Abstract
Injection medialization laryngoplasty is a procedure that has many advantages in treating vocal fold paralysis; however, undesired complications can occur. We experienced a case of a pulmonary embolism, suspected in a patient who had undergone an injection laryngoplasty with calcium hydroxylapatite (CaHA). The patient suffered dyspnea after undergoing the injection laryngoplasty. Chest embolism computed tomography (CT) scan revealed a new lesion of enhancing materials at the pulmonary vasculature in the right upper lobe. The CaHA embolism was suspected, and the patient was treated with warfarin for 12 months. The patient's symptom of dyspnea nearly disappeared and a follow up chest embolism CT scan revealed no signs of the previous lesion. Thus, we would like to report this rare case along with a review of the literature.
Injection laryngoplasty is a procedure that provides support to the vocal fold that lacks either the volume (e.g., vocal fold bowing) or the mobility (e.g., paralysis) it once had.12 The procedure can re-volume up the vocal fold to move it towards the opposite vocal fold and make the folds contact again for speaking.23
Radiesse (Merz Aesthetic Inc., USA) is one of injectable filler that is a sterile, semi-solid, injectable implant whose principal component is synthetic calcium hydroxylapatite (CaHA), and is biocompatible with use in medical application for over 20 years.45 A few cases, however, have been reported about vascular occlusion associated with percutaneous injection filler, resulting in pulmonary embolism (PE).6
We experienced a patient who was diagnosed with PE after percutaneous injection laryngoplasty, and would therefore like to present the case as well as a literature review.
A 63-year-old female patient was experiencing a change in her voice after thyroidectomy due to thyroid papillary carcinoma, which was done approximately 3 months ago. Endoscopic evaluation of the larynx revealed a right vocal fold paralysis. Results from other physical examinations and past medication history were unremarkable. We studied the CT scan for another cause of vocal fold palsy. However, the patient's lungs were clear and no signs of a heart problem (Fig. 1).
After careful examination of her vocal folds, a Radiesse injection was performed on the right vocal fold through cricothyroid membrane under local anesthesia. The procedure did not go as planned since the patient suddenly coughed and moved during the injection laryngoplasty, thereby causing an accidental injection around the vocal fold (Fig. 2A and B). The inadvertently injected CaHA around vocal fold was seen CT scan of inferior larynx area (Fig. 2C).
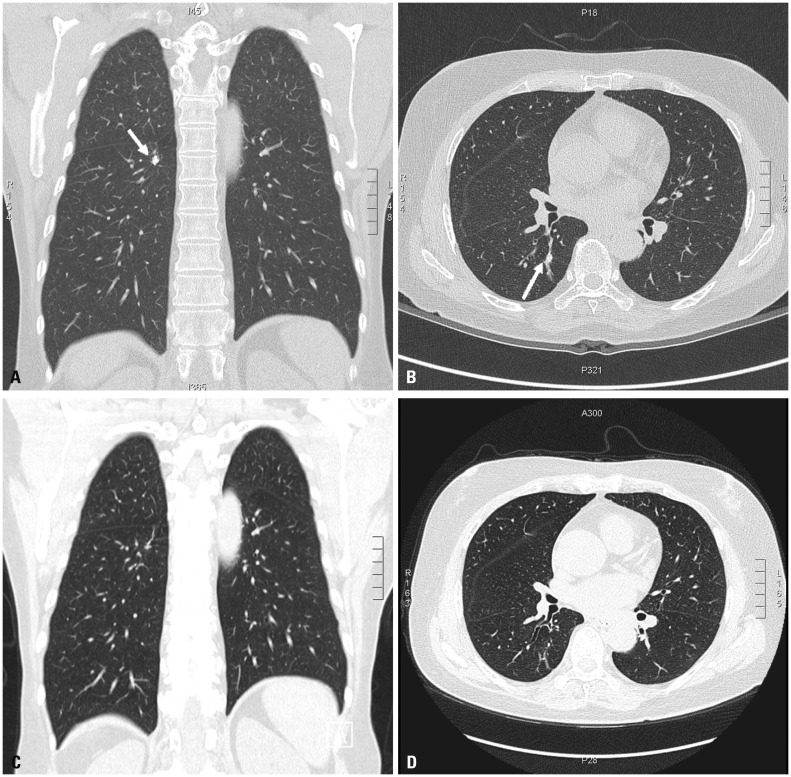
The total volume of injected Radiesse was 1.4 mL. After the procedure, the patient suffered from dyspnea. A chest embolism computed tomography (CT) scan revealed a high-density lesion at the pulmonary vasculature in the right upper lobe (Fig. 3A and B).
It revealed the right lung and right vocal fold corresponding to the Radiesse injection done previously. The CaHA PE was suspected, and the patient was treated with warfarin for 12 months. During the follow up, the patient consistently had mild dyspnea.
After 6 months on warfarin, the chest embolism CT revealed that the calcified embolus still existed. At 12 months, the patient's dyspnea symptoms had nearly disappeared and she was able to climb the stairs without stress. The follow-up chest embolism CT scan did not show the embolus lesion of the right lung any more (Fig. 3C and D). We concluded that the CaHA had been re-absorbed and just a follow up of the patient was required. At 2 years, the patient did not have any lingering problems associated with this past experience.
A variety of conditions may lead to dysphonia caused by glottal insufficiency. One of the most common causes is a lesion of the recurrent laryngeal nerve.7 There are many techniques available to adjust for the insufficiency.8 Some of the commonly used techniques involve injecting biomaterials inside the vocal fold for augmentation or medialization.7
One of the significant adverse effect with percutaneous soft tissue augmentation injections is vascular occlusion.9 A few cases have been published on vascular occlusion associated with percutaneous injection procedures and PE after percutaneous kyphoplasty.6 In fact, there was no case of PE associated with percutaneous injection laryngoplasty.
In the present case, the exposure to CaHA in the vessels around the vocal fold led to PE and to the passage of the CaHA in the inferior thyroid veins or inferior laryngeal vein and then into the subclavian vein, ending up in the vasculature. Because of some of inadvertently injected CaHA was seen in the CT scan of inferior larynx area, we suppose that the inadvertent injection was a main cause of PE. Otherwise, the inadvertently injection was happen above of vocal cord, the CaHA was drainage to internal jugular vein and pulmonary vasculature.
In the chest embolism CT scan, we could see only small calcified emboli in the right upper lobe. However, as the patient suffered from dyspnea right after the injection laryngoplasty and considering the patient symptoms, there must have also been multiple other small PE in the lung that can't be found by CT, and small calcified emboli alone couldn't have brought the symptoms.
The CaHA PE is very rare and there is no confirmed treatment method. We consider the CaHA PE as a cement PE in percutaneous kyphoplasty.6 Some authors suggest a protocol of cement PE that applies warfarin (anticoagulation agent) for 3–6 months.6 If symptoms are mild, patient needs only to be closely observed with anticoagulant therapy. In our case, the patient's symptom of dyspnea disappeared nearly after 12 months, and she was able to climb the stairs without stress. In addition, the follow-up chest embolism CT scan did not show the high-density lesion at the right lung previously seen.
Injectable fillers like CaHA have become increasingly popular. Although the majority of adverse reactions are mild and transient, physicians should be aware of the possibility of PE and caution is required while performing procedures with these agents.
ACKNOWLEDGEMENTS
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science, ICT, and Future Planning (2016R1A2B4013000).
The research was also supported by the Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (2012K1A4A3053142).
References
1. Woo SH, Kim JP, Park JJ, Chung PS, Lee SH, Jeong HS. Autologous platelet-poor plasma gel for injection laryngoplasty. Yonsei Med J. 2013; 54:1516–1523. PMID: 24142660.

2. Woo SH, Son YI, Lee SH, Park JJ, Kim JP. Comparative analysis on the efficiency of the injection laryngoplasty technique using calcium hydroxyapatite (CaHA): the thyrohyoid approach versus the cricothyroid approach. J Voice. 2013; 27:236–241. PMID: 23280385.

3. Mallur PS, Rosen CA. Vocal fold injection: review of indications, techniques, and materials for augmentation. Clin Exp Otorhinolaryngol. 2010; 3:177–182. PMID: 21217957.

4. Jacovella PF. Use of calcium hydroxylapatite (Radiesse) for facial augmentation. Clin Interv Aging. 2008; 3:161–174. PMID: 18488886.
5. DeFatta RA, Chowdhury FR, Sataloff RT. Complications of injection laryngoplasty using calcium hydroxylapatite. J Voice. 2012; 26:614–618. PMID: 22056892.

6. Kollmann D, Hoetzenecker K, Prosch H, Ankersmit HJ, Aigner C, Taghavi S, et al. Removal of a large cement embolus from the right pulmonary artery 4 years after kyphoplasty: consideration of thrombogenicity. J Thorac Cardiovasc Surg. 2012; 143:e22–e24. PMID: 22424531.

7. Cantillo-Baños E, Jurado-Ramos A, Gutiérrez-Jódas J, Ariza-Vargas L. Vocal fold insufficiency: medialization laryngoplasty vs calcium hydroxylapatite microspheres (Radiesse Voice®). Acta Otolaryngol. 2013; 133:270–275. PMID: 23145984.

8. Lodder WL, Dikkers FG. Comparison of voice outcome after vocal fold augmentation with fat or calcium hydroxylapatite. Laryngoscope. 2015; 125:1161–1165. PMID: 25545723.

9. Hsiung MW, Woo P, Minasian A, Schaefer Mojica J. Fat augmentation for glottic insufficiency. Laryngoscope. 2000; 110:1026–1033. PMID: 10852525.

Fig. 1
The preoperative CT scan, showing no signs of lung and heart problem. (A) Coronal view. (B) Axial view.
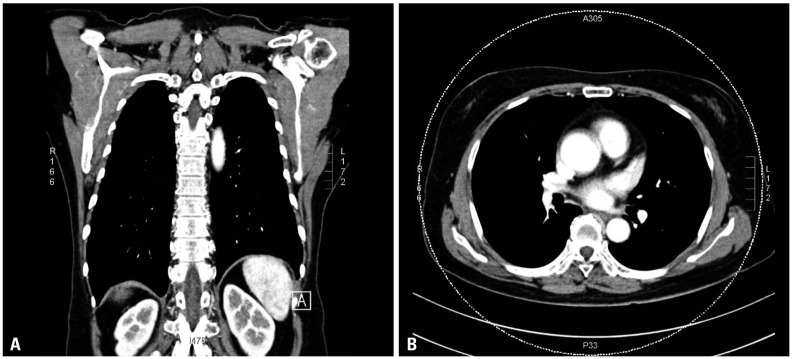
Fig. 2
An accidental injection of CaHA around the vocal fold (A), high-density lesion in the right vocal fold (B: arrow) and inferior larynx (C: arrow). CaHA, calcium hydroxylapatite.
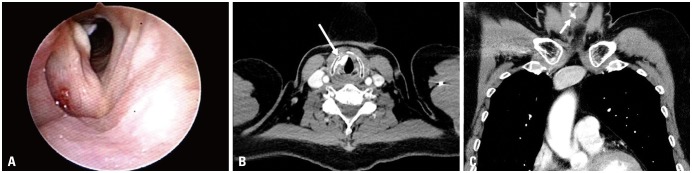
Fig. 3
A chest embolism CT scan revealed a high-density lesion in the pulmonary vasculature (arrows), most predominantly in the right upper lobe, which was thought to be caused by the CaHA injection (A and B). The follow-up chest embolism CT scan did not show the embolus lesion of the right lung previously seen (C and D). CaHA, calcium hydroxylapatite.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download