Abstract
Purpose
Materials and Methods
Results
Figures and Tables
Fig. 1
Unadjusted dose-response association between ALT and the risk of MS in women. MS, metabolic syndrome; ALT, alanine aminotransferase; OR: odds ratio.
Fig. 2
Adjusted dose-response association between ALT and the risk of MS in women. MS, metabolic syndrome; ALT, alanine aminotransferase; OR: odds ratio.
Fig. 3
Unadjusted dose-response association between ALT and the risk of MS in men. MS, metabolic syndrome; ALT, alanine aminotransferase; OR: odds ratio.
Fig. 4
Adjusted dose-response association between ALT and the risk of MS in men. MS, metabolic syndrome; ALT, alanine aminotransferase; OR: odds ratio.
Table 1
General Characteristics Stratified by ALT Quartiles in Women*

MS, metabolic syndrome; ALT, alanine aminotransferase; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting blood-glucose; T-CH, total cholesterol; HDL-C, high density lipoprotein cholesterol; TG, triglyceride; WBC, white blood cell count; UA, uric acid; Cr, serum creatinine; TBIL, total bilirubin.
*ALT quartiles in women were as follows: ≤11.0 U/L, 11.1–15.0 U/L, 15.1–20.0 U/L, 20.1–40.0 U/L, †Categorical variable expressed as percentages. Pearson χ2 test was used to test the difference between four groups, ‡Skewed variable expressed as median (interquartile range). Kruskal-Wills H test was used, §Normally distributed continuous variable expressed as means±SD. One-Way Analysis of Variance was used, ∥Linear regression analysis was used to test for the trend across the four groups.
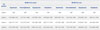
Table 2
General Characteristics Stratified by ALT Quartiles in Men*

MS, metabolic syndrome; ALT, alanine aminotransferase; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting blood-glucose; T-CH, total cholesterol; HDL-C, high density lipoprotein cholesterol; TG, triglyceride; WBC, white blood cell count; UA, uric acid; Cr, serum creatinine; TBIL, total bilirubin.
*ALT quartiles in men were as follows: ≤16.0 U/L, 16.1–21.0 U/L, 21.1–28.0 U/L, 28.1–40.0 U/L, †Categorical variable expressed as percentages. Pearson χ2 test was used to test the difference between four groups, ‡Skewed variable expressed as medians (interquartile range). Kruskal-Wills H test was used, §Normally distributed continuous variable expressed as means±SD. One-way analysis of Variance was used, ∥Linear regression analysis was used to test for the trend across the four groups.
Table 3
Logistic Regression for the Presence of MS in Relation to ALT Quartiles

MS, metabolic syndrome; ALT, alanine aminotransferase; OR, odds ratio; CI, confidence interval; WBC, white blood cell count; UA, uric acid; Cr, serum creatinine; TBIL, total bilirubin.
*Gender-specific quartiles of ALT: women (≤11.0, 11.1–15.0, 15.1–20.0, 20.1–40.0 U/L), men (≤16.0, 16.1–21.0, 21.1–28.0, 28.1–40.0 U/L), †Adjusted for age, smoking, drinking, WBC, UA, Cr and TBIL, ‡The value of OR was statically significant, p<0.05.
Table 4
Multiple Logistic Regression for the Presence of the Components of MS in Relation to ALT Quartiles
MS, metabolic syndrome; ALT, alanine aminotransferase; OR, odds ratio; CI, confidence interval; WBC, white blood cell count; UA, uric acid; Cr, serum creatinine; TBIL, total bilirubin.
*Gender-specific quartiles of ALT: women (≤11.0, 11.1–15.0, 15.1–20.0, 20.1–40.0 U/L), men (≤16.0, 16.1–21.0, 21.1–28.0, 28.1–40.0 U/L), †Adjusted for age, smoking, drinking, WBC, UA, Cr, TBIL and the components of MS other than the analyzed component, ‡The value of OR was statically significant, p<0.05.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download