Abstract
Purpose
In childhood cancer survivors, the most common late effect is thyroid dysfunction, most notably subclinical hypothyroidism (SCH). Our study evaluated the risk factors for persistent SCH in survivors.
Materials and Methods
Survivors (n=423) were defined as patients who survived at least 2 years after cancer treatment completion. Thyroid function was assessed at this time and several years thereafter. Two groups of survivors with SCH were compared: those who regained normal thyroid function during the follow-up period (normalized group) and those who did not (persistent group).
Results
Overall, 104 of the 423 survivors had SCH. SCH was observed in 26% of brain or nasopharyngeal cancer survivors (11 of 43) and 21.6% of leukemia survivors (35 of 162). Sixty-two survivors regained normal thyroid function, 30 remained as persistent SCH, and 12 were lost to follow-up. The follow-up duration was 4.03 (2.15–5.78) years. Brain or nasopharyngeal cancer and Hodgkin disease were more common in the persistent group than in the normalized group (p=0.002). More patients in the persistent group received radiation (p=0.008). Radiation to the head region was higher in this group (2394±2469 cGy) than in the normalized group (894±1591 cGy; p=0.003). On multivariable analysis, lymphoma (p=0.011), brain or nasopharyngeal cancer (p=0.039), and head radiation dose ≥1800 cGy (p=0.039) were significant risk factors for persistent SCH.
Improved treatment modalities for childhood cancers have increased 5-year survival rates to nearly 80%.12 However, complications may arise later in the lives of childhood cancer survivors who received cytotoxic drugs, radiation, or other treatments. Due to the increasing number of long-term survivors, these late effects have become an important issue in childhood cancer management.3 Endocrine-related late effects are commonly reported, of which thyroid disorders are the most frequent.4
Thyroid hormones play an important role in growth and development during childhood. The thyroid is especially radiosensitive, and irradiation of the neck, head, or brain can cause thyroid dysfunction.45 Recent reports demonstrate that childhood cancer survivors who received total body irradiation, mantle irradiation for Hodgkin disease (HD), craniospinal irradiation for brain tumors, or other conditioning regimens are at risk for thyroid disease.456
The most common thyroid disease of childhood cancer survivors is hypothyroidism.57 There are two types of hypothyroidism, characterized as follows: primary hypothyroidism, with elevated levels of serum thyroid-stimulating hormone (TSH); and secondary or central hypothyroidism, with reduced levels of circulating TSH. Primary hypothyroidism can be overt [reduced levels of free thyroxine (fT4) and triiodothyronine (T3)] or subclinical (normal fT4 and T3 levels). In central hypothyroidism, the reduced thyroid hormone levels result from inadequate stimulation of the thyroid gland due to reduced TSH in cases where hypothalamic-pituitary disturbance is present.8910 Overt hypothyroidism is usually treated via daily administration of thyroxine pills,8910 and the distinction between it and subclinical hypothyroidism (SCH) is determined via biochemical measurement of fT4 and T3 concentrations in serum. There is no standard management for patients with SCH and mildly high serum TSH concentrations, although treatment of patients with concentrations of 10 mU/L or more is recommended.8910
Pediatric endocrinologists are undecided as to how to treat children with SCH, as controlled pediatric SCH studies are rare. Two recent studies reported that untreated patients with SCH had normal TSH levels at follow-up.1011 However, elucidation of the natural history of SCH as a late effect in childhood cancer survivors is lacking, despite its frequent occurrence in such survivors.1213
The aim of this study was to determine which children are at risk for persistent SCH after cancer treatment and who therefore should be treated early during the follow-up period.
Starting in 2005, we established a long-term follow-up clinic at the Yonsei Cancer Center, Yonsei University Health System, Korea to evaluate cancer survivors once or twice a year.7 In accordance with published guidelines, survivors were defined as individuals with no evidence of cancer for 2 or more years after the completion of cancer treatment.14 Among the more than 700 registered survivors in the clinic, 423 had been tested for thyroid function, and seven showed hyperthyroidism (three overt and four subclinical) at 2 years after cancer treatment. The remainder (n=416) included survivors of leukemia (162, 38.9%); non-Hodgkin lymphoma (NHL; 47, 11.3%); HD (12, 2.9%); brain or nasopharyngeal cancer (brain/naso; 43, 10.3%); Wilms tumor (WT), neuroblastoma (NB), or abdominal malignancies including hepatoblastoma (WT/NB/abdomen; 79, 19.0%); and sarcoma or other non-abdominal malignancies (sarcoma/others; 73, 17.5%). Two years after completion of cancer treatment, 300 survivors (72.1%) had normal thyroid function, 12 (2.9%) had overt hypothyroidism, and 104 (25.0%) had SCH. Twelve of the survivors with SCH were lost to follow-up; therefore, 92 survivors with SCH were ultimately included in this study. This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System (4-2015-0016).
Serum T3, fT4, and TSH levels were monitored in the survivors; the reference values were 80–200 ng/dL, 0.95–2.23 ng/dL, and 0.3–4.0 mU/L, respectively, as defined by our institution. SCH was defined as a condition in which TSH levels were higher than the reference value and T3 and T4 levels were within the range of the reference values. To detect thyroid disorders in survivors, the thyroid function test (TFT) was performed 2 years after cancer treatment completion as a baseline test.7 Survivors with no thyroid disease-related symptoms received no additional TFTs as routine surveillance to comply with the Korean health insurance policy. Survivors with abnormal thyroid function were followed-up annually or biannually. If thyroid function became normal, they were designated as "normalized." If it did not, they were designated as "persistent."
As recommended by an endocrinologist, thyroid hormone (levothyroxine) was prescribed for survivors whose TSH levels were >8–10 mU/L, with consideration of their clinical symptoms, signs, and developmental stage. Thyroid hormone replacement was tapered out after 6–12 months. If the TSH level increased after tapering or discontinuing the treatment, the treatment was reinitiated. Thyroid function was monitored every 1–2 years after short-term discontinuation of replacement therapy. If the therapy was permanently discontinued, the survivor was considered to be normalized.
The six cancer diagnosis groups were leukemia, NHL, HD, brain/naso, WT/NB/abdomen, and sarcoma/others. We reviewed the treatment modalities, including chemotherapy, radiation therapy, and hematopoietic stem cell transplantation (HSCT). The types of chemotherapeutic agents used were also reviewed, as were radiation body sites and doses. The total radiation dose per survivor was defined as the maximum total dose of radiation at a specific radiation site. If a survivor had received craniospinal irradiation long after prophylactic brain radiation, we summed the doses at each site and calculated the maximum dose for each site.
The time variables were as follows: age at diagnosis, age at cancer treatment completion, age at the initial TFT (the age at which thyroid function was first categorized after treatment completion), age at the final TFT, and follow-up period (time from the initial TFT to the final TFT).
Categorical variables including diagnoses and treatment modalities were evaluated by using the chi-square test or Fisher's exact test. Continuous variables including time variables and radiation doses were assessed by using Student's t-test or an analysis of variance for parametric tests and the Mann-Whitney U-test or Kruskal Wallis test for non-parametric tests. Paired variables were tested using the Wilcoxon signed rank test. The cumulative incidence of thyroid function normalization was assessed in each cancer diagnosis group by using a Kaplan-Meier analysis and the log-rank test. For the Kaplan-Meier analysis and regression analysis, diagnosis groups were categorized into three groups: brain/naso, lymphoma, and other tumors. Variables that were significant in a univariate analysis, including treatment modalities and age at diagnosis, were included in the multivariable model. We calculated the odds ratios using logistic regression after adjustment for the risk factors of persistent SCH including age, gender, HSCT, head radiation, neck radiation, and chemotherapeutic agents such as enzymes and epipodophyllotoxins. All statistical analyses were performed by using SPSS version 21 for Windows (SPSS Inc., Chicago, IL, USA).
Two years after cancer treatment completion, 116 of the 423 childhood cancer survivors initially surveyed (27.4%) had hypothyroidism; 112 (26.5%) had primary hypothyroidism, and four (0.94%) had secondary hypothyroidism. The four survivors with secondary hypothyroidism were brain tumor survivors, and all were cases of overt hypothyroidism. Eight of the 112 (7.1%) survivors with primary hypothyroidism had overt hypothyroidism, whereas 104 (92.9%) had SCH. Six of the eight (75%) survivors with overt hypothyroidism were brain tumor survivors (data not shown). The percentage of survivors with SCH was similar for all diagnoses (p=0.322, data not shown): leukemia, 35 of 162 (21.6%); NHL, 12 of 47 (25.5%); HD, 6 of 12 (50.0%); brain/naso, 11 of 43 (25.6%); WT/NB/abdomen, 23 of 79 (29.1%); and sarcoma/others, 17 of 73 (32.3%, data not shown).
Our findings showed that SCH was the most common thyroid hormone disturbance after cancer treatment (n=104). Owing to losses (n=12) during follow-up, our study group ultimately comprised 92 childhood cancer survivors with SCH; their characteristics are shown in Table 1. The number of male survivors was 61 (66.3%). The median ages at cancer diagnosis, cancer treatment completion, initial TFT, and final TFT were 3.97 (1.80–8.11), 6.00 (2.95–10.50), 9.75 (6.92–14.59), and 14.42 (10.82–19.15) years, respectively. The interval from completion of treatment to enrollment was 2.97 (2.33–4.95) years. The follow-up duration (initial TFT to final TFT) was 4.03 (2.15–5.78) years. The most common diagnosis was leukemia (n=32, 34.8%), followed by WT/NB/abdomen (n=21, 22.8%). Most survivors underwent chemotherapy (n=91, 98.9%), and 43 survivors received HSCT (46.7%).
Sixty-two survivors with SCH regained normal thyroid function more than 2 years after cancer treatment completion (the normalized group), whereas 30 did not (the persistent group). There were no differences in sex or any time variables (age at diagnosis or age at cancer treatment completion) between the normalized and persistent groups. There were, however, significant differences in terms of cancer type: leukemia (75.0%), WT/NB/abdomen (85.7%), and sarcoma/others (73.3%) were more common in the normalized group, whereas brain/naso (87.5%) and HD (66.7%) were more common in the persistent group. The fT4 levels were statistically similar in all survivors regardless of cancer type (p=0.176) (Table 2). TSH levels were significantly higher in survivors of brain/naso cancer than in survivors of the other cancer types (p=0.010). As for the treatment modality, fT4 was significantly higher in patients treated with HSCT than in those without HSCT (p=0.021), and fT4 was significantly lower in patients treated with radiation (p=0.044); however, the fT4 levels in all groups were within the normal range.
The initial TSH level was significantly higher in the persistent group than in the normalized group (7.71 mU/L vs. 4.86 mU/L; p=0.001 via Mann-Whitney U-test, data not shown). In the normalized group, the TSH level was significantly lower at the final follow-up than at the initial follow-up (2.88 mU/L vs. 4.86 mU/L; p<0.001 via Wilcoxon signed rank test) (Table 3). The fT4 level was significantly higher at the initial follow-up than at the final follow-up (1.18 ng/dL vs. 1.07 ng/dL; p=0.008 via Wilcoxon signed rank test); however, all were in the normal range. In the persistent group, the TSH level was also lower at the final follow-up than at the initial follow-up (4.70 mU/L vs. 7.71 mU/L; p<0.001 via Wilcoxon signed rank test).
In the persistent SCH group, 23 (76.7%) survivors received thyroid hormone replacement therapy. The mean TSH levels tended to be higher in the replacement group than in the non-replacement group, though not significant [8.79 (5.46–12.71) mU/L vs. 6.27 (4.90–7.12) mU/L; p=0.149 via Mann-Whitney U-test], and fT4 levels were not different [1.11 (0.95–1.28) ng/dL vs. 1.09 (0.94–1.20) ng/dL; p=0.756 via Mann-Whitney U-test, data not shown]. Survivors with good clinical status did not receive hormone replacement therapy, and their TSH level did not exceed 10 mU/L throughout the follow-up period.
More survivors treated with radiation than without radiation showed persistent SCH (21 of 48, 43.8% vs. 9 of 44, 20.5%; p=0.017); the numbers of survivors previously receiving HSCT (p=0.378) or chemotherapy (p=0.326) were similar in both groups (Table 1). There were no group differences in the types of chemotherapeutic agents used with two exceptions: more survivors showed normalized SCH when treated with enzyme (e.g., L-asparaginase) than those treated without enzyme [21 of 25 (84.0%) vs. 41 of 67 (61.2%); p=0.038], whereas epipodophyllotoxin usage tended to be higher in the persistent group [25 of 63 (38.1%) vs. 5 of 29 (20.7%); p=0.098] (Table 4).
Radiation doses to the head region were significantly higher in the persistent group (2394±2469 cGy) than in the normalized group (894±1591 cGy; p=0.003), as were doses to the spine region (1319±1603 cGy vs. 462±921 cGy; p=0.001) (Table 5). Sixteen of the 37 (43.2%) survivors who had received head radiation ≥1800 cGy still had SCH at the final follow-up. In contrast, all four survivors (100%) who had received head radiation of <1800 cGy returned to normal at the final follow-up (p=0.031, data not shown).
Radiation doses to the neck region were also higher in the persistent group than in the normalized group, although the difference was not significant (626±1468 cGy vs. 115±357 cGy; p=0.086) (Table 5). All of the four survivors who had received neck radiation ≥1500 cGy still showed SCH at the final follow-up. Seven of the nine survivors (77.8%) who had received neck radiation <1500 cGy recovered normal thyroid function (p=0.009, data not shown). The total radiation dose per survivor was higher in the persistent group than in the normalized group (2883±2304 cGy vs. 1266±1707 cGy; p=0.001) (Table 5).
The median interval from time of cancer treatment completion to time of normalization of thyroid function was 8.84 years (95% confidence interval, 7.10–10.58 years). When the survivors were split into three cancer type groups (brain tumor survivors, lymphoma survivors, and survivors of other cancers), there was a tendency of difference in the normalized proportion of SCH among the three groups (p=0.094) (Fig. 1). Brain tumor survivors did not regain normal thyroid function during the follow-up compared to the survivors in the other groups (p=0.039).
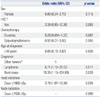
Lymphoma (odds ratio, 6.71; p=0.011), and brain/naso (odds ratio, 15.35; p=0.039) were significant risk factors for persistent SCH when compared to other tumors as a reference (Table 6). A head radiation dose of ≥1800 cGy was also a significant risk factor (odds ratio, 3.78; p=0.039). Sex, HSCT, type of chemotherapeutic agent, and neck radiation dose ≥1500 were not significant risk factors.
Primary hypothyroidism is caused by direct damage to the thyroid gland and is categorized as SCH or, if more severe, overt hypothyroidism. Central hypothyroidism is caused by damage to the hypothalamus-pituitary gland axis and can result in loss of endocrine function. In our study, SCH was the most common thyroid disease after treatment of childhood cancer (104 of 112 survivors, 92.9%). Development of SCH during the follow-up period was unrelated to the previous cancer type. However, the percentage of survivors who regained a euthyroid status differed according to cancer type and treatment. Our aim was to identify survivors at risk for persistent SCH and to suggest a watchful waiting strategy for the normalized group and an early therapy for the persistent group.
Diagnosis of SCH is based on laboratory findings. Most patients with SCH show no symptoms or signs. Some present with non-specific symptoms such as poor quality of life, anxiety, depression, fatigue, or constipation.15 The prevalence of SCH ranges from 1% to 12.4% in the general population.10 Other estimates are 4.3% (the National Health and Examination Survey III) and 5.4–17.3% (large studies of thyroid dysfunctions in Koreans 17 years of age or older).1617 Prevalence tends to increase as age increases.17 There are no studies on SCH prevalence in Korean children.
TSH levels return to normal in 15–65% of untreated individuals 1–6 years after one-time elevations1819 and in >50% of individuals with increased or decreased levels.19 However, a significant proportion of adult patients with SCH progress to overt hypothyroidism. The rate of progression to overt hypothyroidism was 1–4% per year in one study and 2.9% per 5 years in another.1519 In a prospective study with a mean observation time of 9 years, 30–50% of female patients with SCH developed overt hypothyroidism, depending on clinical risk factors.20
The clinical consequences of SCH are controversial. In a meta-analysis of 55287 subjects, the risk of coronary heart disease and mortality increased as TSH concentration increased.21 The hazard ratio in the meta-analysis was 1.89 (95% confidence interval, 1.28–2.80) at 10 mU/L TSH. Conversely, two prospective studies found no association between SCH and the outcomes of patients with cardiovascular disease.2223 Other consequences of SCH include non-alcoholic fatty liver disease24 and, although not observed in all studies, psychiatric manifestations such as depression, anxiety, and cognitive dysfunction.25
Endocrinologists recommend thyroid hormone replacement for patients with TSH concentrations of >10 mU/L and routine surveillance for patients with TSH concentrations of ≤10 mU/L.89 Replacement therapy is sometimes advised for people aged less than 65 years, as their cardiovascular risks are greater than those of people aged 65 years or more.15
SCH is less prevalent in children than in adults. Although insufficient, data thus far suggest that SCH occurs in 1.7–9.5% of otherwise normal children.10 The natural course of SCH in childhood has not been well studied. In a recent meta-analysis, only nine relevant studies could be evaluated,6 most of which included only a small number of subjects. An exception was a large-scale retrospective study conducted in Israel; however, most of its subjects had autoimmune thyroiditis.11 The rate of recovery in the meta-analysis was 21.9–50%, and progression to overt hypothyroidism was 0–28.8%.6 In the Israeli study, SCH prevalence was 3.3% (n=3938), and 70.1% of patients with SCH had normal TSH levels in subsequent tests.11
Thyroid dysfunction in childhood cancer survivors is a well-known late effect.3726 Primary hypothyroidism is the most common abnormal thyroid-related response to thyroid irradiation.4 Risk factors for hypothyroidism include neck, craniospinal, and total body irradiation34 yet apparently not chemotherapy.413 Compared with primary overt hypothyroidism, SCH in childhood cancer survivors is less understood. The percentage of long-term survivors of Hodgkin lymphoma (n=55) who develop SCH is 20%.
Data on the natural history of SCH in childhood cancer survivors are limited. A previous study showed impaired thyroid function in 24% of survivors (71 of 291) during a median follow-up period of 6.1 years13 yet did not address SCH status after this time. Ishiguro, et al.12 found that 26.5% of patients (39 of 147) who underwent bone marrow transplantation developed SCH. Their TSH levels decreased from the upper normal range 8 years after bone marrow transplantation to the mid to normal range thereafter. However, the proportion of patients who recovered from SCH was not presented.
In our study, 12 (2.8%) of the 423 childhood cancer survivors had overt hypothyroidism, mainly the brain/naso survivors. SCH was the most common thyroid dysfunction in the 423 survivors (104, 24.6%), as well as in the 123 survivors with thyroid abnormalities (104, 84.5%). Among the study cohort (n=92), 67.4% of patients with SCH regained normal thyroid function. This result is similar to those in other pediatric studies on patients with autoimmune disease or healthy thyroids.611 In our study, 60–85% of leukemia, NHL, and WT/NB/abdomen survivors regained normal thyroid function, whereas only 12.5–33.3% of brain/naso and HD survivors did so; this difference was significant (p=0.002) (Table 2). Although the proportion of leukemia survivors with SCH was substantial (21.6%, which was much higher than in a normal pediatric cohort), most exhibited normalized thyroid function at the final follow-up. The percentages of brain/naso survivors with SCH or overt hypothyroidism were 25.6% (11 of 43) and 20.9% (9 of 43), respectively; however, most of them did not recover a euthyroid status. Collectively, these data show that SCH is frequently found in childhood cancer survivors regardless of cancer type. Leukemia and WT/NB/abdomen survivors can be managed without further treatment, whereas brain/naso survivors should receive thyroid hormone replacement as soon as possible, even if they have SCH rather than overt hypothyroidism.
The risk factors for persistent SCH are similar to those for overt hypothyroidism as reported in previous studies.45 However, the data on the dose-volume effect for the development of SCH are generally lacking. Our multivariable analysis confirmed that brain/naso tumors, lymphoma, and head radiation doses ≥1800 cGy were all significant risk factors for SCH. Brain tumor survivors have an increased risk of endocrine, psychiatric, cognitive, neurological, and developmental disorders owing to previous radiotherapy.34 The threshold dose for pituitary-hypothalamus hypothyroidism was 5000 cGy in the studies on the cranial irradiation.272829 When the radiation dose to the pituitary gland was increased from 2000 to 4500 cGy, the risk of hypothyroidism increased from 9% to 52%.29 As for direct thyroid radiation, the thresholds are less clear; however, radiation doses greater than 3000–4000 cGy are generally accepted as a threshold.2930 Nevertheless, the threshold for SCH has not yet been established. A large study on the general health status of cancer survivors reported that exposure of the hypothalamuspituitary axis to ≥1800 cGy disrupted this axis in >50% of survivors.31 However, it regarded all physical and laboratory findings including growth, pubertal progress, menstrual history, insulin-like growth factor 1 (IGF-1), cortisol, estradiol, TSH, and fT4 by screening studies as outcome measurements and did not specify the kind, proportion, or severity of axis disruption.31 Therefore, the radiation dose for inducing SCH could not be confirmed. In this study, radiation exposure of 1800 cGy or more to the head region posed the risk of persistent SCH, and this dose was lower than the dose causing overt hypothyroidism.
Whether cancer survivors who develop SCH during follow-up should receive treatment is an unanswered question. Our study provides suggestions based on the presence of risk factors. However, it had several limitations. First, the study cohort was prospective, whereas the analysis was retrospective. Second, follow-ups regularly occurred every 6 months; however, several survivors were lost during follow-up. Third, the duration of the follow-up was 4.2 years, yet the range was variable. Fourth, certain cancer types had an insufficient number of survivors for analysis. Fifth, survivors with normal thyroid function at the initial follow-up did not receive additional TFTs in compliance with the Korean health insurance policy. Sixth, thyroid autoantibodies as a risk factor for progression to thyroid disease were not examined owing to the retrospective nature of our analysis. Despite these limitations, our study is one of the few studies on SCH in childhood cancer survivors, and it provides new data for Korean survivors. We showed that a substantial number of leukemia and WT/NB/abdomen survivors developed SCH, and our follow-up data described the natural course of SCH in survivors.
In conclusion, SCH is a frequent late effect in childhood cancer survivors. Most leukemia and WT/NB/abdomen survivors with SCH recovered spontaneously. There was an increased risk of persistent SCH in survivors with brain/naso, lymphoma, or head radiation at doses ≥1800 cGy.
Figures and Tables
 | Fig. 1Cumulative incidence of normalization of thyroid function according to cancer type. Other tumors included Wilms tumor, neuroblastoma, abdomen tumors, sarcoma, and other cancer types. |
Table 1
Demographic Characteristics of Patients with Persistent Subclinical Hypothyroidism (SCH)

Table 2
Thyroid Function at 2 Years after Cancer Treatment Completion

Table 3
Change of Thyroid Function during Follow-Up

Table 4
Thyroid Function According to Chemotherapeutic Agent
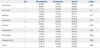
Table 5
Thyroid Function According to Radiation Site and Dose

Table 6
Multivariable Analysis of Risk Factors for Persistent Subclinical Hypothyroidism
References
1. Hewitt M, Weiner SL, Simone JV. Childhood cancer survivorship: improving care and quality of life. Washington, DC: National Academies Press;2003.
2. Pui CH, Pei D, Pappo AS, Howard SC, Cheng C, Sandlund JT, et al. Treatment outcomes in black and white children with cancer: results from the SEER database and St Jude Children's Research Hospital, 1992 through 2007. J Clin Oncol. 2012; 30:2005–2012.

3. Kurt BA, Armstrong GT, Cash DK, Krasin MJ, Morris EB, Spunt SL, et al. Primary care management of the childhood cancer survivor. J Pediatr. 2008; 152:458–466.

4. Chemaitilly W, Sklar CA. Endocrine complications in long-term survivors of childhood cancers. Endocr Relat Cancer. 2010; 17:R141–R159.

5. Nandagopal R, Laverdière C, Mulrooney D, Hudson MM, Meacham L. Endocrine late effects of childhood cancer therapy: a report from the Children's Oncology Group. Horm Res. 2008; 69:65–74.

6. Monzani A, Prodam F, Rapa A, Moia S, Agarla V, Bellone S, et al. Endocrine disorders in childhood and adolescence. Natural history of subclinical hypothyroidism in children and adolescents and potential effects of replacement therapy: a review. Eur J Endocrinol. 2012; 168:R1–R11.

7. Han JW, Kwon SY, Won SC, Shin YJ, Ko JH, Lyu CJ. Comprehensive clinical follow-up of late effects in childhood cancer survivors shows the need for early and well-timed intervention. Ann Oncol. 2009; 20:1170–1177.

8. Gharib H, Tuttle RM, Baskin HJ, Fish LH, Singer PA, McDermott MT. Subclinical thyroid dysfunction: a joint statement on management from the American Association of Clinical Endocrinologists, the American Thyroid Association, and the Endocrine Society. J Clin Endocrinol Metab. 2005; 90:581–585.

9. Garber JR, Cobin RH, Gharib H, Hennessey JV, Klein I, Mechanick JI, et al. Clinical practice guidelines for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 2012; 22:1200–1235.

10. Catli G, Abaci A, Büyükgebiz A, Bober E. Subclinical hypothyroidism in childhood and adolescense. J Pediatr Endocrinol Metab. 2014; 27:1049–1057.

11. Lazar L, Frumkin RB, Battat E, Lebenthal Y, Phillip M, Meyerovitch J. Natural history of thyroid function tests over 5 years in a large pediatric cohort. J Clin Endocrinol Metab. 2009; 94:1678–1682.

12. Ishiguro H, Yasuda Y, Tomita Y, Shinagawa T, Shimizu T, Morimoto T, et al. Long-term follow-up of thyroid function in patients who received bone marrow transplantation during childhood and adolescence. J Clin Endocrinol Metab. 2004; 89:5981–5986.

13. Madanat LM, Lähteenmäki PM, Alin J, Salmi TT. The natural history of thyroid function abnormalities after treatment for childhood cancer. Eur J Cancer. 2007; 43:1161–1170.

14. Landier W, Bhatia S, Eshelman DA, Forte KJ, Sweeney T, Hester AL, et al. Development of risk-based guidelines for pediatric cancer survivors: the Children's Oncology Group Long-Term Follow-Up Guidelines from the Children's Oncology Group Late Effects Committee and Nursing Discipline. J Clin Oncol. 2004; 22:4979–4990.

16. Kim TH, Kim KW, Ahn HY, Choi HS, Won H, Choi Y, et al. Effect of seasonal changes on the transition between subclinical hypothyroid and euthyroid status. J Clin Endocrinol Metab. 2013; 98:3420–3429.

17. Kim YA, Park YJ. Prevalence and risk factors of subclinical thyroid disease. Endocrinol Metab (Seoul). 2014; 29:20–29.

18. Somwaru LL, Rariy CM, Arnold AM, Cappola AR. The natural history of subclinical hypothyroidism in the elderly: the cardiovascular health study. J Clin Endocrinol Metab. 2012; 97:1962–1969.

19. Meyerovitch J, Rotman-Pikielny P, Sherf M, Battat E, Levy Y, Surks MI. Serum thyrotropin measurements in the community: five-year follow-up in a large network of primary care physicians. Arch Intern Med. 2007; 167:1533–1538.
20. Huber G, Staub JJ, Meier C, Mitrache C, Guglielmetti M, Huber P, et al. Prospective study of the spontaneous course of subclinical hypothyroidism: prognostic value of thyrotropin, thyroid reserve, and thyroid antibodies. J Clin Endocrinol Metab. 2002; 87:3221–3226.

21. Rodondi N, den Elzen WP, Bauer DC, Cappola AR, Razvi S, Walsh JP, et al. Subclinical hypothyroidism and the risk of coronary heart disease and mortality. JAMA. 2010; 304:1365–1374.

22. Boekholdt SM, Titan SM, Wiersinga WM, Chatterjee K, Basart DC, Luben R, et al. Initial thyroid status and cardiovascular risk factors: the EPIC-Norfolk prospective population study. Clin Endocrinol (Oxf). 2010; 72:404–410.

23. Rodondi N, Newman AB, Vittinghoff E, de Rekeneire N, Satterfield S, Harris TB, et al. Subclinical hypothyroidism and the risk of heart failure, other cardiovascular events, and death. Arch Intern Med. 2005; 165:2460–2466.

24. Chung GE, Kim D, Kim W, Yim JY, Park MJ, Kim YJ, et al. Non-alcoholic fatty liver disease across the spectrum of hypothyroidism. J Hepatol. 2012; 57:150–156.

25. Baldini IM, Vita A, Mauri MC, Amodei V, Carrisi M, Bravin S, et al. Psychopathological and cognitive features in subclinical hypothyroidism. Prog Neuropsychopharmacol Biol Psychiatry. 1997; 21:925–935.

26. Han JW, Kim HS, Kim BS, Kwon SY, Shin YJ, Kim SH, et al. Increasing and worsening late effects in childhood cancer survivors during follow-up. J Korean Med Sci. 2013; 28:755–762.

27. Vogelius IR, Bentzen SM, Maraldo MV, Petersen PM, Specht L. Risk factors for radiation-induced hypothyroidism: a literature-based meta-analysis. Cancer. 2011; 117:5250–5260.
28. Jereczek-Fossa BA, Alterio D, Jassem J, Gibelli B, Tradati N, Orecchia R. Radiotherapy-induced thyroid disorders. Cancer Treat Rev. 2004; 30:369–384.

29. Littley MD, Shalet SM, Beardwell CG, Robinson EL, Sutton ML. Radiation-induced hypopituitarism is dose-dependent. Clin Endocrinol (Oxf). 1989; 31:363–373.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download