Abstract
Purpose
Acute hepatitis A (AHA) and acute hepatitis B (AHB) are caused by an acute infection of the hepatitis A virus and the hepatitis B virus, respectively. In both AHA and AHB, liver injury is known to be mediated by immune cells and cytokines. In this study, we measured serum levels of various cytokines and T-cell cytotoxic proteins in patients with AHA or AHB to identify liver injury-associated cytokines.
Materials and Methods
Forty-six patients with AHA, 16 patients with AHB, and 14 healthy adults were enrolled in the study. Serum levels of 17 cytokines and T-cell cytotoxic proteins were measured by enzyme-linked immunosorbent assays or cytometric bead arrays and analyzed for correlation with serum alanine aminotransferase (ALT) levels.
Results
Interleukin (IL)-18, IL-8, CXCL9, and CXCL10 were significantly elevated in both AHA and AHB. IL-6, IL-22, granzyme B, and soluble Fas ligand (sFasL) were elevated in AHA but not in AHB. In both AHA and AHB, the serum level of CXCL10 significantly correlated with the peak ALT level. Additionally, the serum level of granzyme B in AHA and the serum level of sFasL in AHB correlated with the peak ALT level.
Hepatitis A virus (HAV) is a non-enveloped, single-stranded RNA virus of the Picornaviridae family.1 HAV infection is often asymptomatic in children. However, HAV infection in adults tends to result in acute hepatitis, called acute hepatitis A (AHA), one of the most common forms of acute viral hepatitis.234 In adult patients with AHA, severe liver injury and jaundice frequently develop and last for several weeks. However, AHA resolves spontaneously in most cases and does not progress to chronic viral hepatitis.5
Hepatitis B virus (HBV) is a partly double-stranded DNA virus that belongs to the Hepadnaviridae family.6 HBV infection is the most common form of chronic viral infection in the world, with more than 350 million people chronically infected.7 In endemic areas, chronic HBV infection is often established by vertical transmission.8 In adults, acute HBV infection causes acute hepatitis B (AHB), which is accompanied by liver injury and jaundice.89 Although AHB resolves spontaneously in most adult patients, some cases (1–5%) progress to chronic persistent infection.89
In both AHA and AHB, liver injury is known to be caused by T cells, not by the virus, because both HAV and HBV are non-cytopathic viruses.91011 Immune-mediated tissue injury, so-called immunopathology, is mediated by diverse mechanisms in different viral infections.12 The inflammatory process is mediated by cytokines, including interleukin (IL)-1β, IL-6, and tumor necrosis factor-α (TNF-α), and it is suppressed by IL-10.12 Additionally, helper 1 T (Th1) cells and helper 17 T (Th17) cells contribute to tissue injury by secreting cytokines; e.g., Th1 cells secrete interferon (IFN)-γ and TNF-α, and Th17 cells secrete IL-17 and IL-21.13 Moreover, cytotoxic T cells and natural killer (NK) cells directly lyse host cells through perforin/granzyme, and Fas ligand-mediated mechanisms.14 Chemokines are also involved in immune-mediated tissue injury by recruiting immune cells to the site of a viral infection.1516 However, in AHA and AHB, the exact mechanisms of immune-mediated liver injury remain to be elucidated.
In this study, we measured serum levels of 17 cytokines and T-cell cytotoxic proteins in patients with AHA and AHB in the acute phase to understand immunological mechanisms of liver injury in acute viral hepatitis, and identified cytokines or T-cell cytotoxic proteins associated with severe liver injury in AHA and AHB. The present study provides insight regarding which effector function of T cells contributes to liver injury in AHA and AHB.
Forty-six patients with AHA, 16 patients with AHB, and 14 healthy adults were recruited from hospitals in the Seoul metropolitan area (Seoul National University Bundang Hospital, Chung-Ang University Hospital, Bundang CHA Hospital, Seongnam Central Hospital, and Daejin Medical Center). AHA and AHB were diagnosed based on positive detection with anti-HAV IgM, and HBsAg and anti-HBc IgM, respectively, typical disease symptoms, and elevated serum alanine aminotransferase (ALT) levels. Peak ALT level and peak total bilirubin level were determined for each patient during the course of acute hepatitis. We obtained informed consent from participating subjects and study approval from the Institutional Review Boards. At the time of hospital admission, blood was drawn from patients, and serum samples were frozen for later analysis.
Eleven cytokines: IL-1β, IL-6, IL-10, IL-12p70, IL-18, IL-21, IL-22, IL-28, IL-29, IFN-γ, and TNF-α; and four chemokines: IL-8, CCL2 (monocyte chemoattractant protein-1), CXCL9 (monokine induced by IFN-γ), and CXCL10 (IFN-γ-inducible protein-10) were measured in this study. We also analyzed the serum levels of T-cell cytotoxic proteins, including granzyme B and soluble Fas ligand (sFasL). The serum levels of these proteins were measured with either enzyme-linked immunosorbent assay (ELISA) kits (IL-18, Abcam, Cambridge, UK; IL-22, R&D Systems, Minneapolis, MN, USA; and IL-28 and IL-29, RayBiotech Inc., Norcross, GA, USA) or cytometric bead array flex kits (BD Biosciences, San Jose, CA, USA).
Discrete variables were compared using the χ2 method, and independent t tests were used for continuous variables. Pearson or Spearman correlation analysis was used to determine simple correlations between continuous variables. All statistical analyses were performed with Statistical Product and Service Solutions 13.0. (SPSS Inc., Chicago, IL, USA).
Table 1 shows the demographic and laboratory characteristics of the study population. The median age of the AHA patients, AHB patients, and healthy controls were 33.6, 35.8, and 32.1 years, respectively. The average of peak ALT levels (IU/L) was 4450 in AHA patients and 1406 in AHB patients. The average of peak total bilirubin levels (mg/dL) was 5.1 in AHA patients and 9.6 in AHB patients.
Among the serum proteins analyzed, several were significantly elevated in serum samples from patients with AHA or AHB, compared to serum samples from healthy subjects. IL-18, IL-8, CXCL9, and CXCL10 were significantly elevated in both AHA and AHB, whereas IL-6, IL-22, granzyme B, and sFasL were significantly elevated in AHA, but not in AHB (Fig. 1).
Next, we analyzed which chemokines were associated with the degree of liver injury, assessing liver injury in terms of serum ALT levels. CXCL10 and CXCL9 are CXCR3 chemokines and known to be elevated frequently in systemic viral infections.17 Fig. 2 shows that CXCL10 levels were significantly correlated with peak ALT levels in both AHA and AHB, whereas the serum CXCL9 levels were correlated with peak ALT levels in AHA, but tended to correlate with peak ALT levels in AHB (Fig. 2B).
Next, we investigated which cytokines or T-cell cytotoxic proteins were associated with peak ALT levels. In AHA, serum granzyme B, but not serum sFasL, was significantly correlated with peak ALT levels (Fig. 3A). Conversely, in AHB, serum sFasL but not serum granzyme B was significantly correlated with peak ALT levels (Fig. 3B). In addition, the serum IL-18 levels significantly correlated with peak total bilirubin levels in AHA (Fig. 3C) but not in AHB (Fig. 3D). We also analyzed IL-22, a known hepatoprotective cytokine.181920 However, the serum IL-22 levels did not correlate with peak ALT levels in either AHA or AHB (data not shown).
In the present study, we found that the serum levels of IL-18, IL-8, CXCL9, and CXCL10 were elevated in AHA and AHB. In addition, the serum levels of IL-6, IL-22, granzyme B and sFasL were increased in AHA but not in AHB, indicating that AHA is accompanied by more vigorous immune responses compared to AHB. The levels of CXCR3 ligands, CXCL10 and CXCL9 correlated with peak ALT levels in AHA and AHB. Moreover, serum granzyme B levels correlated with peak ALT levels in AHA, and serum sFasL levels correlated with peak ALT levels in AHB. These findings together suggest that effector functions of T cells are elevated and contribute to liver injury in AHA and AHB.
CXCR3 and its ligand chemokines regulate the migration of Th1 cells and effector CD8+ T cells into infection sites during various human and murine acute viral infections, such as influenza,21 dengue,22 and West Nile virus infection.23 In viral hepatitis, CXCR3 chemokines have been studied, particularly in hepatitis C virus (HCV) infection. CXCR3 chemokines are detected in the peripheral blood 2–8 weeks after HCV infection.242526 The expression level of CXCR3 chemokines in the liver or the peripheral blood correlated well with the severity of hepatic inflammation in patients with chronic HCV infection.27282930 In ch-ronic HBV infection, it was demonstrated that serum CXCL10 and CXCL9 levels are associated with the acute flare-up of liver injury.31 Consistent with these reports, our data from the sera of AHA and AHB patients demonstrated that CXCR3 chemokines are increased during AHA and AHB, and that their levels correlate with liver damage, thus implying that they might play an important role in liver injury.
Notably, our present data also showed that serum granzyme B levels correlated with peak ALT levels in AHA (Fig. 3A), and that serum sFasL levels correlated with peak ALT levels in AHB (Fig. 3B). The correlation between serum sFasL and serum ALT levels was previously reported in self-limited AHB and fulminant hepatitis B.32 CD8+ cytotoxic T cells and NK cells can contribute to liver injury by target cell-killing activity. When these cells are triggered, they exert cytotoxic activity through two different mechanisms: degranulation of perforin and granzymes, and upregulation of FasL on their cell surface.33 The current findings indicate that a distinct cytotoxic mechanism might contribute to hepatocyte destruction in AHA and AHB.
In the present study, we examined serum levels of cytokines and T-cell cytotoxic proteins to evaluate immune responses during AHA and AHB. However, we did not examine immune cells such as T cells and NK cells, therefore, we do not know yet which subsets of immune cells produce the cytokines and cytotoxic proteins that are increased in the sera of AHA and AHB patients. Future studies should investigate the expression levels of cytokines and cytotoxic proteins in T cells and NK cells obtained from patients with AHA or AHB.
Recently, the levels of multiple serum proteins were systematically analyzed in blood drawn from patients with AHA, AHB, and acute hepatitis C.34 However, that study did not consider the levels of serum proteins relative to the degree of liver injury. In the present study, we compared the associations between liver injury and cytokines, chemokines, and T-cell cytotoxic proteins in AHA and AHB. Our present findings led us to propose that distinct immunological mechanisms of liver injury might operate in AHA and AHB. The exact mechanisms of liver injury require further investigation at the cellular and molecular levels in acute viral hepatitis.
Figures and Tables
 | Fig. 1Serum levels of cytokines, chemokines, and T-cell cytotoxic proteins in AHA and AHB. The data represent the serum proteins that were elevated in patients with AHA or AHB compared to healthy controls. Horizontal lines indicate mean values; n=46 for AHA, n=16 for AHB, and n=14 for healthy controls. p values are presented as *p<0.01 or †p<0.001, based on the unpaired Student's t-test. IL, interleukin; AHA, acute hepatitis A; AHB, acute hepatitis B. |
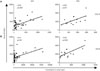 | Fig. 2Correlation between the serum levels of CXCR3 chemokines and the degree of liver injury. Serum concentrations of CXCL10 (A) and CXCL9 (B) correlated to peak ALT levels in samples drawn from patients with AHA (left) or AHB (right). Correlation coefficients (r) are based on Pearson (AHA) or Spearman (AHB) analyses. p values <0.05 are considered statistically significant. AHA, acute hepatitis A; AHB, acute hepatitis B; ALT, alanine aminotransferase. |
 | Fig. 3Correlation between the serum levels of cytokines or T-cell cytotoxic proteins and the degree of liver injury. Serum concentrations of granzyme B (left), sFasL (center), or IL-18 (right) correlated to peak ALT levels (A and B) or peak total bilirubin levels (C and D) in samples drawn from patients with AHA (A and C) or AHB (B and D). Correlation coefficients (r) are based on Pearson (AHA) or Spearman (AHB) analyses. p values<0.05 are considered statistically significant. n.s., non-significant; sFasL, soluble Fas ligand; IL, interleukin; AHA, acute hepatitis A; AHB, acute hepatitis B; ALT, alanine aminotransferase. |
Table 1
Demographic and Laboratory Characteristics of the Study Population

ACKNOWLEDGEMENTS
This study was supported by a grant from the Korea Health Technology R&D Project of the Ministry of Health & Welfare, Republic of Korea (HI13C1263) and by a grant from the SNUBH Research Fund (03-2011-010).
References
1. Chung SJ, Kim TY, Kim SM, Roh M, Yu MY, Lee JH, et al. Changes in the seroprevalence of IgG anti-hepatitis A virus between 2001 and 2013: experience at a single center in Korea. Clin Mol Hepatol. 2014; 20:162–167.

2. Wasley A, Fiore A, Bell BP. Hepatitis A in the era of vaccination. Epidemiol Rev. 2006; 28:101–111.

3. Franco E, Meleleo C, Serino L, Sorbara D, Zaratti L. Hepatitis A: epidemiology and prevention in developing countries. World J Hepatol. 2012; 4:68–73.

4. Collier MG, Tong X, Xu F. Hepatitis A hospitalizations in the United States, 2002-2011. Hepatology. 2015; 61:481–485.

6. Seeger C, Mason WS. Molecular biology of hepatitis B virus infection. Virology. 2015; 479-480:672–686.

7. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2095–2128.
9. Rehermann B, Nascimbeni M. Immunology of hepatitis B virus and hepatitis C virus infection. Nat Rev Immunol. 2005; 5:215–229.

10. Guidotti LG, Chisari FV. Immunobiology and pathogenesis of viral hepatitis. Annu Rev Pathol. 2006; 1:23–61.

11. Walker CM, Feng Z, Lemon SM. Reassessing immune control of hepatitis A virus. Curr Opin Virol. 2015; 11:7–13.

12. Rouse BT, Sehrawat S. Immunity and immunopathology to viruses: what decides the outcome. Nat Rev Immunol. 2010; 10:514–526.

13. Weaver CT, Hatton RD, Mangan PR, Harrington LE. IL-17 family cytokines and the expanding diversity of effector T cell lineages. Annu Rev Immunol. 2007; 25:821–852.

14. Williams MA, Bevan MJ. Effector and memory CTL differentiation. Annu Rev Immunol. 2007; 25:171–192.

15. Allen SJ, Crown SE, Handel TM. Chemokine: receptor structure, interactions, and antagonism. Annu Rev Immunol. 2007; 25:787–820.
16. Marra F, Tacke F. Roles for chemokines in liver disease. Gastroenterology. 2014; 147:577–594.e1.

17. Groom JR, Luster AD. CXCR3 ligands: redundant, collaborative and antagonistic functions. Immunol Cell Biol. 2011; 89:207–215.

18. Radaeva S, Sun R, Pan HN, Hong F, Gao B. Interleukin 22 (IL-22) plays a protective role in T cell-mediated murine hepatitis: IL-22 is a survival factor for hepatocytes via STAT3 activation. Hepatology. 2004; 39:1332–1342.

19. Park O, Wang H, Weng H, Feigenbaum L, Li H, Yin S, et al. In vivo consequences of liver-specific interleukin-22 expression in mice: implications for human liver disease progression. Hepatology. 2011; 54:252–261.

20. Xing WW, Zou MJ, Liu S, Xu T, Gao J, Wang JX, et al. Hepatoprotective effects of IL-22 on fulminant hepatic failure induced by d-galactosamine and lipopolysaccharide in mice. Cytokine. 2011; 56:174–179.

21. Fadel SA, Bromley SK, Medoff BD, Luster AD. CXCR3-deficiency protects influenza-infected CCR5-deficient mice from mortality. Eur J Immunol. 2008; 38:3376–3387.

22. Hsieh MF, Lai SL, Chen JP, Sung JM, Lin YL, Wu-Hsieh BA, et al. Both CXCR3 and CXCL10/IFN-inducible protein 10 are required for resistance to primary infection by dengue virus. J Immunol. 2006; 177:1855–1863.

23. Klein RS, Lin E, Zhang B, Luster AD, Tollett J, Samuel MA, et al. Neuronal CXCL10 directs CD8+ T-cell recruitment and control of West Nile virus encephalitis. J Virol. 2005; 79:11457–11466.

24. Shin EC, Park SH, Demino M, Nascimbeni M, Mihalik K, Major M, et al. Delayed induction, not impaired recruitment, of specific CD8+ T cells causes the late onset of acute hepatitis C. Gastroenterology. 2011; 141:686–695.

25. Kang W, Shin EC. Clinical implications of chemokines in acute and chronic hepatitis C virus infection. Yonsei Med J. 2011; 52:871–878.

26. Grebely J, Feld JJ, Applegate T, Matthews GV, Hellard M, Sherker A, et al. Plasma interferon-gamma-inducible protein-10 (IP-10) levels during acute hepatitis C virus infection. Hepatology. 2013; 57:2124–2134.

27. Harvey CE, Post JJ, Palladinetti P, Freeman AJ, Ffrench RA, Kumar RK, et al. Expression of the chemokine IP-10 (CXCL10) by hepatocytes in chronic hepatitis C virus infection correlates with histological severity and lobular inflammation. J Leukoc Biol. 2003; 74:360–369.

28. Helbig KJ, Ruszkiewicz A, Semendric L, Harley HA, McColl SR, Beard MR. Expression of the CXCR3 ligand I-TAC by hepatocytes in chronic hepatitis C and its correlation with hepatic inflammation. Hepatology. 2004; 39:1220–1229.

29. Zeremski M, Petrovic LM, Chiriboga L, Brown QB, Yee HT, Kinkhabwala M, et al. Intrahepatic levels of CXCR3-associated chemokines correlate with liver inflammation and fibrosis in chronic hepatitis C. Hepatology. 2008; 48:1440–1450.

30. Apolinario A, Majano PL, Alvarez-Pérez E, Saez A, Lozano C, Vargas J, et al. Increased expression of T cell chemokines and their receptors in chronic hepatitis C: relationship with the histological activity of liver disease. Am J Gastroenterol. 2002; 97:2861–2870.

31. Tan AT, Koh S, Goh W, Zhe HY, Gehring AJ, Lim SG, et al. A longitudinal analysis of innate and adaptive immune profile during hepatic flares in chronic hepatitis B. J Hepatol. 2010; 52:330–339.

32. Shiota G, Oyama K, Noguchi N, Takano Y, Kitaoka S, Kawasaki H. Clinical significance of serum soluble Fas ligand in patients with acute self-limited and fulminant hepatitis. Res Commun Mol Pathol Pharmacol. 1998; 101:3–12.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download