Abstract
Purpose
The association between the red cell distribution width (RDW) and vasospastic angina (VSA) has not been elucidated. We investigated the association of the RDW with the incidence and angiographic subtypes of VSA in Korean patients.
Materials and Methods
A total of 460 patients who underwent intracoronary ergonovine provocation tests were consecutively enrolled and classified into two groups: the VSA group (n=147, 32.0%) and non-VSA group (n=313, 68.0%). The subjects were classified into 3 subgroups (tertiles) according to the baseline level of RDW assessed before the angiographic provocation test.
Results
The VSA group had a higher RDW than the non-VSA group (12.9±0.8% vs. 12.5±0.7%, p=0.013). The high RDW level demonstrated an independent association with the high incidence of VSA [second tertile: hazard ratio (HR) 1.96 (1.13–2.83), third tertile: HR 2.33 (1.22–3.47), all p<0.001]. Moreover, the highest RDW tertile level had a significant association with the prevalence of the mixed-type coronary spasm [HR 1.29 (1.03–1.59), p=0.037].
Coronary spasm is an important factor in the pathogenesis of ischemic cardiovascular disease (CVD), particularly among Asians.1 The long-term prognosis of vasospastic angina (VSA) is relatively benign.12 However, conventional medical treatments including vasodilators are often ineffective and sometimes lead to fatal arrhythmias.12 Several diagnostic methods have been introduced, and angiographic provocation with acetylcholine or ergonovine is the most frequently used, as recent Japanese multicenter studies23 demonstrated an acceptable level of safety during provocation tests. Although angiographic provocation for VSA is widely performed in Korea and Japan, some clinicians still focus only on atherosclerotic stenosis, with less emphasis on coronary spasm.123 Therefore, it is important not only to induce a great clinical interest on VSA in clinicians, but also to find reliable markers for screening patients who may need a proactive clinical investigation including angiographic provocation test.24
The red cell distribution width (RDW) reflects the variability in the size of red blood cells (RBC) and has been used in the differential diagnosis of anemia.567 Interestingly, the RDW has been reported as a strong predictor of the incidence and prognosis in a wide spectrum of CVD.678910 The mechanism for the association between an elevated RDW and the incidence and clinical outcomes of CVD is still unclear. However, recent studies suggested that an interaction between chronic inflammatory responses, oxidative stress, and endothelial dysfunction, which have been reported as the pathophysiology of coronary spasms, might explain this association.1112
Despite the similar pathophysiological relevance between an elevated RDW and coronary spasm, the relationship between the RDW and VSA has not been elucidated. Therefore, we aimed to investigate the association of the RDW with the incidence and angiographic subtypes of VSA in Korean patients.
The patients who had suspicious symptoms and underwent the angiographic intracoronary ergonovine provocation test for VSA, according to the clinician's decision at three cardiovascular centers (Incheon St. Mary's, Daejeon St. Mary's, and Seoul St. Mary's Hospitals, The Catholic University of Korea) from July 2013 to September 2014, were consecutively enrolled in this analysis. During the study period, we assessed the baseline RDW before coronary angiography (CAG) in all enrolled patients. All these participating centers have performed the high-volume CAG (>1200 cases/year) and have used the same study protocol for the intracoronary ergonovine provocation test.
A total of 460 patients were consecutively included into two groups: the VSA group (n=147, 32.0%) and non-VSA group (n=313, 68.0%). All enrolled patients had normal findings or minimal (<50% of luminal narrowing) atherosclerosis on the baseline CAG. Meanwhile, the patients with significant atherosclerosis (≥50%), renal failure on continuous dialysis, and malignant or inflammatory diseases were excluded. We compared the baseline characteristics between the two groups and investigated the association between the RDW and VSA.
The study protocol of this three-center observational study was approved by the institutional review board of each participating center.
The Guidelines for Diagnosis and Treatment of Patients with VSA of the Japanese Circulation Society was used in the diagnosis of VSA.13 The baseline CAG was performed for the right coronary artery (RCA) and the left coronary artery (LCA) after an intracoronary injection of normal saline (5 mL). If there was no significant atherosclerosis on the baseline CAG, incremental doses of 20 µg, 40 µg, and 60 µg of ergonovine were injected into the LCA. If coronary spasm was not provoked in the LCA, incremental doses of (10 µg), 20 µg, and 40 µg were injected into the RCA. Once spasm was provoked, intracoronary nitrates was injected to resolve spasm immediately. Medications that affect vasomotion were discontinued at least 48 hours before CAG.
The baseline level of the RDW was determined before the provocation test using the Sysmex XE-2100 Hematology Analyzer (Sysmex, Kobe, Japan), as part of the routine hemogram.
The definition of a positive result in the ergonovine provocation test was a total or subtotal (>90% of luminal diameter narrowing) occlusion with ischemic symptoms and/or electrocardiographic (ECG) changes (the VSA group).13 Patients who did not meet the positive criteria were included in the non-VSA group. All responses to ergonovine and atherosclerosis on the baseline CAG were quantitatively analyzed by clinicians blinded to patient status.
An ischemic ECG change was defined as an ST-elevation or depression of ≥0.1 mV or T-inversion or a negative U-wave in at least two related leads.1 A multivessel spasm was defined as a positive spasm in more than two major (≥2.5 mm of vessel diameter) epicardial coronary arteries. A focal-type spasm was defined as a discrete spasm localized in one coronary segment, while a spasm observed continuously from the proximal to the distal segment was defined as a diffuse-type spasm. In addition, a multivessel spasm in which at least one coronary artery had a diffuse-type and the other had a focal-type was defined as the mixed-type spasm.3 Anemia was defined as a hemoglobin level of <12.0 g/dL in women and <13.0 g/dL in men.14
Continuous variables were presented as mean±standard deviation and categorical variables were presented as numbers and percentage. The Student's t-test was used for continuous variables and categorical variables were compared using the chi-square or Fisher's exact test. All enrolled patients were classified into three groups (tertiles) according to the baseline RDW to determine the association between the RDW and the incidence of VSA. Additionally, the patients in the VSA group were reclassified into tertiles according to the baseline RDW to evaluate the impact of the RDW on the angiographic subtypes of VSA. The prevalence and angiographic characteristics of VSA were compared among the groups using the Kruskal-Wallis test. A multivariate logistic regression analysis was performed to identify independent predictors. Variables with a p<0.20 in the univariate were entered into a multivariate analysis. The hazard ratio (HR) and 95% confidence intervals (95% CI) were also calculated. A p value of <0.05 was considered to be significant. All analyses were performed using SPSS statistical software (version 18.0, SPSS Inc., Chicago, IL, USA).
The baseline clinical and laboratory characteristics are presented in Tables 1 and 2. The incidence of males and current smokers was significantly higher in the VSA group (p<0.05). The VSA group also demonstrated higher levels of high-sensitivity C-reactive protein (hsCRP) and triglyceride (TG) than the non-VSA group (p<0.05). Although the other hematologic findings, renal and thyroid function, prevalence of anemia, and medication history were very similar between the groups, the baseline RDW was significantly higher in the VSA group (12.9±0.8% vs. 12.5±0.7%, p=0.013) (Table 2).
All patients in the VSA and non-VSA groups were subclassified according to the baseline RDW to evaluate the association of the RDW with the incidence of VSA: <12.2% (n=162, first tertile), 12.2–12.8% (n=153, second tertile), >12.8% (n=145, third tertile).
The RDW level was closely associated with the incidence of VSA, and patients in the third RDW tertile showed the highest incidence of VSA (p<0.001) (Fig. 1). Moreover, in the multivariate logistic regression analysis, a high RDW [second tertile: HR 1.96, 95% CI (1.13–2.83), third tertile: 2.33 (1.22–3.47), all p<0.001] was revealed as an independent predictor of VSA. Current smoking [2.52 (1.21–3.79), p=0.007] and the TG level [1.29 (1.12–1.50), p=0.032] were additional independent predictors for VSA (Table 3).
In the VSA group (n=147), the mixed-type spasm was seen in 40 patients (27.2%), while non-mixed type including the diffuse-type (79, 53.7%) and the focal-type (28, 19.0%) was provoked in 107 patients. Ninety-two patients (62.6%) had single vessel spasm and multivessel spasm was observed in 55 patients (37.4%).
The patients in the VSA group were further classified according to the baseline RDW to evaluate the association between the RDW and the angiographic characteristics of VSA: <12.6% (n=48, first tertile), 12.6–13.1% (n=50, second tertile), >13.1% (n=49, third tertile). The distribution of single vessel and multivessel spasm were very similar among tertile groups (p=0.411), while the mixed-type and non-mixed type were differently distributed among the groups (p=0.028) (Table 4). The mixed-type was the most frequently provoked in the third tertile (45.0%). Meanwhile, the focal-type was observed in 11 patients (39.3%) in the first tertile, 9 (32.1%) in the second tertile, and 8 (28.6%) in the third tertile group. Twenty-eight patients (35.4%) in the first tertile, 28 (35.4%) in the second tertile, and 23 (29.1%) in the third tertile groups demonstrated the diffuse-type. In the logistic regression analysis, the second tertile level of the RDW demonstrated no significant statistical interaction with the mixed-type spasm. However, the third tertile group of the RDW had an independent association with the prevalence of the mixed-type coronary spasm [1.29 (1.03–1.59), p=0.037] (Table 5).
In the present analysis, we demonstrated that an elevated RDW had an independent association with the prevalence of VSA in Korean patients. The high RDW was not only an independent predictor for VSA, but was also associated with the mixed-type spasm which has been reported to be associated with adverse clinical outcomes in VSA patients.3
The RDW is a simple and inexpensive parameter that reflects the degree of heterogeneity of RBC, and is traditionally used for the differential diagnosis of anemia.6715 However, recent studies have demonstrated the association between the RDW and a wide spectrum of CVDs including heart failure, coronary artery disease, pulmonary-thromboembolism, and peripheral artery disease.678910 Nevertheless, few reports have detailed an association between the RDW and coronary spasm, even though VSA is one of the most important functional coronary diseases, especially in East Asians. To the best of our knowledge, this is the first report demonstrating a close association between the RDW and the prevalence and angiographic characteristics of VSA in Korean patients.
An elevated RDW indicates a profound deregulation of RBC homeostasis and can be attributed to a variety of underlying metabolic conditions including aging, oxidative stress, inflammation, and poor nutritional status. Moreover, the RDW is influenced by underlying pathologies including anemia, diabetes, hypertension, cancer, and thyroid and renal dysfunction, which induce RBC fragmentation.111215 In the present analysis, both VSA and non-VSA groups had similar characteristics in age, prevalence of diabetes and hypertension, cardiac, thyroid and renal function, and the incidence of anemia, and patients with renal failure on dialysis and malignant or inflammatory diseases, which can affect the RDW, were excluded. However, the factors which can influence the RDW may be innumerable.15 In our analysis, the VSA group demonstrated the higher prevalence of male and current smokers than the non-VSA group. It has been reported that the RDW level could be elevated in male or smokers.1617 Although the multivariate regression analysis including gender and current smoking demonstrated that the high level of RDW was one of independent predictors for the incidence of VSA, it is still possible to assume that these factors played a role as confounding factors in our analysis.
The precise mechanism for the relationship between an elevated RDW and the high prevalence of VSA remains unclear. However, an elevated RDW could reflect increased inflammatory responses and oxidative stress, and is also associated with impaired endothelial function.1112151819 Förhécz, et al.11 reported that the RDW is associated with various inflammatory markers including interleukin-6 (IL-6) and tumor necrosis factor (TNF) receptors I and II, and CRP. And Semba, et al.18 also suggested that oxidative stress, conjugated with inflammation, might significantly increase the RDW. Interestingly, chronic inflammation and increased oxidative stress are important factors in the pathogenesis of coronary spasm.24 Oxygen free radicals could degrade nitric-oxide, the most potent endothelium-dependent vasodilator, causing vasoconstriction.2 Moreover, the levels of adhesion molecules such as P-selection and hsCRP, a sensitive marker of inflammation, were also increased in patients with VSA.20 In addition, smoking, a crucial risk factor for VSA, is associated with chronic inflammation.12 These findings suggest that chronic inflammation may simultaneously contribute to the pathogenesis of an elevated RDW and VSA. In our results, the VSA group had a higher hsCRP and higher number of current smokers than the non-VSA group. However, in the multivariate analysis, the level of hsCRP demonstrated only a trend of association with VSA (p=0.075), although current smoking was revealed as an independent predictor for VSA (p=0.007). Moreover, various parameters for inflammation or oxidative stress could not be estimated and we only assessed the baseline hsCRP. Thus, the patient's inflammatory status could not be precisely determined in the present analysis. Further studies should be conducted to clearly determine the association of the inflammatory status or oxidative stress with the RDW and VSA.
Recently, an elevated RDW was reported to be independently associated with systemic endothelial dysfunction, assessed by microalbuminuria and flow-mediated dilation (FMD).1219 Endothelial dysfunction is involved in every stage of atherosclerosis as well as in the development of VSA. Moreover, early changes in atherosclerosis may also induce coronary spasm.1221 Considering these previous results, endothelial dysfunction may also contribute to the similarity in the pathological relevance between an elevated RDW and VSA. In the present analysis, however, we did not assess the parameter for endothelial function and could not demonstrate the direct association between the RDW and endothelial dysfunction. Further studies including the markers for endothelial function would be helpful for precisely determining the relationship between the RDW and VSA.
Different patterns of angiographic changes in response to ergonovine or acetylcholine, including the diffuse- and focal-types, have been prescribed.322 The focal-type spasm may be closely associated with an increased coronary intima-media thickness and relatively advanced atherosclerosis. Meanwhile, the diffuse-type was induced by more extensive endothelial dysfunction.2322 Although the prognosis of VSA according to the subtypes could be controversial,2223 a nation-wide Japanese study group recently suggested that the mixed-type spasm, which might share features of both focal- and diffuse-types, was independently associated with a poor prognosis in VSA patients. They demonstrated a significant impact of the mixed multivessel spasm on adverse events, while other types such as including focal or diffuse single-vessel and focal or diffuse multivessel spasm had no correlation with adverse clinical outcomes.3 Our present analysis provided the novel finding that the highest RDW level had a significant association with the prevalence of the mixed-type spasm. Although the precise me-chanism for this association between the RDW and this high-risk angiographic subtype still remains unclear, our result could highlight the importance of paying more clinical attention to the VSA patients with an elevated RDW for future adverse cardiovascular events.
In the present study, we demonstrated that a high TG was also an independent predictor for VSA, although the association between the RDW and the level of TG was not clearly defined. In a hyper-TG state, the expression of adhesion molecules, cytotoxic inflammation, and foam cell formation are enhanced. Therefore, the high level of TG can cause endothelial dysfunction and accelerated atherosclerosis due to an increase of in small dense low-density lipoprotein cholesterol and a reduction of high-density lipoprotein cholesterol.2425 In previous studies, the high TG was not only significantly related to an increased basal coronary tone, which is related to the activity of VSA, but was also a predictor for multivessel spasm.2223 Consequently, meticulous clinical attention should be paid to patients with an elevated TG, in addition to other known risk factors such as smoking.
The clinical prognosis of VSA is relatively good. Moreover, the prevalence worldwide appears to have declined, which may be attributable to cessation of smoking and more frequent use of calcium-channel blockers.1223 Thus, clinical interest in atherosclerotic stenosis and coronary intervention is growing among clinicians, while less attention is being paid to VSA.2 Nevertheless, VSA is still prevalent and some patients are refractory to conventional medications.12 Thus, it is necessary to find reliable markers for screening patients who could benefit from a proactive investigation including angiographic provocation. Recently, the advanced understanding of the pathogenesis of VSA has resulted in new possible markers including IL-6, intercellular adhesion molecule-1, nitrotyrosine, and lipoprotein(a).42627 However, our present analysis indicated that the RDW, which has been known as a comprehensive marker of inflammation, oxidative stress, and endothelial dysfunction, showed a close association with VSA in Korean patients.
Several limitations should be noted. First, this analysis used data from an observational study, which has inherent limitations. Second, this analysis was originally designed as a cross-sectional study. Thus, the relationship between the RDW and long-term outcomes was not determined. Third, there still may be possible confounding factors such as gender and smoking, and also several biases in the selection of patients, most likely due to the relatively small study population. However, all patients who underwent the angiographic ergonovine provocation during the study period were consecutively enrolled in this analysis. Especially, the relatively high prevalence of female patients in the non-VSA group could be associated with the possibility of a selection bias. Finally, in our study, hsCRP was the only parameter for inflammation to unravel the association between the RDW and VSA. Moreover, we did not investigate other surrogate markers of chronic inflammation and endothelial dysfunction, including IL-6, TNF, P-selectin, microalbuminuria, and FMD. The assessment of these parameters would be helpful in clarifying the precise mechanism of association between the RDW and VSA. Despite these limitations, our results emphasize the importance of understanding the association of an elevated RDW with the prevalence and angiographic subtypes of VSA.
In conclusion, the high RDW was significantly associated with the prevalence of VSA and the high-risk angiographic subtype of coronary spasm, consequently emphasizing the clinical value of a proactive clinical investigation of VSA in Korean patients with an elevated RDW.
Figures and Tables
Fig. 1
Incidence of VSA according to the baseline RDW. The baseline RDW demonstrates a significant association with the incidence of VSA. VSA, vasospastic angina; RDW, red cell distribution width.
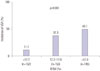
Table 1
Baseline Clinical Characteristics

Table 2
Baseline Laboratory Characteristics

Table 3
Independent Predictors of VSA

VSA, vasospastic angina; HR, hazard ratio; CI, confidence interval; ARB, angiotensin receptor blocker; ACEi, angiotensin converting enzyme inhibitor; WBC, white blood cell; HDL, high density lipoprotein; hsCRP, high-sensitivity C-reactive protein; RDW, red cell distribution width.
*The max-rescaled R-square: 0.3808.
Table 4
Association between the Baseline RDW and Angiographic Characteristics in the VSA Group

ACKNOWLEDGEMENTS
We acknowledge the valuable support of Ji-Hoon Jung, MA in the statistical analysis.
References
1. Shin DI, Baek SH, Seo SM, Koh YS, Choi YS, Kim DB, et al. Rates of coronary intervention due to de novo significant atherosclerosis and cardiac death are very low in Korean patients with vasospastic angina: 36-month follow-up results of the Vasospastic Angina in the Catholic Medical Center (VA-CMC) registry. Circ J. 2012; 76:2681–2689.

2. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm--clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008; 51:2–17.

3. Takagi Y, Yasuda S, Takahashi J, Tsunoda R, Ogata Y, Seki A, et al. Clinical implications of provocation tests for coronary artery spasm: safety, arrhythmic complications, and prognostic impact: multicentre registry study of the Japanese Coronary Spasm Association. Eur Heart J. 2013; 34:258–267.

4. Hung MJ, Cherng WJ, Cheng CW, Li LF. Comparison of serum levels of inflammatory markers in patients with coronary vasospasm without significant fixed coronary artery disease versus patients with stable angina pectoris and acute coronary syndromes with significant fixed coronary artery disease. Am J Cardiol. 2006; 97:1429–1434.

5. Demirkol S, Balta S, Cakar M, Unlu M, Arslan Z, Kucuk U. Red cell distribution width: a novel inflammatory marker in clinical practice. Cardiol J. 2013; 20:209.
6. Arbel Y, Shacham Y, Finkelstein A, Halkin A, Milwidsky A, Berliner S, et al. Red blood cell distribution width (RDW) and long-term survival in patients with ST elevation myocardial infarction. Thromb Res. 2014; 134:976–979.

7. Felker GM, Allen LA, Pocock SJ, Shaw LK, McMurray JJ, Pfeffer MA, et al. Red cell distribution width as a novel prognostic marker in heart failure: data from the CHARM Program and the Duke Databank. J Am Coll Cardiol. 2007; 50:40–47.

8. Hong SJ, Youn JC, Oh J, Hong N, Lee HS, Park S, et al. Red cell distribution width as an independent predictor of exercise intolerance and ventilatory inefficiency in patients with chronic heart failure. Yonsei Med J. 2014; 55:635–643.

9. Zorlu A, Bektasoglu G, Guven FM, Dogan OT, Gucuk E, Ege MR, et al. Usefulness of admission red cell distribution width as a predictor of early mortality in patients with acute pulmonary embolism. Am J Cardiol. 2012; 109:128–134.

10. Zalawadiya SK, Veeranna V, Panaich SS, Afonso L. Red cell distribution width and risk of peripheral artery disease: analysis of National Health and Nutrition Examination Survey 1999-2004. Vasc Med. 2012; 17:155–163.

11. Förhécz Z, Gombos T, Borgulya G, Pozsonyi Z, Prohászka Z, Jánoskuti L. Red cell distribution width in heart failure: prediction of clinical events and relationship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am Heart J. 2009; 158:659–666.

12. Afonso L, Zalawadiya SK, Veeranna V, Panaich SS, Niraj A, Jacob S. Relationship between red cell distribution width and microalbuminuria: a population-based study of multiethnic representative US adults. Nephron Clin Pract. 2011; 119:c277–c282.

13. JCS Joint Working Group. Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Circ J. 2010; 74:1745–1762.
14. Tanne D, Molshatzki N, Merzeliak O, Tsabari R, Toashi M, Schwammenthal Y. Anemia status, hemoglobin concentration and outcome after acute stroke: a cohort study. BMC Neurol. 2010; 10:22.

15. Montagnana M, Cervellin G, Meschi T, Lippi G. The role of red blood cell distribution width in cardiovascular and thrombotic disorders. Clin Chem Lab Med. 2011; 50:635–641.

16. Zalawadiya SK, Veeranna V, Panaich SS, Afonso L, Ghali JK. Gender and ethnic differences in red cell distribution width and its association with mortality among low risk healthy United state adults. Am J Cardiol. 2012; 109:1664–1670.

17. Kurtogğlu E, Aktürk E, Korkmaz H, Sincer I, Yılmaz M, Erdem K, et al. Elevated red blood cell distribution width in healthy smokers. Turk Kardiyol Dern Ars. 2013; 41:199–206.

18. Semba RD, Patel KV, Ferrucci L, Sun K, Roy CN, Guralnik JM, et al. Serum antioxidants and inflammation predict red cell distribution width in older women: the Women's Health and Aging Study I. Clin Nutr. 2010; 29:600–604.

19. Solak Y, Yilmaz MI, Saglam M, Caglar K, Verim S, Unal HU, et al. Red cell distribution width is independently related to endothelial dysfunction in patients with chronic kidney disease. Am J Med Sci. 2014; 347:118–124.

20. Kaikita K, Ogawa H, Yasue H, Sakamoto T, Suefuji H, Sumida H, et al. Soluble P-selectin is released into the coronary circulation after coronary spasm. Circulation. 1995; 92:1726–1730.

21. Cho SH, Jeong MH, Park IH, Choi JS, Yoon HJ, Kim KH, et al. Endothelial dysfunction, increased carotid artery intima-media thickness and pulse wave velocity, and increased level of inflammatory markers are associated with variant angina. J Cardiol. 2009; 54:183–191.

22. Sato K, Kaikita K, Nakayama N, Horio E, Yoshimura H, Ono T, et al. Coronary vasomotor response to intracoronary acetylcholine injection, clinical features, and long-term prognosis in 873 consecutive patients with coronary spasm: analysis of a single-center study over 20 years. J Am Heart Assoc. 2013; 2:e000227.
23. Park YM, Han SH, Ko KP, Koh KK, Kang WC, Lee K, et al. Diffuse multi-vessel coronary artery spasm: incidence and clinical prognosis. Int J Cardiol. 2013; 167:398–402.

24. Yun KH, Shin SN, Ko JS, Rhee SJ, Kim NH, Oh SK, et al. Coronary artery responsiveness to ergonovine provocation in patients without vasospatic angina: a quantitative coronary angiography analysis. Int Heart J. 2011; 52:338–342.

25. Yu KC, Cooper AD. Postprandial lipoproteins and atherosclerosis. Front Biosci. 2001; 6:D332–D354.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download