mustajoki P. Immediate and long term effects of weight reduction in obese people with asthma: randomised controlled study. BMJ. 2000; 320:827–832.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download