Abstract
Purpose
Many epidemiological studies have investigated environmental risk factors for the development of acoustic neuroma. However, these results are controversial. We conducted a meta-analysis of case-control studies to identify any potential relationship between history of noise exposure, smoking, allergic diseases, and risk of acoustic neuroma.
Materials and Methods
We searched PubMed to identify relevant articles. Two researchers evaluated the eligibility and extracted the data independently.
Results
Eleven case-control studies were included in our meta-analysis. Acoustic neuroma was found to be associated with leisure noise exposure [odds ratio (OR)=1.33, 95% confidence interval (CI): 1.05–1.68], but not with occupational noise exposure and ever noise exposure (OR=1.20, 95% CI: 0.84–1.72 and OR=1.15, 95% CI: 0.80–1.65). The OR of acoustic neuroma for ever (versus never) smoking was 0.53 (95% CI: 0.30–0.94), while the subgroup analysis indicated ORs of 0.95 (95% CI: 0.81–1.10) and 0.49 (95% CI: 0.41–0.59) for ex-smoker and current smoker respectively. The ORs for asthma, eczema, and seasonal rhinitis were 0.98 (95% CI: 0.80–1.18), 0.91 (95% CI: 0.76–1.09), and 1.52 (95% CI: 0.90–2.54), respectively.
Conclusion
Our meta-analysis is suggestive of an elevated risk of acoustic neuroma among individuals who were ever exposed to leisure noise, but not to occupational noise. Our study also indicated a lower acoustic neuroma risk among ever and current cigarette smokers than never smokers, while there was no significant relationship for ex-smokers. No significant associations were found between acoustic neuroma and history of any allergic diseases, such as asthma, eczema, and seasonal rhinitis.
Acoustic neuroma, also referred to as vestibular schwannoma, is a benign, generally slow-growing tumor that develops in the acoustic nerve Schwann's sheath in the inner auditory canal. This tumor constitutes about 6 percent of all intracranial tumors, with an incidence from 1 to 20 per million per year.1234 The gender ratio (females/males) for acoustic neuroma has been reported to be greater than 1, and the mean age at diagnosis of tumor ranges from 50 to 55 years old.12 Due to better diagnostic tools and increased awareness of the disease, patients with acoustic neuroma can receive earlier diagnosis and better therapy.
Currently, the etiology of acoustic neuroma remains largely unknown. However, several studies have shown some predisposing factors for the development of acoustic neuroma, such as ionizing radiation, radio frequency electromagnetic fields (e.g., from mobile phone use), noise exposure, and allergic diseases. Studies of children from atomic bomb survivors in Japan have linked moderate to high doses of ionizing radiation to increased acoustic neuroma.56 Many case-control studies have investigated the risk of acoustic neuroma after mobile phone use with inconsistent results.789 The systematic review by Hardell, et al.10 indicated an increased risk for ipsilateral acoustic neuroma after >10 years of mobile phone use with a calculated odds ratio (OR) of 1.6 [95% confidence interval (CI): 1.1–2.4]. Until now, there is no systematic review analyzing the potential risk of history of noise exposure, smoking, and allergic diseases for acoustic neuroma. Thus, we carried out a meta-analysis of case-control studies to clarify whether these histories are risk factors of acoustic neuroma.
We searched PubMed to identify relevant studies published from the inception thereof to January 2015 using the following search terms: 1) "noise/sound", "smoking/tobacco/smoke/cigarette", "allergy/autoimmune", and "risk factor"; 2) acoustic neuroma, vestibular schwannoma, and brain tumor. In addition, we searched the bibliographies of all identified relevant publications and the bibliographies from citations for relevant articles. Publication language was restricted. All studies identified by this process were subsequently screened by two independent reviewers (Chen and Fan).
Two reviewers (Chen and Fan) evaluated the studies independently and discrepancies were resolved through discussion. Articles were selected on the basis of the following criteria: 1) case-control study; 2) acoustic neuroma cases that were medically confirmed; and 3) raw data necessary to calculate OR with CI. Studies were excluded if they did not have adequate data to calculate ORs and 95% CIs. Generally, we chose studies with a relatively larger quantity for the same research.
The following data were extracted from eligible studies: study authors, publication year, study site, sample size (numbers of case patients and control subjects), research instruments, and research contents. The two investigators above extracted the necessary data independently from all included studies. ORs and their respective 95% CIs were calculated from available raw data.
Meta-analysis was performed on the extracted data with STATA 11 software (StataCorp, College Station, TX, USA). The heterogeneity between included studies was assessed using I2 test. Heterogeneity was considered to be significant when I2 >75% and p<0.05. The data from each study were combined using a fixed-effect model with the Mantel-Haenszel method in case no heterogeneity was presented. Otherwise, the random-effect model with the DerSimonian-Laird method was used for analysis.
After searching PubMed and the bibliographies of all identified relevant publications, as well as screening by the inclusion and exclusion criteria, 11 case-control studies were eligible. 1112131415161718192021 The study authors, publication year, study site, sample size (numbers of case patients and control subjects), type of control, research instruments, and research contents are all listed in Table 1.
The included studies in the meta-analysis for the risk associated with noise exposure comprised eight studies. There was a high heterogeneity among these studies (I2=87.3%); therefore, a random-effects model was used to analyze the association between ever and never noise exposure. The OR was 1.15 (95% CI: 0.80–1.65). As the assessment of these studies indicated a high heterogeneity for occupational noise exposure (I2=86.4%), the random-effects model was used to calculate the OR of 1.20 (95% CI: 0.84–1.72). The OR for leisure noise exposure was 1.33 (95% CI: 1.05–1.68) with a fixed-effects model (I2=0.00%) (Fig. 1).
There were six studies including raw data on smoking. There was a high heterogeneity among these studies (I2=93.7%), and a random-effects model was used to analyze associations. The OR was 0.53 (95% CI: 0.30–0.94). Only four studies had data on ex-smoker and current smoker. There was no heterogeneity among these four studies (I2=0.00%), and a fixed-effects model was used to analyze associations. The ORs were 0.95 (95% CI: 0.81–1.10) and 0.49 (95% CI: 0.41–0.59) for ex-smokers and current smokers, respectively (Fig. 2).
Five studies were included in the risk analysis of allergic diseases (asthma, eczema, and seasonal rhinitis). A fixed-effects model was used for the analysis of asthma and eczema (I2= 51.9% and 55.2%), while a random-effects model was used for seasonal rhinitis (I2=88.8%). The ORs for asthma, eczema, and seasonal rhinitis were 0.98 (95% CI: 0.80–1.18), 0.91 (95% CI: 0.76–1.09), and 1.52 (95% CI: 0.90–2.54), respectively (Fig. 3).
Our meta-analysis suggested an elevated risk of acoustic neuroma among individuals who were ever exposed to leisure noise, but not to occupational noise and ever occupational or leisure noise exposure. Our study also indicated a lower acoustic neuroma risk among ever and current cigarette smokers than among never smokers, while there was no significant relationship for ex-smokers. Furthermore, no significant associations were found between acoustic neuroma and history of any allergic diseases, such as asthma, eczema, and seasonal rhinitis.
In our study, acoustic neuroma was found to be associated with leisure noise exposure (OR=1.33, 95% CI: 1.05–1.68), whereas no statistically significant association was found between occupational noise exposure and acoustic neuroma (OR=1.20, 95% CI: 0.84–1.72). The eight studies employed two methods of data analysis: self-reports and job exposure matrix. We extracted the self-reported exposure data to analyze the result of noise exposure in our study. The self-reported exposure results of eight studies were inconsistent, which induced the negative meta-analysis result. However, the two studies that used the job exposure matrix did not demonstrate an increased risk of acoustic neuroma related to occupational noise exposure, even after allowing for a long latency period.1521 Two studies have implied loud leisure noise as a risk factor for acoustic neuroma, 1721 while the other two studies did not imply the same conclusion. 1316 However, the largest-sample study by Fisher, et al.21 occupied the weight of 83.2%, which led to the elevated risk of acoustic neuroma for leisure noise exposure. The different results between the occupational and leisure noise exposure may be due to the healthy worker survivor effect.22 The participants, who developed hearing loss or tinnitus under the condition of high-noise, may have left their occupations or transferred to lower noise exposure occupations. Furthermore, people may willingly expose unprotected ears to leisure noise levels that would be unacceptable in the working environment and the participants who are exposed to occupational noise may wear protection devices that reduce the risk of acoustic neuroma.
Although noise exposure has been a possible predisposing factor in the development of acoustic neuroma, the exact mechanism of noise on acoustic neuroma is still unclear. Experimental studies in rodents have shown clearly that severe acoustic trauma from impulse noise causes mechanical damage of the eighth nerve and the surrounding tissue.23 The electrolytes disequilibrium of Cochlea fluids and free radicals by loud acoustic stimulation could induce DNA damage in cochlear cells.172425 If cancer risk is proportional to the number of proliferating cells that occurs during the repair process, as has been previously postulated,26 it is then plausible that a benign tumor such as acoustic neuroma may arise due to cochlear hair cell trauma. In the course of cellular repair processes, cellular division results in replication errors of DNA that may in turn lead to chromosomal changes necessary for neoplastic transformation.11
The OR of acoustic neuroma for the ever (versus never) smoking was 0.53 (95% CI: 0.30–0.94), while subgroup analysis indicated ORs of 0.95 (95% CI: 0.81–1.10) and 0.49 (95% CI: 0.41–0.59) for ex-smokers and current smokers, respectively. Only one study by Schoemaker, et al.14 analyzed the role of cigarette smoking on the risk of acoustic neuroma, while other case-control studies only had the necessary data on cigarette smoking. Schoemaker, et al. indicated that the risk of acoustic neuroma was significantly reduced in subjects who had regularly smoked cigarettes, although the reduction occurred only in current smokers, not ex-smokers. There are two studies similar to our current work.2728 One study by Palmisano, et al.,27 in which data were extracted from the study by Fisher, found that the risks for ever cigarette smoking, former smoker, and current smoker were 0.80 (95% CI: 0.61–1.04), 0.98 (95% CI: 0.73–1.32), and 0.54 (95% CI: 0.36–0.81), respectively. Another excluded cohort study by Benson, et al.28 noted that current smokers were at significantly reduced risk of acoustic neuroma, compared with never smokers [adjusted relative risk (RR)=0.41, 95% CI: 0.24–0.70], and past smokers had no significantly different risk than never smokers (RR=0.87, 95% CI: 0.62–1.22).
The possible mechanisms for the inverse association between smoking and risk of acoustic neuroma are as follows: Both in vitro and in vivo animal studies have shown that nicotine exposure suppresses the severity of experimental autoimmune encephalomyelitis.2930 This attenuated inflammatory response implicated nicotine as the chemical substance responsible for the protective effects on acoustic neuroma genesis. 27 Smoking has a hypoxic effect on human tissue, and the onset and duration of tissue hypoxia paralleled the well-established plasma pharmacokinetics of nicotine.31 In vitro study showed a significant decrease in the Schwann cells survival after culture under a hypoxia/reoxygenation condition, which reduced the mRNA levels of brain derived neurotrophic factor (BDNF).32 BDNF mRNA expression is significantly up-regulated in acoustic neuroma and correlated with proliferative activity, as shown by the analysis of the acoustic neuroma samples. 33 The latter pathway can reasonably explain why cigarette smoking protects against acoustic neuroma risk.
Five studies were included in the risk analysis of allergic diseases. The ORs for asthma, eczema, and seasonal rhinitis were 0.98 (95% CI: 0.80–1.18), 0.91 (95% CI: 0.76–1.09), and 1.52 (95% CI: 0.90–2.54), respectively. Studies by Brenner, et al.12 and Shoemaker, et al.14 showed no significant association between allergic diseases and risk of acoustic neuroma, whereas a study by Schlehofer, et al.16 found an increased risk for seasonal rhinitis, but not asthma and eczema. A large, 13-country population-based case-control study indicated a significant inverse association between allergic history and acoustic neuroma (OR= 0.64, 95% CI: 0.49–0.83). Meanwhile, inverse associations with asthma and seasonal rhinitis were strengthened with increasing age of allergy onset and weakened with longer time since onset.20 However, a case-control study nested in the European Prospective Investigation into Cancer study reported an inverse association between elevated respiratory-specific IgE concentrations and glioma (OR=0.73, 95% CI: 0.51–1.06), but not meningioma or acoustic neuroma.34
Publications on the direct effect of allergic diseases on the development of acoustic neuroma are scarce. One explanation for the inverse associations between an allergic history and cancer risk is the hypothesis of immuno-surveillance, which was proposed firstly in 1970 by Burnet.35 The hypothesis states that the immune system protects the host against the development of cancer. Another explanation might be reverse causality, which means that the observed association might be due to suppression of immune system by the tumor itself.34
Nevertheless, the present meta-analysis indicated that seasonal rhinitis may be a possible risk factor of acoustic neuroma (OR=1.52, 95% CI: 0.90–2.54). Sensitivity analyses for the meta-analysis of seasonal rhinitis showed that exclusion of any single study did not materially alter the overall combined risk estimate, with a range from 1.34 (95% CI: 0.78–2.29) to 1.89 (95% CI: 1.13–3.16). Until now, there have been no exact mechanisms postulated on the relationship between seasonal rhinitis and acoustic neuroma. A study investigating the association between seasonal rhinitis and polymorphisms in Th1, Th2, and cytokine genes suggested a high association of several genetic variants for elevated IgE phenotype in seasonal rhinitis patients.36 IgE-mediated allergic rhinitis may result in dysfunction of the eustachian tube and otitis media, which might prompt patients to receive additional examinations and discovery of acoustic neuroma.12
There are still several other possible risk factors for acoustic neuroma, such as head injury, alcohol consumption, and history of cancer. The study by Schoemaker, et al.14 found that the risk of acoustic neuroma was not significantly reduced in participants who had a history of head trauma (OR=0.8, 95% CI: 0.6–1.1). The result was consistent with the case-control study by Corona, et al.18 (OR=1.37, 95% CI: 0.66–2.82) and the cohort study by Inskip, et al.37 (RR=0.8, 95% CI: 0.4–1.7). However, one neighborhood-base case-control study indicated a two-fold increase in acoustic neuroma risk in men 30 years or older after a major head trauma.11 The study by Schoemaker, et al.14 further indicated that the risk of acoustic neuroma is significantly raised for a history of epilepsy (OR=2.5, 95% CI: 1.3–4.9). Earlier studies found that acoustic neuroma risk was not related to consumption of alcohol, history of cancer/diabetes, and family cancer.111418
Several limitations of this study should be considered. Firstly, our meta-analysis contains 11 case-control studies. Owing to information about exposure that relied on the participants' memory, recall bias is common in case-control studies. Secondly, the sample sizes between these eligible studies vary widely. Several studies included a relatively small sample,1118 which raised some concerns regarding the reliability of their results. Thirdly, there are potential confounding factors that may affect the results, such as different control types and research instruments. Among the enrolled studies, different studies are adjusted for different confounding factors: for example, age, gender, socioeconomic status, and region.
In summary, this meta-analysis suggested an elevated risk of acoustic neuroma among individuals who are ever exposed to leisure noise but not to occupational noise. We also found a lower acoustic neuroma risk among ever and current cigarette smokers than never smokers, whereas there was no significant relationship for ex-smokers. The elevated risk of acoustic neuroma was not positively related with any allergic diseases. The public health hazards associated with both cigarette smoking and occupational noise are well known and well documented; therefore, it is not our intention to endorse smoking as a means of protection against the development of acoustic neuroma. We also do not support loud occupational noise exposure without protection devices. Considering the limitations of our meta-analysis, our present findings should be interpreted with caution. Prospective studies including enough cases are needed to further confirm the role of these risk factors in the etiology of acoustic neuroma.
Figures and Tables
 | Fig. 1Odds ratio (OR) and 95% confidence interval (CI) for the association between ever noise exposure (A), occupational (B), and leisure noise exposure (C) versus never noise exposure and risk of acoustic neuroma. |
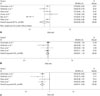 | Fig. 2Odds ratio (OR) and 95% confidence interval (CI) for the association between (A) ever, (B) ex-smoker, and (C) current smoker versus never smoking and risk of acoustic neuroma. |
 | Fig. 3Odds ratio (OR) and 95% confidence interval (CI) for the association between (A) asthma, (B) eczema, and (C) seasonal rhinitis and risk of acoustic neuroma. |
Table 1
Description of Epidemiological Studies on History of Noise Exposure, Smoking, Allergic Diseases, and Risk of Acoustic Neuroma

| Study | Year | Country | Case/control | Type of control | Research contents | Research instrument |
|---|---|---|---|---|---|---|
| Preston-Martin, et al.11 | 1989 | USA | 86/86 | Neighborhood | Occupational noise | Interview |
| Brenner, et al.12 | 2002 | USA | 96/799 | Hospital | Allergies and autoimmune diseases | Interview |
| Edwards, et al.13 | 2006 | Sweden | 146/564 | Population | Occupational and nonoccupational noise | Interview or questionnaire |
| Schoemaker, et al.14 | 2007 | Nordic countries and United Kingdom | 563/2703 | Population | Allergic diseases, smoking | Interview |
| Edwards, et al.15 | 2007 | Swedish | 793/101756 | Population | Occupational noise | Censuses data |
| Schlehofer, et al.16 | 2007 | Germany | 97/194 | Population | Smoking, noise (occupation and leisure), allergic diseases | Interview |
| Hours, et al.17 | 2009 | France | 108/212 | Population | Smoking, noise (occupation and leisure) | Interview |
| Corona, et al.18 | 2012 | Brazil | 44/104 | Hospital | Tobacco, occupational noise | Interview |
| Han, et al.19 | 2012 | USA | 343/343 | Hospital | Smoking, occupational noise, allergic disease | Questionnaire |
| Turner, et al.20 | 2013 | Australia, Canada, France, Israel, New Zealand | 394/2520 | Population | Allergy, allergic disease | Interview |
| Fisher, et al.21 | 2014 | Sweden | 451/710 | Population | Smoking, noise (occupational and leisure) | Questionnaire |
ACKNOWLEDGEMENTS
We thanks for the funding from medicine and health technology projects of Zhejiang Province (NO. 201350473). The funding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
1. Howitz MF, Johansen C, Tos M, Charabi S, Olsen JH. Incidence of vestibular schwannoma in Denmark, 1977-1995. Am J Otol. 2000; 21:690–694.
2. Propp JM, McCarthy BJ, Davis FG, Preston-Martin S. Descriptive epidemiology of vestibular schwannomas. Neuro Oncol. 2006; 8:1–11.
3. Stangerup SE, Tos M, Thomsen J, Caye-Thomasen P. True incidence of vestibular schwannoma? Neurosurgery. 2010; 67:1335–1340.

4. Gal TJ, Shinn J, Huang B. Current epidemiology and management trends in acoustic neuroma. Otolaryngol Head Neck Surg. 2010; 142:677–681.

5. Preston DL, Ron E, Yonehara S, Kobuke T, Fujii H, Kishikawa M, et al. Tumors of the nervous system and pituitary gland associated with atomic bomb radiation exposure. J Natl Cancer Inst. 2002; 94:1555–1563.

6. Yonehara S, Brenner AV, Kishikawa M, Inskip PD, Preston DL, Ron E, et al. Clinical and epidemiologic characteristics of first primary tumors of the central nervous system and related organs among atomic bomb survivors in Hiroshima and Nagasaki, 1958-1995. Cancer. 2004; 101:1644–1654.

7. Schoemaker MJ, Swerdlow AJ, Ahlbom A, Auvinen A, Blaasaas KG, Cardis E, et al. Mobile phone use and risk of acoustic neuroma: results of the Interphone case-control study in five North European countries. Br J Cancer. 2005; 93:842–848.

8. Hardell L, Carlberg M, Hansson Mild K. Case-control study on cellular and cordless telephones and the risk for acoustic neuroma or meningioma in patients diagnosed 2000-2003. Neuroepidemiology. 2005; 25:120–128.

9. Inskip PD, Tarone RE, Hatch EE, Wilcosky TC, Shapiro WR, Selker RG, et al. Cellular-telephone use and brain tumors. N Engl J Med. 2001; 344:79–86.

10. Hardell L, Carlberg M, Hansson Mild K. Epidemiological evidence for an association between use of wireless phones and tumor diseases. Pathophysiology. 2009; 16:113–122.

11. Preston-Martin S, Thomas DC, Wright WE, Henderson BE. Noise trauma in the aetiology of acoustic neuromas in men in Los Angeles County, 1978-1985. Br J Cancer. 1989; 59:783–786.

12. Brenner AV, Linet MS, Fine HA, Shapiro WR, Selker RG, Black PM, et al. History of allergies and autoimmune diseases and risk of brain tumors in adults. Int J Cancer. 2002; 99:252–259.

13. Edwards CG, Schwartzbaum JA, Lnn S, Ahlbom A, Feychting M. Exposure to loud noise and risk of acoustic neuroma. Am J Epidemiol. 2006; 163:327–333.

14. Schoemaker MJ, Swerdlow AJ, Auvinen A, Christensen HC, Feychting M, Johansen C, et al. Medical history, cigarette smoking and risk of acoustic neuroma: an international case-control study. Int J Cancer. 2007; 120:103–110.

15. Edwards CG, Schwartzbaum JA, Nise G, Forssén UM, Ahlbom A, Lönn S, et al. Occupational noise exposure and risk of acoustic neuroma. Am J Epidemiol. 2007; 166:1252–1258.

16. Schlehofer B, Schlaefer K, Blettner M, Berg G, Böhler E, Hettinger I, et al. Environmental risk factors for sporadic acoustic neuroma (Interphone Study Group, Germany). Eur J Cancer. 2007; 43:1741–1747.

17. Hours M, Bernard M, Arslan M, Montestrucq L, Richardson L, Deltour I, et al. Can loud noise cause acoustic neuroma? Analysis of the INTERPHONE study in France. Occup Environ Med. 2009; 66:480–486.

18. Corona AP, Ferrite S, Lopes Mda S, Rgo MA. Risk factors associated with vestibular nerve schwannomas. Otol Neurotol. 2012; 33:459–465.

19. Han YY, Berkowitz O, Talbott E, Kondziolka D, Donovan M, Lunsford LD. Are frequent dental x-ray examinations associated with increased risk of vestibular schwannoma? J Neurosurg. 2012; 117:Suppl. 78–83.

20. Turner MC, Krewski D, Armstrong BK, Chetrit A, Giles GG, Hours M, et al. Allergy and brain tumors in the INTERPHONE study: pooled results from Australia, Canada, France, Israel, and New Zealand. Cancer Causes Control. 2013; 24:949–960.

21. Fisher JL, Pettersson D, Palmisano S, Schwartzbaum JA, Edwards CG, Mathiesen T, et al. Loud noise exposure and acoustic neuroma. Am J Epidemiol. 2014; 180:58–67.

22. Arrighi HM, Hertz-Picciotto I. The evolving concept of the healthy worker survivor effect. Epidemiology. 1994; 5:189–196.

23. Hamernik RP, Turrentine G, Wright CG. Surface morphology of the inner sulcus and related epithelial cells of the cochlea following acoustic trauma. Hear Res. 1984; 16:143–160.

24. Watanabe K, Inai S, Hess A, Michel O, Yagi T. Acoustic stimulation promotes the expression of inducible nitric oxide synthase in the vestibule of guinea pigs. Acta Otolaryngol Suppl. 2004; (553):54–57.

25. Van Campen LE, Murphy WJ, Franks JR, Mathias PI, Toraason MA. Oxidative DNA damage is associated with intense noise exposure in the rat. Hear Res. 2002; 164:29–38.

26. Albanes D, Winick M. Are cell number and cell proliferation risk factors for cancer? J Natl Cancer Inst. 1988; 80:772–774.
27. Palmisano S, Schwartzbaum J, Prochazka M, Pettersson D, Bergenheim T, Florentzson R, et al. Role of tobacco use in the etiology of acoustic neuroma. Am J Epidemiol. 2012; 175:1243–1251.

28. Benson VS, Green J, Pirie K, Beral V. Cigarette smoking and risk of acoustic neuromas and pituitary tumours in the Million Women Study. Br J Cancer. 2010; 102:1654–1656.

29. Shi FD, Piao WH, Kuo YP, Campagnolo DI, Vollmer TL, Lukas RJ. Nicotinic attenuation of central nervous system inflammation and autoimmunity. J Immunol. 2009; 182:1730–1739.

30. Nizri E, Irony-Tur-Sinai M, Lory O, Orr-Urtreger A, Lavi E, Brenner T. Activation of the cholinergic anti-inflammatory system by nicotine attenuates neuroinflammation via suppression of Th1 and Th17 responses. J Immunol. 2009; 183:6681–6688.

31. Jensen JA, Goodson WH, Hopf HW, Hunt TK. Cigarette smoking decreases tissue oxygen. Arch Surg. 1991; 126:1131–1134.

32. Zhu H, Li F, Yu WJ, Wang WJ, Li L, Wan LD, et al. Effect of hypoxia/reoxygenation on cell viability and expression and secretion of neurotrophic factors (NTFs) in primary cultured schwann cells. Anat Rec (Hoboken). 2010; 293:865–870.

33. Kramer F, Stöver T, Warnecke A, Diensthuber M, Lenarz T, Wissel K. BDNF mRNA expression is significantly upregulated in vestibular schwannomas and correlates with proliferative activity. J Neurooncol. 2010; 98:31–39.

34. Schlehofer B, Siegmund B, Linseisen J, Schüz J, Rohrmann S, Becker S, et al. Primary brain tumours and specific serum immuno-globulin E: a case-control study nested in the European Prospective Investigation into Cancer and Nutrition cohort. Allergy. 2011; 66:1434–1441.

36. Nieters A, Linseisen J, Becker N. Association of polymorphisms in Th1, Th2 cytokine genes with hayfever and atopy in a subsample of EPIC-Heidelberg. Clin Exp Allergy. 2004; 34:346–353.

37. Inskip PD, Mellemkjaer L, Gridley G, Olsen JH. Incidence of intracranial tumors following hospitalization for head injuries (Denmark). Cancer Causes Control. 1998; 9:109–116.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download