INTRODUCTION
The Trauma and Injury Severity Score (TRISS) is an injury severity scoring system developed by combining a patient's age, Injury Severity Score (ISS), and Revised Trauma Score (RTS).
1 Despite its known limitations,
23456 TRISS is used worldwide for benchmarking trauma outcomes.
7891011 The TRISS coefficient, which is used to give the variable weights, derived from an ordinary logistic regression of the Major Trauma Outcome Study (MTOS) database created in the U.S. in 1987.
12 In 1995, revisions were made by the American College of Surgeons Committee on Trauma.
3 Most of the recent studies involving Asian populations
91011 used the MTOS-derived coefficient revised in 1995. However, owing to a great deal of progress in the trauma care system, it has been steadily proposed that the coefficients be revised again. In fact, various studies are available on the topic.
13141516 In particular, the TRISS coefficients 2009 revision study published in 2010
13 proposed a new set of coefficients upon an analysis of U.S. National Trauma Data Bank (NTDB) and National Sample Project (NSP) large data sets. Recent European and Japanese studies
891011171819 have produced new coefficients or devised a new scoring system by modifying the TRISS predictors. However, such a discussion is non-existent in Korea, where the trauma care system is not as well established, and no such databases have been compiled.
The Korean government has been attempting to develop a plan to establish regional trauma care centers across the nation, which was set motion in 2012. In addition, the Korea Trauma Data Bank (KTDB) was established in 2013 by mandating registration of trauma victims at the institutes participating in the project. However, various hurdles have hindered its progress, and no notable outcomes have been attained thus far. The current study aimed to verify the utility of the existing TRISS coefficients by using the data collected in 2014 and to improve the quality of data entered through the course of the study. Additionally, the study aimed to propose a new trauma mortality or survival prediction model with a new set of TRISS coefficients or predictors composing TRISS, which would allow a more accurate prediction of prognosis for trauma patients.
MATERIALS AND METHODS
Hospital setting and patient data
The medical center where the authors are employed is a tertiary university hospital visited by approximately 17000 trauma patients annually, approximately 2000–3000 of whom receive in-patient treatment. Since being selected for the regional trauma center project in 2013 by the government, our medical center has been equipped with 20 intensive care unit beds, a two-bed resuscitation room for trauma cases (T-bay), and two operation rooms specialized for trauma victims. The level of the facility corresponds to that of a U.S. Level-I trauma center. The facility is run by 12 dedicated trauma faculty members, including four general surgeons, one thoracovascular surgeon, one emergency physician, one neurosurgeon, four orthopedic surgeons, and one radiologist.
Of the trauma patients who were admitted to our medical center in 2014, those eligible for KTDB entry were selected, and TRISS predictors such as age, ISS, and RTS were collected. ISS was coded by three nurses (one trauma program manager and two trauma coordinators), whose work was confirmed by specialists in the trauma care center. For RTS calculation, the initial systolic blood pressure (SBP), respiratory rate (RR), and Glasgow Coma Scale (GCS) measured at emergency room admission were used.
Study sample (inclusion and exclusion criteria)
KTDB inclusion criteria were as follows:
1) Disease status of "causes other than disease".
2) Status of "hopeless discharge," "discharge," "transfer," "admission," or "deceased".
3) Diagnosis data at emergency room (ER) discharge, diagnosis data codes of S or T at hospital discharge (with the exclusion of certain codes).
• Trauma registration exclusion codes:
-Superficial injury, blister: S00.01, S00.21, S00.31, S00.41, S00.51, S00.91, S10.11, S10.81, S10.91, S20.11, S20.31, S20.41, S20.81, S30.81, S30.91, S40.81, S50.81, S60.81, S70.81, S80.81, S90.91
-Insect bite (nonvenomous): S00.02, S00.22, S00.32, S00.42, S00.52, S00.82, S00.92, S10.12, S10.82, S10.92, S20.12, S20.32, S20.42, S20.82, S30.82, S30.92, S40.82, S50.82, S60.82, S70.82, S80.82, S90.82
-Foreign body: T15–T19
-Poisoning: T36–T65
-Superficial injuries involving multiple body regions, injury of unspecified body region: T00.8, T14.0
Although the trauma victims who died in the emergency department despite resuscitation efforts were included, those who had an ISS that could not be measured were excluded. Ultimately, only the blunt trauma patients 15 years of age and older were included in the study.
The TRISS model
TRISS coefficients, which are used to give the variable weights, were originally estimated from ordinary logistic regression models in 1987
12 and then revised in 1995
3 using the MTOS database coordinated by the American College of Surgeons Committee on Trauma. In the TRISS model, if the patient is 15 years of age and older, different coefficients are used according to the type of injury mechanism (blunt or penetrating). The current study involved only trauma patients 15 years and older. TRISS determines the probability of survival (P
S) of a patient using the following formula:
Here, α is an injury mechanism type (blunt or penetrating) coefficient, β
age is an age coefficient, β
RTS is an RTS coefficient, and β
ISS is an ISS coefficient. RTS is calculated using the following formula, where β
RR is an RR coefficient, β
SBP is an SBP coefficient, and β
GCS is a GCS coefficient.
Ultimately, the above formulas can be reorganized into the following formula:
The TRISS coefficient and statistical analyses
The study data were input into the above TRISS formula in order to obtain P
S values, which were examined for consistency with actual patient survival status. For TRISS coefficients, MTOS-derived values revised in 1995
112 and NTDB-derived coefficients and NSP-derived coefficients revised in 2009
13 were used. Particularly in the study on the TRISS coefficients revision that was performed in 2009, analyses were conducted on the complete and imputed values. Here, "complete" cases were those patients with valid non-missing data for all covariates, and "imputed" data were those covariates with invalid or missing data converted using a statistical method.
13 Areas under the receiver operating characteristic (ROC) curve (AUC) for each prediction ability were obtained, and a pairwise comparison of ROC curves was performed using the Hanley and McNeil method. Additionally, using a logistic regression method, a new set of coefficients were derived from our medical center's database (Ajou Trauma Data Bank, ATDB), and several of the TRISS predictor variables were modified in an aim to identify a model superior to the existing TRISS model. Subsequently, AUCs were obtained and compared with the existing data. We set out to modify several of the TRISS predictor variables to identify a model with superior predictive or explanatory power. We evaluated the quality of the model using the power of explanation of the model (-2 log likelihood, Nagelkerke R
2) and its calibration (Hosmer-Lemeshow test) and discriminative power (for the AUC).
We used SPSS version 22 (IBM Corp., Armonk, NY, USA) and MedCalc version 15.6.1 for Windows (MedCalc Software bvba, Broekstraat, Mariakerke, Belgium) for statistical analyses. Significance of statistical differences was attributed to p values<0.05.
Ethics statement
This study was approved by the Institutional Review Board of Ajou University Hospital (IRB No. AJIRB-MED-MDB-15-195). Informed consent was waived by the board due to the observational nature of the study.
RESULTS
Of the trauma patients treated at our medical center in 2014, a total of 2307 trauma patients met the eligibility requirements for KTDB data entry. A total of 2022 patients (87.6%) were 15 years or older, 1841 (91.0%) of whom were blunt trauma patients. TRISS scores of 1791 patients were obtained, upon exclusion of 50 death on arrival (DOA) patients. Forty-five patients (2.5%) were further excluded owing to missing data among TRISS predictor variables, which resulted in a total of 1746 patients enrolled in the study (
Fig. 1).
Table 1 displays the participants' basic demographic data and TRISS predictor variables.
Male participants accounted for 64.9% (1133 patients) of the total, patients 55 years and younger accounted for 58.2% (1016 participants), and close to half of all participants (794 participants, 45.5%) were patients transferred from another hospital to our trauma center. In the case of RR, no patient was found with an RR of 0–9, which corresponded to a coded value of 0, 1, or 2. In the case of SBP also, only one patient with an SBP of 0–49 mm Hg was found. On the other hand, age, GCS, and ISS exhibited a relatively even distribution. The median ISS value was 9 points, and the number of patients with ISS >15 was 435 (24.9%). A total of 86 patients died, yielding a crude mortality rate of 4.9% (86 of 1746) in the study (
Table 1).
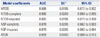
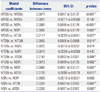
Table 2 displays the coefficients calculated for the TRISS predictor variables obtained from the existing database, as well as the coefficients estimated via a logistic regression performed with our medical center's data.
Fig. 2 displays the ROC curves created to examine the utility of the TRISS value (P
S) obtained by plugging in the coefficients.
Table 3 displays the calculated AUC values. The values indicate that ATDB (0.899)>MTOS (0.888)>NTDB-imputed (0.885)>NTDB-complete (0.880)>NSP-imputed (0.879)>NSP-complete (0.878), with associated 95% confidence intervals (CI) showing a tendency to overlap with one another. However, pairwise comparison of ROC curves indicated that ATDB had a significantly higher value than those of the others (
Table 4).
When certain TRISS predictor variables were modified (mTRISS) in an aim to identify a model superior to the existing TRISS model, we discovered that converting "coded age" into "continuous age" alone (b=α+β
age×continuous value of age+β
RR×RR+β
SBP×SBP+β
GCS×GCS+β
ISS×ISS) produced a model with a higher AUC value (0.913) and greater explanatory power (-2 log likelihood=437.652 vs. 455.739, R
2=0.408 vs. 0.380, respectively) than the existing TRISS model. In other words, the new model developed in the current study (mTRISS) had an explanatory power of 40.8%, which was greater than what was derived from regression of the existing TRISS model's predictor variable (38.0%). In addition, the model's calibration and fit were verified using the Hosmer-Lemeshow test results (χ
2=7.487,
p value=0.510) (
Table 5). Although pairwise comparison of the ROC curves (mTRISS vs. ATDB derived model) did not indicate statistically significant differences (
p value=0.064), a comparison with the MTOS-derived model, which had previously shown the most favorable results among the existing models, indicated a superior discriminative power (
p value=0.003) (
Table 6,
Fig. 3).
DISCUSSION
Although numerous injury severity scoring systems have been introduced historically, TRISS, which is developed by considering both the anatomical variables and physiologic factors, is currently accepted as the most effective method for benchmarking trauma outcomes.
7891011 Nevertheless, many Korean circumstances differ from those of the U.S., where the scoring system was developed. In particular, given that significant differences are found in the level of treatment provided to trauma patients, indiscriminately applying the trauma survival prediction model of another country when treating patients in Korea is bound to result in difficulties. In other words, verification based on a Korean trauma population is needed sooner rather than later. Thus, developing a new set of TRISS coefficients or a new prediction model will be highly beneficial.
The current study applied the existing TRISS coefficients to the adult blunt trauma population of a single trauma center in Korea. The results found AUC values of 0.878–0.888, which was lower than those of existing foreign studies (AUC: 0.896–0.928),
1314 indicating lower utility. However, for a more accurate comparison, further research involving a sample size comparable to that of the databases used in the foreign studies is needed. Nevertheless, the fact that a new coefficient closely approximating 0.9 was obtained in the current study is encouraging (AUC=0.899, 95% CI=0.884–0.913), considering that the value is significantly higher than those of other models and that the study sample only consisted of a single trauma care center's small scale database (ATDB) (
Table 2).
The Ministry of Health and Welfare established the KTDB in 2013, which has been collecting data from select regional trauma centers ever since. However, owing to the lack of a clear "data dictionary," the quality of registered data is questionable. Furthermore, despite the designation of a trauma care center in each region, a trauma patient transport system has not yet been firmly established, resulting in many patients being shuffled from one hospital to another until they are finally admitted. Moreover, the lack of clear definitions pertaining to parameters such as initial vital signs and GCS has added to the confusion commonly experienced in these circumstances. SBP, RR, and GCS, which were used in the study to calculate TRISS, are the initial measurements taken at our medical center. However, considering that 45.5% of patients are transferred from another hospital (
Table 1), it is an assumption to consider these measurements as the initial values fitting the definition of TRISS. Certain patients may have been admitted after an intubation performed at a previous hospital, while others may have been on sedatives administered at a previous hospital, which interferes with accurate measurement of initial RR and initial GCS. There is also the possibility that fluid, blood transfusion, or inotropes used during a previous resuscitation effort at another hospital may have elevated the initial SBP. It should be noted that there were no initial RR values below 9 and only one case of initial SBP below 50 in the study. It is thought that these factors negatively affected the predictive power and explanatory power of the model, resulting in a lower AUC value than those of the existing foreign studies. All cases, regardless of transfer, were included in this study, as the enrolled population would have been too small to draw significant results statistically if the cases transferred from other hospitals had been excluded. A follow-up large-scale study is needed to further examine these issues. Additionally, a clear and specific "data dictionary" is imperative at this point.
Regarding the comparison of outcomes by regional trauma care centers for benchmarking, the MTOS-derived coefficient revised in 1995 and the NTDB-imputed data coefficient revised in 2010 are thought to be suitable for the current circumstances in Korea (
Table 2,
3, and
4). However, we would like to recommend use of the MTOS coefficient in particular. No statistically significant difference was found when the ROC curves of the two coefficients were compared (0.888 vs. 0.885,
p value=0.149, respectively) (
Table 3 and
4). However, it should also be considered that most of the recent TRISS studies
8911 used the MTOS coefficients and that coordinators of the trauma centers in Korea mostly estimate the TRISS while using the TRISS calculation program at TRAUMA.ORG (a trauma information website run by a British trauma surgeon; calculations use MTOS-derived coefficients).
20
Further multi-institutional large-scale studies are needed in order to develop a new set of TRISS model coefficients or a so-called Korean trauma outcome prediction model. The model developed in the current study capitalized on such an assertion (
Table 5). We modified several of the existing TRISS predictor variables in an aim to identify the most robust model via regression analysis. Although a more in-depth analysis could not be performed due to the insufficient sample size, we were able develop a model with a higher AUC value (0.888 vs. 0.913, respectively,
p value=0.003) than the existing TRISS model (MTOS-derived) simply by converting the "coded age" into a continuous value (
Table 6,
Fig. 3). This conversion was performed as our previous research on risk factors for trauma mortality showed that a continuous value of age could be a better predictor for trauma outcome while other converted values regarding SBP, RR, or GCS could not.
21 The model shows a greater explanatory power (R
2 of 0.408=40.8% vs. 38.0%, respectively) than the existing TRISS combination (coded age value, RTS, ISS), and the Hosmer-Lemeshow test results (χ
2=7.487,
p value=0.485) verified a good fit and calibration of the model (
Table 5). If such an encouraging result could be obtained with a single trauma care center's small-scale data, a more robust model may be identifiable through a study using multi-institutional data, such as the KTDB.
The current study had several limitations. Owing to the nature of TRISS, which is calculated by combining various predictor variables, a greater accumulation of data tends to result in a model with greater utility. However, the current study involved a small sample accumulated over a relatively short period of time, compared with other studies. Additionally, given that our medical center is a tertiary care center, the sample in the study may not have represented Korea's overall trauma patient population. Such a limitation has been frequently mentioned in other foreign TRISS studies as well.
1113141517 Furthermore, selection bias may have been a factor in cases where variables were not clearly defined. Nevertheless, although existing large-scale studies
121314 showed a large level of missing data (over 10%), the amount of missing data in the current study was relatively less at 5.2% (95 of 1841). In fact, the current study's sample, which was extracted from a single medical center, was treated by the same medical staff following the same protocol, and the fact that data entry also followed the same set of guidelines may have contributed to the increased homogeneity of the data, despite the small sample size. In order to address all of these limitations, randomized multi-institutional studies are needed. However, under the current Korean circumstances where the trauma database has only started to be established, much more time and effort will need to be invested first.
KTDB's benchmarking of the U.S. NTDB's format and the use of the Abbreviated Injury Scale (AIS), ISS, RTS, and TRISS as tools to estimate trauma outcome worldwide are inevitable under the current circumstances. However, as our circumstances differ from those of other countries that are 30–40 years ahead of us in terms of a trauma care system, a verification process using Korean data needs to precede the application of TRISS in evaluating trauma outcomes in Korea. Furthermore, Korean TRISS coefficients or a new prediction model suited for Korea needs to be developed using a sufficiently sized sample. Until then, the MTOS-derived TRISS model coefficients would be a realistic alternative. However, the requirement of a clear data dictionary that will ensure a certain level of quality in the data registered by all trauma care centers is more important than the question of which coefficient should be used.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download