Abstract
Purpose
To demonstrate the impact of correcting sagittal balance (SB) on functional outcomes of surgical treatment for degenerative spinal disease and actual falls via utilization of new minimally invasive lumbar fusion techniques via a lateral approach.
Materials and Methods
From November 2011 to March 2015, we enrolled 56 patients who underwent minimally invasive lateral lumbar interbody fusion (LLIF) and matched 112 patients receiving decompression/postero-lateral fusion (PLF) surgery for lumbar spinal stenosis. According to SB status using C7-plumb line-distance (C7PL) and surgery type, patients were divided into three groups: SB PLF, sagittal imbalance (SI) PLF, and LLIF groups. We then compared their outcomes.
Results
The mean C7PL was 6.2±13.6 mm in the SB PLF group, 72.9±33.8 mm in the SI PLF group, and 74.8±38.2 mm in the LLIF group preoperatively. Postoperatively, C7PL in only the LLIF group improved significantly (p=0.000). Patients in the LLIF group showed greater improvement in fall-related functional test scores than the SI PLF group (p=0.007 for Alternate-Step test, p=0.032 for Sit-to-Stand test). The average number of postoperative falls was 0.4±0.7 in the SB PLF group, 1.1±1.4 in the SI PLF group, and 0.8±1.0 in the LLIF group (p=0.041). Oswestry Disability Index and the Euro-QoL 5 dimension visual analogue scale scores also showed greater improvements in the LLIF group than in the SI PLF group at postoperative 1 year (p=0.003, 0.016).
Sagittal balance (SB) has become a major concern in the treatment of degenerative spine disease.1 However, the impact of SB in the surgical treatment of degenerative spinal disease is still controversial.234 Nevertheless, the development and utilization of new minimally invasive lateral approach lumbar fusion techniques, including lateral lumbar interbody fusion (LLIF), has made it much easier to improve correction of postoperative spinal SB.56 We hypothesized that corrected spine balance in patients with symptomatic lumbar spinal stenosis (LSS) might affect surgical outcomes in terms of both functional mobility tests reflecting the risk of falling and quality of life. Therefore, our objectives in the current investigation were to assess postoperative changes in the risk of falling and quality of life in patients with LSS after SB corrective surgery. We compared minimally invasive LLIF combined with posterior surgery with classical decompression and postero-lateral fusion (PLF) surgery according to whole spinal SB status.
This study was approved by the Institutional Review Board of the authors' hospital (IRB No. 4-2011-0399). From November 2011 to March 2015, 76 patients who underwent LLIF surgery [combined with posterior surgery using a conventional pedicular screw-rod system and cages for lateral interbody fusion and posterior lumbar interbody fusion (Medtronic Sofamor Danek, Inc., Memphis, TN, USA)] were enrolled in prospective single cohort manner and matched retrospectively. All patients whose conservative treatment for LSS had failed were recommended to undergo decompression and additional fusion surgery when LSS was accompanied by segmental instability and/or severe stenosis with leg symptoms in which facet joints could be resected more than 75% unilaterally or 50% bilaterally during surgery.789 Among 76 patients, patients with other conditions that hampered their functional performance, including neuropathological and other neurodegenerative conditions, such as Parkinson's disease, Alzheimer's disease, or a specific ataxic condition, were excluded.1011 Furthermore, patients with severe osteoarthropathic conditions causing knee and hip joint contractures that affected the entire spinal SB were also excluded.12 In addition, severe coronally imbalanced patents with a local Cobb angle larger than 10 degrees of degenerative scoliosis were also excluded to remove possible confounding factors affecting SB status. Finally, 56 patients in the LLIF surgery group who completed 3 months and 1 year follow-up comprised the LLIF group.
Standard, full-length, 36-inch lateral radiographs of the spine were taken in a conventional standardized manner13 and used to evaluate whole spinal SB. The C7 plumb line was placed over the center of the vertebral body and its distance from the postero-superior corner of S1 was measured and defined as C7-plumb line-distance (C7PL). An offset of larger than 2.5 cm anteriorly or posteriorly was considered to indicate sagittal imbalance.14
Different components, such as thoracic kyphosis (TK) and lumbar lordosis (LL) were recorded, and pelvic incidence (PI), pelvic tilt (PT), and sacral slope (SS) angles were used to describe the shape and orientation of the pelvis.15
All patients in the LLIF group, who were enrolled consecutively, had a sagittally imbalanced spine. Based on age, gender, body mass index, sagittal profiles, operated spine level, and operation length of the LLIF group, each of the 56 patients were retrospectively matched and compared with prospectively enrolled patients who underwent decompression and PLF surgery at the authors' institute (Fig. 1). A total of 168 patients (36 men, 132 women) in three groups were followed-up for at least 1 year postoperatively.
Major diagnoses were spinal stenosis (124 patients) and spinal stenosis with spondylolisthesis (44 patients). All patients were treated with decompression, which included laminectomy, total facetectomy, and additional discectomy if necessary, and posteriorly instrumented PLF surgery or LLIF using local autologous and allo-chip bone mixing with demineralized bone matrix grafts. All surgeries were performed by two surgeons regardless of surgery type. A failure of fusion with non-union in the PLF group and in the LLIF groups were investigated on follow-up radiographs and a CT scan based on suggested criteria.1617
Walking distance in a single trial, the Oswestry Disability Index (ODI), the Euro-QoL 5 dimension (EQ-5D), and Euro-QoL-visual analogue scale (VAS) were recorded181920 at the initial preoperative evaluation and at 3 months and 1 year postoperatively.
Other basic demographic data were also gathered, including hip osteoarthritis and knee osteoarthritis using the Kellgren-Lawrence scale,21 and total hip/knee replacement status. Furthermore, the presence of osteoporotic vertebral compression fractures was evaluated based on conventional thoraco-lumbar lateral radiographs using an established visual semi-quantitative system22 in all enrolled patients. Osteoporosis of the lumbar spine area was also measured by dual energy X-ray absorptiometry using a GE-lunar densitometer (Lunar Prodigy, GE Lunar Corp., Madison, WI, USA).
To evaluate the risk of falling, four functional mobility tests were used: the alternate-step test (AST), the six-meter-walk test (SMT), the sit-to-stand test (STS), and the timed up and go test (TUGT).102324
Additionally, a fall diary was given to all patients or caregivers who were encouraged to record every fall and report it when they visited the outpatient clinic for regular follow-up at 3 months and 1 year postoperatively.
The basic steps were the same as in the LLIF procedure and were designed to protect the psoas muscle by full posterior retraction during the procedure.25 However, six-degree lordotic angled cages (Clydesdale® PEEK, Medtronic Sofamor Danek, Inc., Memphis, TN, USA) (preferentially 12–14 mm in height) were inserted within the anterior one-third portion of the vertebral body to enhance correction of the lordotic angle. The demineralized bone matrix and allo-chip bone mixture was used and packed into the cage. To enhance the fusion process, we employed our own technique to create linear breakage of end-plates along the line of expected cage insertion position with a straight 1/4-inch osteotome, after full endplate preparation. For cases in which the LLIF procedure was difficult due to iliac vascular bifurcation variants that crossed the entry point into L5-S1 disc space, posterior lumbar interbody fusion was carried out instead using bulleted tipped convex-shaped cages (Capstone® PEEK, Medtronic Sofamor Danek, Inc., Memphis, TN, USA). In 10 cases of posterior lumbar interbody fusion, cages were also placed into the anterior one-third portion of the vertebral body. During posterior procedures, decompression surgery, which included total facetectomy, laminectomy, and additional discectomy/foraminotomy, was performed. Compression forces between the conventional pedicle screws were applied during rod assembly to ensure greater lordosis as well as more contact between the vertebral body and inserted cages during the procedure. Also, unilateral PLF over the whole surgery level was added for the sake of non-union of LLIF level.
Basic statistical analyses, including the ANOVA and chi-square tests, were used to evaluate the statistical significance of differences between SB PLF, SI PLF, and LLIF groups in terms of QOL, the four functional mobility tests, actual falls, and other demographic data. Post-hoc analysis by the Bonferroni method was also used to confirm statistical differences between groups. A forward stepwise multiple linear regression analysis was also used to evaluate if radiologic parameters were significantly related to ODI and EQ-VAS scores at each follow-up. All statistical analyses were performed using the SPSS 19.0 statistics package (IBM Corp., Armonk, NY, USA). p-values less than 0.05 were considered statistically significant.
The mean patient age was 70.6 years in the SB PLF group (range 61–83 years), 71.4 years in the SI PLF group (range 55–80 years), and 70.3 years in the LLIF group (range 60–85 years) (not significant, ANOVA). Other demographic comparisons are shown in Table 1.
Perioperatively, two cases of hip flexor weakness and one case of postoperative hematoma around the retracted psoas muscle area were encountered in the LLIF group. Also, one case of dural tear and two case of perioperative pneumonia were observed in the whole PLF group. Fortunately, all perioperative complications were resolved without perioperative mortality.
In the SB PLF group, the mean C7PL was 6.2±13.6 mm preoperatively, 14.1±15.5 mm at 3 months postoperatively, and 19.4±22.2 mm at 1 year postoperatively (p=0.007, ANOVA). In the SI PLF group, the mean C7PL was 72.9±33.8 mm preoperatively, 73.8±42.5 mm at 3 months postoperatively, and 79.9±48.5 mm at 1 year postoperatively (p=0.754, ANOVA). In the LLIF group, the mean C7PL was 74.8±38.2 mm preoperatively, 27.6±19.8 mm at 3 months postoperatively, and 31.7±17.2 mm at 1 year postoperatively (p=0.000, ANOVA).
Values of these measures and comparisons between SB PLF, SI PLF, and LLIF groups are presented in Fig. 2 and Table 2.
In post-hoc analysis by the Bonferroni method, preoperative C7PL, LL, and PI-LL in the SB PLF group demonstrated significant differences, compared with those in the SI PLF and LLIF groups (p=0.000, 0.000, 0.000). At 3 months and 1 year postoperatively, C7PL, LL, and PI-LL differed significantly in the SI PLF group, compared with those in the SB PLF and LLIF groups (p=0.000, 0.000, 0.002 for 3 months, p=0.000, 0.000, 0.012 for 1 year).
Radiological non-union and adjacent segmental failure was negligible in the three groups (one case in the SB PLF, 3 cases in the SI PLF groups, and no cases in the LLIF group) up to 1 year postoperative follow-up.
In the SB PLF group, All four functional tests improved significantly in comparison to preoperative abilities (p=0.025 for AST, p=0.000 for SMT, p=0.000 for STS, p=0.000 for TUGT, ANOVA) (Fig. 3). In the SI PLF group, only the SMT and STS tests showed significant improvement during the postoperative follow-up period (p=0.021 for SMT, 0.001 for STS, ANOVA). In the LLIF group, all four functional tests improved significantly in comparison to preoperative abilities (p=0.000 for AST, p=0.003 for SMT, 0.000 for STS, p=0.000 for TUGT, ANOVA). The difference between postoperative and preoperative values of the four functional tests of each group are shown in the Table 3.
The average number of actual falls per patient during the follow-up period was 0.4±0.7 in the SB PLF group, 1.1±1.4 in the SI PLF group, and 0.8±1.0 in the LLIF group (p=0.041, ANOVA). In the post-hoc analysis, the SI PLF group demonstrated significantly more falls than the SB PLF group. During follow-up, two patients in the SI PLF group fell down and suffered intertrochanteric fractures; they both underwent hip surgery as treatment.
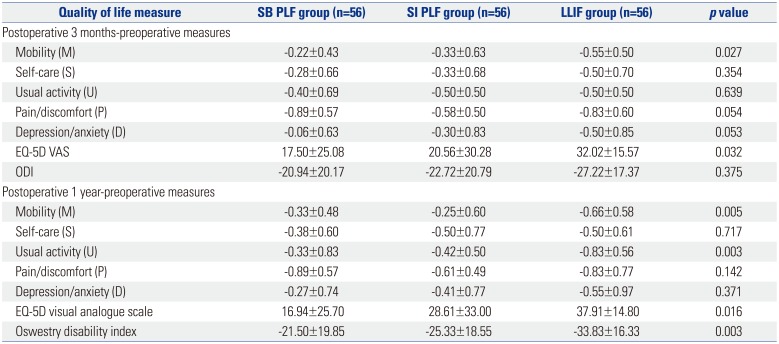
The mean EQ-5D VAS for general health status and mean ODI in the SB PLF, SI PLF and LLIF groups were improved significantly during follow-up, compared to preoperative values (p=0.002, 0.000 for SB PLF group, p=0.000, 0.000 for SI PLF group, p=0.000, 0.000 for LLIF group, ANOVA) (Fig. 4). Each parameter, except the D dimension in the EQ-5D scale (p=0.230), improved significantly postoperative in the SI PLF group (p=0.012 for M, p=0.000 for S, U and P, ANOVA). However, in the SB PLF and LLIF groups, all dimensions demonstrated statistically significant improvement after surgery (In the SB PLF group, p=0.009 for mobility (M), p=0.001 for self-care (S), p=0.020 for usual activity (U), p=0.000 for pain/discomfort (P), and p=0.043 for depression/anxiety (D), ANOVA) (In the LLIF group, p=0.000 for M, S, U, P, and D, ANOVA). The comparative results of postoperative improvement among three groups are presented in Table 4.
In a correlation analysis between the radiologic parameters, including PI-LL mismatch (PI-LL≤10 versus >10), EQ-VAS, and ODI, only C7PL correlated with ODI and EQ-VAS at preoperative and postoperative measurement (p=0.000, multiple regression). Other radiologic parameters did not correlate with EQ-VAS or ODI.
Minimally invasive lateral lumbar interbody fusion procedures are very effective at simultaneously restoring sagittal and coronal balance.52627 From this, it is expected that recovered SB after lateral fusion procedures could favorably affect fall risk. Indeed, poor postoperative spinal sagittal alignment is related to body imbalance, which may account for the association between poor spinal sagittal alignment and falls.2829 In this study, we included patients who underwent posterolateral fusion surgery along with decompressive surgery for LSS. These patients were set as the control group against the LLIF group, as PLF alone does not change the SB-related parameters postoperatively.29
In many papers related to SI, the suggested values differ from 2.5 cm to 7.0 cm, depending on the compensatory mechanism, age, and presence of symptom.14303132 A guideline for choosing corrective surgery for adult spinal deformity33 were observed in our SI PLF and LLIF groups (PT, 22.3±7.1° and 26.6±9.9°; C7PL, 72.9±33.8 mm and 74.8±38.2 mm; PI-LL, 22.8±15.7° and 29.6±19.3°; and preoperative ODI, 61.7±15.9 and 58.2±14.8). However, one group of patients only underwent decompression and posterolateral fusion surgery. The LLIF group underwent a minimally invasive anterolateral interbody fusion surgery, enabling an increased improvement in SB, similar to extensive corrective surgeries such as Smith-Peterson and pedicle-subtraction osteotomy.34 Compared with other direct lateral interbody fusion and LLIF related studies,2535 our case series had a larger lordotic correction, because of strategic positioning of the cage into the anterior 1/3 space of the vertebral body nearest to the anterior longitudinal ligament and additional posterior compression force during rod assembly after total facetectomy.
Presumably based on LSS pathophysiology, it is thought that there must be additional surgical corrective effects on the compensatory flexed posture to increase the spinal canal diameter, which adversely affects SB,36 along with restoration of LL using a 6-degree angled cage during LLIF.35
Our study was unique in its analysis of actual falls and functional mobility tests as a means of evaluating functional outcomes along with quality of life (QOL) after correction of SB. This is in contrast to other studies, which have mainly focused on radiologic parameters or employed extensive corrective surgery.23437 In the present study, changes in postoperative SB and related outcomes depending on surgery type were demonstrated to have significant differences in both radiological and clinical parameters of functional mobility tests (reflecting fall risk) and actual falls as recorded in a fall diary. In all three groups, most patients achieved improvement in their QOL and functional outcome. However, the noted improvement was much greater in the LLIF group than the SI PLF group, but to a lesser extent, compared to the reference value in the SB PLF group.
In the four functional mobility tests, LLIF patients demonstrated the worst preoperative measures; however, these patients also demonstrated the most postoperative improvement compared to the SI PLF group, especially in the AST and STS tests, which reflects function during destabilizing activities in the sagittal plane, such as bending forward and standing on one leg while stepping up and down.38 The other functional mobility tests focused on alternative characteristics, as multiple confounding factors makes it difficult to confirm a difference between groups.
In part, the limited improvement of functional mobility in the LLIF group could be explained by the fact that individuals who present with a long duration of considerable sagittal imbalance often also have atrophy of the spinal extensor muscles,3940 which plays a major role in the posturing and balancing activities in older adults.28 Although correction of LL and other sagittal parameters were achieved after LLIF procedures, the function and action of back muscles remained weakened and even worsened by surgical trauma and the presence of spinal implants. Therefore, although postoperative improvement of SB resulted in improved posture, the function of the back muscles was not recovered to the extent necessary for true functional improvement in the four mobility tests. Also, the newly fixed spine likely requires time to adapt to its new lumbar curve and proprioception after surgery.41 This could be confirmed by serial improvement between 3 months and 1 year postoperative in terms of EQ-5D measure and the 4 mobility test results.
The number of actual falls during postoperative follow-up was also shown to be statistically different between groups. Compared with the SI PLF group, the LLIF group had similar radiologic parameters and worse functionality preoperatively, but better radiologic values, functional results, and less falls postoperatively during follow-up. This supports our hypothesis that SI reduces energy efficiency and necessitates more time on behalf of the patient to complete stability tests. All groups demonstrated better functional test results postoperatively, although the improvement in the SI PLF group was still worst among the three groups. However, the LLIF groups demonstrated considerable improvement to reach a similar level as the SB PLF group.
In all patients, the number of actual falls was more frequent than was expected. One possible reason is lifestyle, including activities necessitating repetitive squatting and standing up from the ground. Even though preoperative and postoperative education was provided to patients and caregivers, some still continue their preoperative lifestyle after discharge. In our next study, we are planning to investigate the effect of floor activities on the postoperative risk of falling compared with the western lifestyle.
Our study had several limitations. First, we did not perform a head-to-toe evaluation on a single radiograph, as is done in the EOS imaging system.32 However, as part of our exclusion criteria, based on physical exams and whole lower extremity radiographs, we excluded patients with hip or knee contractures or pathologic conditions that may affect global sagittal alignment.12 Second, all efforts were given to match enrolled patients in terms of age, sagittal profile, and surgery level; however, there were inevitable differences in the preoperative baseline in terms of functional mobility and QOL between the groups. Third, with only 1-year follow up, it is difficult to comment on adjacent segment disease in all three groups. As of now, we are gathering the 5-year long-term follow-up data for our next topic. We would like to stress that the purpose of this study was to evaluate the actual falls and improvement of fallrelated functional tests after correctional surgery using minimally invasive lateral interbody fusion surgery plus posterior surgery.
Despite these limitations, this was the first study to analyze outcomes, determined by functional mobility, actual falls, and QOL, of minimally invasive surgery to treat LSS with an emphasis on achieving SB. We found that LLIF patients showed greater improvement in functional mobility and experienced less falls during follow-up than did patients in the SI PLF group.
Accordingly, consideration of SI in patients with LSS and its surgical correction, using combined minimally invasive LLIF and posterior surgery, is encouraged to attain better surgical and functional outcomes and to decrease the incidence of actual falls after treatment than when PLF surgery is performed.
ACKNOWLEDGEMENTS
This study was partially supported by Catholic-Kwandong University Research fund (CKURF-2016-0484-0001). This study was mainly performed in the Severance Hospital and Gangnam Severance Hospital, College of Medicine, Yonsei University.
References
1. Berven SH, Deviren V, Smith JA, Hu SH, Bradford DS. Management of fixed sagittal plane deformity: outcome of combined anterior and posterior surgery. Spine (Phila Pa 1976). 2003; 28:1710–1715. PMID: 12897497.

2. Bayerl SH, Pohlmann F, Finger T, Onken J, Franke J, Czabanka M, et al. The sagittal balance does not influence the 1 year clinical outcome of patients with lumbar spinal stenosis without obvious instability after microsurgical decompression. Spine (Phila Pa 1976). 2015; 40:1014–1021. PMID: 25893354.

3. Hikata T, Watanabe K, Fujita N, Iwanami A, Hosogane N, Ishii K, et al. Impact of sagittal spinopelvic alignment on clinical outcomes after decompression surgery for lumbar spinal canal stenosis without coronal imbalance. J Neurosurg Spine. 2015; 23:451–458. PMID: 26140404.

4. Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2002; 27:59–64. PMID: 11805637.

5. Costanzo G, Zoccali C, Maykowski P, Walter CM, Skoch J, Baaj AA. The role of minimally invasive lateral lumbar interbody fusion in sagittal balance correction and spinal deformity. Eur Spine J. 2014; 23(Suppl 6):699–704. PMID: 25217242.

6. Kotwal S, Kawaguchi S, Lebl D, Hughes A, Huang R, Sama A, et al. Minimally invasive lateral lumbar interbody fusion: clinical and radiographic outcome at a minimum 2-year follow-up. J Spinal Disord Tech. 2015; 28:119–125. PMID: 22964885.
7. Resnick DK, Watters WC 3rd, Mummaneni PV, Dailey AT, Choudhri TF, Eck JC, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 10: lumbar fusion for stenosis without spondylolisthesis. J Neurosurg Spine. 2014; 21:62–66. PMID: 24980587.

8. Resnick DK, Watters WC 3rd, Sharan A, Mummaneni PV, Dailey AT, Wang JC, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: lumbar fusion for stenosis with spondylolisthesis. J Neurosurg Spine. 2014; 21:54–61. PMID: 24980586.

9. Rampersaud YR, Ravi B, Lewis SJ, Stas V, Barron R, Davey R, et al. Assessment of health-related quality of life after surgical treatment of focal symptomatic spinal stenosis compared with osteoarthritis of the hip or knee. Spine J. 2008; 8:296–304. PMID: 17669690.

10. Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008; 37:430–435. PMID: 18487264.

11. Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, et al. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011; 364:1218–1229. PMID: 21449785.

12. Lee SM, Yoon MG, Moon MS, Lee BJ, Lee SR, Seo YH. Effect of correction of the contractured flexed osteoarthritic knee on the sagittal alignment by total replacement. Asian Spine J. 2013; 7:204–211. PMID: 24066216.

13. Morvan G, Mathieu P, Vuillemin V, Guerini H, Bossard P, Zeitoun F, et al. Standardized way for imaging of the sagittal spinal balance. Eur Spine J. 2011; 20(Suppl 5):602–608. PMID: 21830081.

14. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976). 1994; 19:1611–1618. PMID: 7939998.
15. Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998; 7:99–103. PMID: 9629932.

16. Tsutsumimoto T, Shimogata M, Yoshimura Y, Misawa H. Union versus nonunion after posterolateral lumbar fusion: a comparison of long-term surgical outcomes in patients with degenerative lumbar spondylolisthesis. Eur Spine J. 2008; 17:1107–1112. PMID: 18536941.

17. Williams AL, Gornet MF, Burkus JK. CT evaluation of lumbar interbody fusion: current concepts. AJNR Am J Neuroradiol. 2005; 26:2057–2066. PMID: 16155160.
18. Solberg TK, Olsen JA, Ingebrigtsen T, Hofoss D, Nygaard OP. Health-related quality of life assessment by the EuroQol-5D can provide cost-utility data in the field of low-back surgery. Eur Spine J. 2005; 14:1000–1007. PMID: 15843969.

19. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000; 25:2940–2952. PMID: 11074683.

20. Lee BH, Yang JH, Lee HM, Park JY, Park SE, Moon SH. Surgical outcome predictor in degenerative lumbar spinal disease based on health related quality of life using euro-quality 5 dimensions analysis. Yonsei Med J. 2016; 57:1214–1221. PMID: 27401654.

22. Binkley N, Krueger D, Gangnon R, Genant HK, Drezner MK. Lateral vertebral assessment: a valuable technique to detect clinically significant vertebral fractures. Osteoporos Int. 2005; 16:1513–1518. PMID: 15834512.

23. Kim HJ, Chun HJ, Han CD, Moon SH, Kang KT, Kim HS, et al. The risk assessment of a fall in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). 2011; 36:E588–E592. PMID: 21242866.

24. Lee BH, Kim TH, Park MS, Lim S, Park JO, Kim HS, et al. Comparison of effects of nonoperative treatment and decompression surgery on risk of patients with lumbar spinal stenosis falling: evaluation with functional mobility tests. J Bone Joint Surg Am. 2014; 96:e110. PMID: 24990984.
25. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kishida S, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lateral interbody fusion for lumbar spinal degeneration disease. Yonsei Med J. 2015; 56:1051–1059. PMID: 26069130.

26. Baghdadi YM, Larson AN, Dekutoski MB, Cui Q, Sebastian AS, Armitage BM, et al. Sagittal balance and spinopelvic parameters after lateral lumbar interbody fusion for degenerative scoliosis: a case-control study. Spine (Phila Pa 1976). 2014; 39:E166–E173. PMID: 24150436.
27. Phan K, Rao PJ, Scherman DB, Dandie G, Mobbs RJ. Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci. 2015; 22:1714–1721. PMID: 26190218.

28. Imagama S, Ito Z, Wakao N, Seki T, Hirano K, Muramoto A, et al. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J. 2013; 22:1346–1353. PMID: 23443680.

29. Lee BH, Park JO, Kim HS, Suk KS, Lee SY, Lee HM, et al. Spinal sagittal balance status affects postoperative actual falls and quality of life after decompression and fusion in-situ surgery in patients with lumbar spinal stenosis. Clin Neurol Neurosurg. 2016; 148:52–59. PMID: 27398622.

30. Jean L. Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J. 2014; 23:1394–1399. PMID: 24509774.

31. Lamartina C, Berjano P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J. 2014; 23:1177–1189. PMID: 24682355.

32. Diebo BG, Ferrero E, Lafage R, Challier V, Liabaud B, Liu S, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine (Phila Pa 1976). 2015; 40:642–649. PMID: 25705962.
33. Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013; 38:E803–E812. PMID: 23722572.
34. Bao H, He S, Liu Z, Zhu Z, Qiu Y, Zhu F. Will immediate postoperative imbalance improve in patients with thoracolumbar/lumbar degenerative kyphoscoliosis? A comparison between Smith-Petersen osteotomy and pedicle subtraction osteotomy with an average 4 years of follow-up. Spine (Phila Pa 1976). 2015; 40:E293–E300. PMID: 25901984.

35. Kim SJ, Lee YS, Kim YB, Park SW, Hung VT. Clinical and radiological outcomes of a new cage for direct lateral lumbar interbody fusion. Korean J Spine. 2014; 11:145–151. PMID: 25346760.

36. Katz JN, Dalgas M, Stucki G, Katz NP, Bayley J, Fossel AH, et al. Degenerative lumbar spinal stenosis. Diagnostic value of the history and physical examination. Arthritis Rheum. 1995; 38:1236–1241. PMID: 7575718.

37. Koller H, Pfanz C, Meier O, Hitzl W, Mayer M, Bullmann V, et al. Factors influencing radiographic and clinical outcomes in adult scoliosis surgery: a study of 448 European patients. Eur Spine J. 2016; 25:532–548. PMID: 25917822.

38. Chung MM, Chan RW, Fung YK, Fong SS, Lam SS, Lai CW, et al. Reliability and validity of Alternate Step Test times in subjects with chronic stroke. J Rehabil Med. 2014; 46:969–974. PMID: 25167536.

39. Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011; 20(Suppl 5):626–633. PMID: 21796393.

40. Nam WD, Chang BS, Lee CK, Cho JH. Clinical and radiological predictive factors to be related with the degree of lumbar back muscle degeneration: difference by gender. Clin Orthop Surg. 2014; 6:318–323. PMID: 25177458.

41. Hobbs AJ, Adams RD, Shirley D, Hillier TM. Comparison of lumbar proprioception as measured in unrestrained standing in individuals with disc replacement, with low back pain, and without low back pain. J Orthop Sports Phys Ther. 2010; 40:439–446. PMID: 20592482.

Fig. 1
Enrollment and follow-up of the study participants. SB, sagittal balance; SI, sagittal imbalance; PLF, postero-lateral fusion; LLIF, lateral lumbar interbody fusion; LSS, lumbar spinl stenosis; EQ-5D, Euro-QoL 5 dimension.
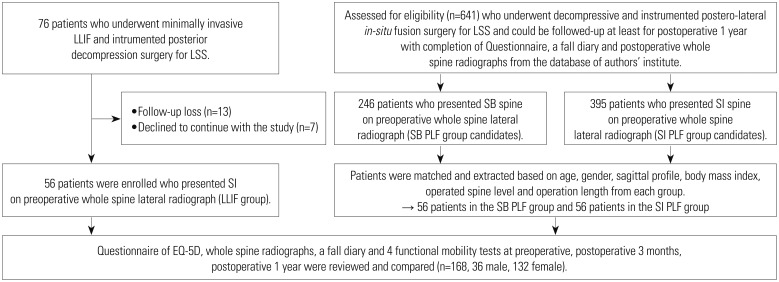
Fig. 2
Comparison of pre- and postoperative sagittal balance status depending on surgical treatment. Both (A) sagittal balance PLF patient and (B) sagittal imbalance PLF patient demonstrated no change on the sagittal profile postoperatively. However (C) sagittal imbalnce LLIF patient presented with considerable change of lumbar lordosis and other sagittal profiles after surgery. PLF, postero-lateral fusion; LLIF, lateral lumbar interbody fusion.
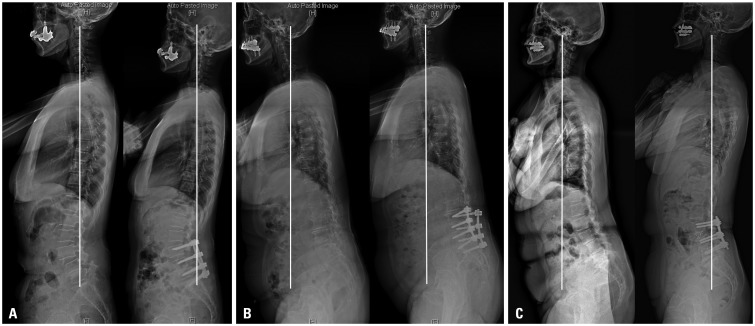
Fig. 3
Postoperative changes in functional mobility test results, reflecting risk of falling in the SB PLF group, SI PLF group, and LLIF group (unit: seconds). In the post-hoc analysis, the Bonferroni method was utilized to demonstrate statistical differences between groups for each measure. *p<0.05. AST, alternate-step test; SMT, six-meter-walk test; STS, sit-to-stand test; TUGT, timed-up-and-go test; SB, sagittal balance; SI, sagittal imbalance; LLIF, lateral lumbar interbody fusion; PLF, postero-lateral fusion.

Fig. 4
Postoperative changes in the values of the EQ-5D questionnaire, EQ-VAS, and ODI in the SB PLF group, SI PLF group, and LLIF group. SB, sagittal balance; SI, sagittal imbalance; PLF, postero-lateral fusion; LLIF, lateral lumbar interbody fusion; EQ-5D, Euro-QoL 5-dimension; VAS, visual analogue scale; ODI, oswestry disability index.
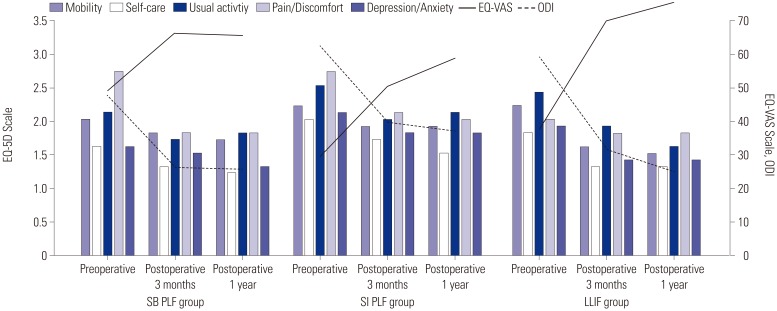
Table 1
Comparison of Demographic Characteristics between the Three Patient Groups
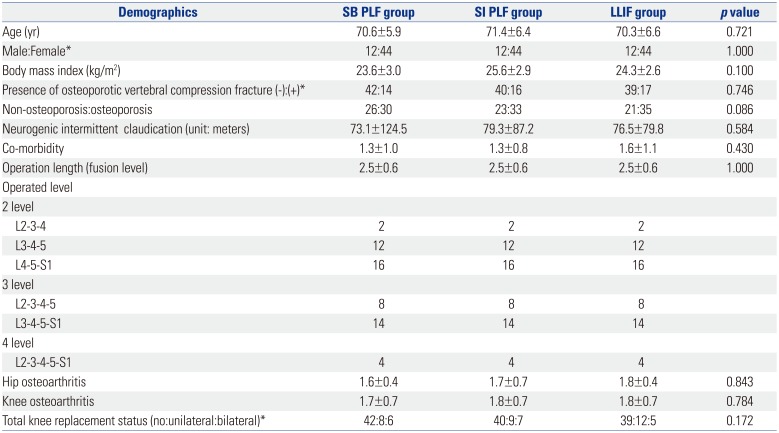
Table 2
Comparison of Radiologic Parameters between the Three Patient Groups
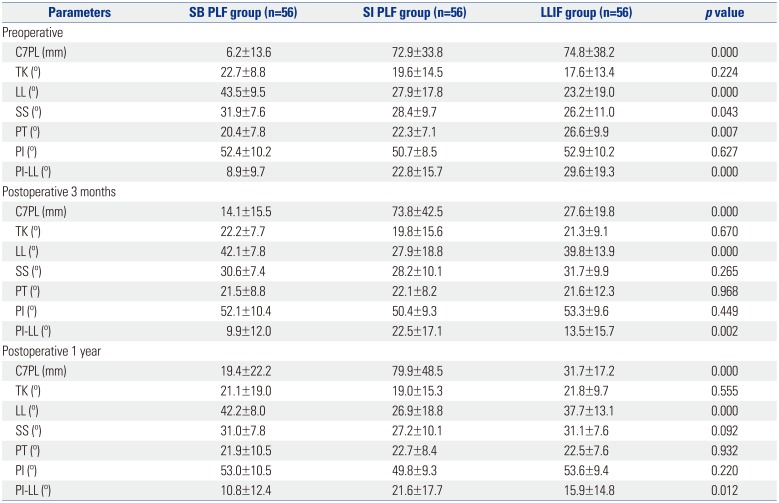
Table 3
Comparison of Differences between Postoperative and Preoperative Values in Four Functional Mobility Tests and Actual Falls
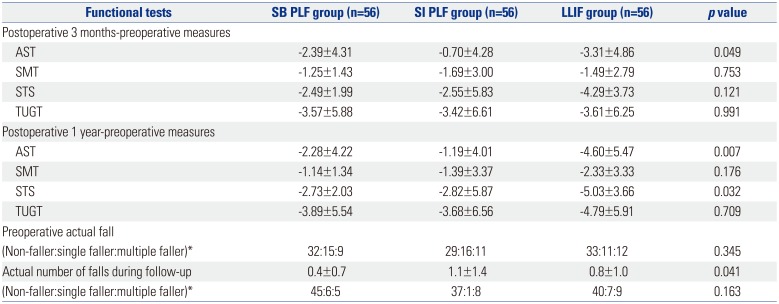
Table 4
Comparison of Postoperative Improvement in Quality of Life Parameters between the Three Patient Groups




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download