Abstract
Purpose
The effects on the side-branch (SB) ostium, following paclitaxel-coated balloon (PCB) treatment of de novo coronary lesions of main vessels have not been previously investigated. This study was aimed at evaluating the serial morphological changes of the SB ostium after PCB treatment of de novo coronary lesions of main vessels using optical coherence tomography (OCT).
Materials and Methods
This prospective, single-center observational study enrolled patients with de novo lesions, which were traversed by at least one SB (≥1.5 mm) and were treated with PCB. The SB ostium was evaluated with serial angiographic and OCT assessments pre- and post-procedure, and at 9-months follow-up.
Results
Sixteen main vessel lesions were successfully treated with PCB, and 26 SBs were included for analysis. Mean SB ostial lumen
area increased at 9-months follow-up (0.92±0.68 mm2 pre-procedure, 1.03±0.77 mm2 post-procedure and 1.42±1.18 mm2 at 9-months). The SB ostial lumen area gain was 0.02±0.24 mm2 between pre- and post-procedure, 0.37±0.64 mm2 between post-procedure and 9-months, and 0.60±0.93 mm2 between pre-procedure and 9-months. The ostial lumen area increased by 3.9% [interquartile range (IQR) of -33.3 to 10.4%] between pre- and post-procedure, 52.1% (IQR of -0.7 to 77.3%) between post-procedure and 9-months and 76.1% (IQR of 18.2 to 86.6%) between pre-procedure and 9-months.
In bifurcated lesions, current knowledge and experience suggest that treating lesions of the main vessel with a drug-eluting stent (DES) produces reasonable results, however, only suboptimal results in adjacent side-branches (SB).12 Functional compromise of the SB also occurs in 15–20% of cases following stent implantation in the main vessel of non-true bifurcation lesions.3 Stenting of bifurcation lesions is associated with some disadvantages, such as overstretching of the distal vessel and straightening of the vessel, both leading to a carina shift into the SB.4 Despite seemingly better flow conditions in the straightened main vessel, the end result is actually a compromise induced by the adjacent SB.5
Non-stent based local drug delivery using paclitaxel-coated balloon (PCB) has recently emerged as a new treatment modality for coronary artery disease.6 Proposed advantages of PCB include a homogeneous drug delivery to the vessel wall, an immediate drug release without the use of a polymer, the potential of reducing the intensity and duration of antiplatelet therapy, and the absence of residual foreign material in the vessel.4 The effects on the SB ostium following PCB treatment of de novo lesions of main vessels have not been previously investigated. The aim of this study was to evaluate the serial morphological changes of the SB ostium after PCB treatment of de novo coronary lesions of main vessels by assessing the SB ostium with optical coherence tomography (OCT) before and immediately after treatment, and at 9-months follow-up.
This prospective, observational single-center study enrolled patients between June 2012 and June 2013 from Ulsan University Hospital. The diagnostic coronary angiography was performed for suspicious cases of myocardial ischemia, based on the clinical presentation and positive findings from non-invasive tests. Patients with stable or unstable angina pectoris scheduled for percutaneous coronary intervention (PCI) but unable to receive long-term dual antiplatelet therapy (DAPT) due to high bleeding risk, poor compliance or awaiting non-cardiac surgery and therefore planned for PCB treatment for their de novo lesions, were eligible for enrollment. Lesions with ≥70% diameter stenosis by visual estimate, a reference vessel diameter of between 2.5 mm and 3.5 mm and lesion length of ≤24 mm which had a SB diameter of ≥1.5 mm regardless of SB stenosis were included in the study.7 Exclusion criteria was left ventricular ejection fraction <30%, acute myocardial infarction (MI), left main disease, ostial lesions that were impossible to assess with OCT, heavily calcified or thrombotic lesions, life expectancy <1 year and known chronic kidney disease (creatinine >2 mg/dL). This study was carried out according to the Declaration of Helsinki guidelines and was approved by the Institutional Review Board Ethics Committee at Ulsan University Hospital. All enrolled patients provided written informed consent.
All patients were treated with acetylsalicylic acid 200 mg and a loading dose of clopidogrel 300 mg to 600 mg before the procedure, followed by maintenance clopidogrel 75 mg daily for 6 weeks. Heparin (100 U/kg) was initially administered intravenously and an activated clotting time ≥250 seconds was maintained during the procedure. All lesions in the main vessel underwent plain old balloon angioplasty pre-dilation with an optimal sized balloon based on angiography with a 1:1 balloon-to-vessel ratio with inflation at nominal pressure and was shorter than the intended length of the PCB. The PCB (SeQuent Please®, PCB catheter, B. Braun, Melsungen, Germany) diameter was sized at 1:1 balloon-to-vessel ratio and inflated at nominal pressure for 60 seconds. Additional bailout stenting was allowed in cases of severe dissection with Thrombolysis In Myocardial Infarction (TIMI) angiographic flow of 0 or 1, or a residual stenosis >30% after balloon angioplasty and PCB treatment.4
Coronary angiograms before and after PCB application and at 9-months follow-up were analyzed using the Cardiovascular Angiography Analysis System (CAAS 5.10, Pie Medical Imaging B.V., Maastricht, the Netherlands) by an independent investigator, who was blinded to the clinical presentation. The main vessel and the SB were analyzed separately.
OCT of the main vessel was performed before and after balloon angioplasty and at 9-months follow-up. OCT of the SB was performed in only one case, as shown in Fig. 1. Images were acquired using the commercially available frequency-domain OCT system and optic catheter (C7XR™ and Dragon Fly™ catheter, LightLab Imaging/St. Jude Medical, Westford, MA, USA). Using the non-occlusive technique, a 2.7 Fr OCT catheter was advanced distal to the lesion along a conventional 0.014-inch guidewire, and images were obtained by motorized pull-back at a rate of 20 mm/s during continuous flushing of 20 mLs of contrast media. Quantitative OCT analysis was performed by proprietary software after calibration for z-offset with the analysis of the images, done by another independent investigator (J. N. N).
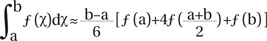
Each OCT cross-sectional still frame was selected with a 0.2 mm interval at the segments crossing a SB. The lumen area of the SB ostium was measured using the Simpson's rule, a numerical method that approximates the value of a definite integral by using quadratic polynomials: as shown above and in Fig. 2.8
For the change in the main vessel around the SB, analyses of the proximal and distal rims of the SB ostium in main vessel were defined as follows and in Fig. 2:
· Proximal rim of the SB ostium in main vessel: first frame proximally to the take-off of the SB
· Distal rim of the SB ostium in main vessel: first frame distally to the take-off of the SB
The percentage change was calculated using the following method; % change=[(the difference between the two numbers compared)/original number]×100.
All statistical analyses were done using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mea±SD or median (25th to 75th interquartile range). Continuous variables were compared between 2 groups using the paired Student's t test for data with normal distribution or Wilcoxon signed rank test for data with non-normal distribution. A 2-tailed p value of 0.05 was considered statistically significant.
Sixteen lesions of main vessels from sixteen patients were successfully treated with PCB and included in the analysis. Among them, 32 SBs were observed. 6 SBs were excluded due to poor OCT images (5 because of wire artifact and 1 dissection flap). Therefore, the final study analysis consisted of 26 SBs (Fig. 3). Baseline clinical and procedural characteristics are described in Table 1.
The quantitative coronary angiography data are showed in Table 2. The main vessel minimal lumen diameter increased at 9-months follow-up (1.22±0.50 mm pre-procedure, 2.19±0.29 mm post-procedure and 2.20±0.32 mm at 9-months). Late luminal loss of main vessel was -0.01±0.18 mm, and luminal net gain of the main vessel was 0.99±0.57 mm at 9-months. The main vessel diameter stenosis decreased at 9-months follow-up (55.6±15.4% at pre-procedure, 24.8±7.8% at post-procedure and 22.2±10.4% at 9-months). The minimal lumen diameter of SB increased at 9-months follow-up (0.97±0.44 mm at pre-procedure, 1.02±0.33 mm at post-procedure and 1.04±0.38 mm at 9-months). Late luminal loss of SB ostium was -0.02±0.22 mm at 9-months. No additional bailout stenting, SB occlusion or slow flow (TIMI <3) occurred after PCB treatment. There were no serious adverse events during the 9-months follow-up period.
The OCT findings are presented in Table 3 and Fig. 4. The lumen area of the proximal rim of the SB ostium in main vessel increased at 9-months follow-up (3.74±2.64 mm2 pre-procedure, 5.03±1.95 mm2 post-procedure and 6.14±2.21 mm2 at 9-months). The lumen area of distal rim of the SB ostium in main vessel also increased at 9-months follow-up (4.35±2.11 mm2 pre-procedure, 4.71±1.92 mm2 post-procedure and 5.88±2.10 mm2 at 9-months). The SB ostial lumen area increased at 9-months follow-up (0.92±0.68 mm2 pre-procedure, 1.03±0.77 mm2 post-procedure and 1.42±1.18 mm2 at 9-months). The mean SB ostial lumen area gain was 0.02±0.24 mm2 between pre- and post-procedure, 0.37±0.64 mm2 between post-procedure and 9-months and 0.60±0.93 mm2 between pre-procedure and 9-months. The median SB ostial lumen area percentage change was 3.9% [interquartile range (IQR) of -33.3 to 10.4%] between pre- and post-procedure, 52.1% (IQR of -0.7 to 77.3%) between post-procedure and 9-months and 76.1% (IQR 18.2 to 86.6%) between pre-procedure and 9-months.
This prospective, observational study shows that PCB treatment of de novo coronary lesions of main vessels increased the SB ostial lumen area at 9-months follow-up for the majority of the included SBs (20 of 26).
Since the beginning of the PCI era, interventions on lesions involving the SB have been recognized as a potential source of acute complications.9 Previous studies have shown SB occlusion after PCI of the main vessel as the most common cause of peri-procedural MI and associated with an increased risk of mortality.1011 Consequently, complex strategies have been used to treat coronary bifurcation lesions in order to protect the SB, however, these procedures can lead to additional thrombus formation and a higher incidence of MI, especially in the setting of acute coronary syndrome.1213 Although the advent of coronary stenting has reduced the risks for dissection and acute vessel closure, in-stent restenosis is still noted to be frequent at the SB ostium.14 Additionally, in bifurcation lesions where a single-stent crossover strategy is used in the main vessel, approximately 20–25% of bifurcation lesions still have hemodynamic compromise in the SB, despite a SB ostial stenosis <75% before the procedure.1516
PCB may be advantageous over DES by providing an immediate and homogeneous drug uptake by the vessel wall, avoiding inflammatory reaction to stent struts or polymers, and respecting the original anatomy of the bifurcation.17 Our data shows that PCB treatment of de novo lesions of main vessels did not compromise the SB ostium but increased the SB ostial lumen area at 9-months follow-up (Fig. 1). The ostial lumen area increased 52.1% (IQR of -0.7 to 77.3%) between post-procedure and 9-months and 76.1% (IQR 18.2 to 86.6%) between pre-procedure and 9-months. Interestingly, our results also show that PCB treatment of main vessels increased the main vessel lumen at 9-months follow-up (main vessel mean lumen area, 4.77±1.45 vs. 5.69±1.71 mm2, p=0.008). Late luminal loss of the main vessel was -0.01±0.18 mm and luminal net gain of the main vessel was 0.99±0.57 mm at 9-months. It is understood that the lumen area increase in the proximal and distal rims of the SB ostium in the main vessel, as well as the SB ostium may be through the same mechanism.
Although the exact mechanism by which PCB contributes to the SB ostial lumen area increase around the main vessel lesion is not well understood, it is more likely the result of positive vessel remodeling due to the local drug delivery effects from PCB treatment.18 The sustained pharmacological effects of paclitaxel are exerted from the binding to the subunit of tubulin, resulting in the arrest of microtubule function, up-regulation of pro-apoptotic factors and promotion of prolonged antiproliferation.1920 Studies have shown that even a short contact between taxane compounds and vascular smooth muscle cells can inhibit the proliferation of the cells for a long period.21,22 Paclitaxel has been found in a much higher concentration in the vascular wall after PCB treatment than that after DES implantation.23 Therefore, it is possible that the more profound effects not only on neointimal growth but also on medial thinning and enlargement are the results of paclitaxel.18
Recent trials of PCB treatment of bifurcation lesions did not unfortunately produce substantial positive results. A previous randomized bifurcation study comparing PCB treatment to bare metal stent (BMS) and DES showed no superiority of the PCB over BMS in terms of late lumen loss or clinical outcomes.24 Late lumen loss in the SB was 0.19±0.66 mm in the group which received pretreatment of both main vessels, and SB with PCB; 0.21±0.57 mm in the group receiving conventional BMS in the main vessel and 0.11±0.43 mm in the group receiving paclitaxel DES in the main vessel.24 A small, observational study investigating the efficacy and safety of PCB revealed a very low in-lesion late luminal loss; however, late and very late stent thrombosis occurred in two patients treated with BMS after PCB application in the main vessel.25 Nonetheless, it is noteworthy to mention that the previous trials used a PCB with stent approach rather than a PCB only approach. The most important difference in our study as compared to previous studies of bifurcation lesions is that the PCB treatment was used without a metal stent in the main vessel, accompanies with no treatment to the SB. Previous studies have suggested that carina shift is the major mechanism of SB ostial compromise and is significantly correlated to the distal main vessel lumen volume increase due to stent expansion.326 In other words, the change of vessel geometry after stent implantation leads to increased major adverse cardiac events. In our study, PCB maintained the original anatomy of the carina without any stent scaffolds, hence diminishing any of abnormal flow patterns into the SB.
Finally, to our fest knowledge, our present study is the first to demonstrate that a PCB only approach may be an option to avoid compromise of the SB ostium following PCI of bifurcation lesions using stents. This relative simple procedure was safe and produced excellent follow-up results on serial angiography and OCT imaging. Moreover, PCB treatment provides patients, who are unable to tolerate long-term DAPT, a safe alternative to coronary stent implantation.
There are some limitations to our study that need consideration. First, this study was an observational study with of small patients and lesions. Nevertheless, sensitive techniques were used, which allowed for the assessment of the short and medium-term mechanisms involved at the SB ostium after PCB treatment of main vessel lesions. Secondly, patients had relatively small sized SBs. Although further studies are required to evaluate the findings in larger SB ostium following PCB treatment, we expect to be able to apply our findings to larger SBs because of the consistent underlying mechanisms that occur. Therefore, despite from small SBs, the results are worthy of notice. Finally, OCT of the SB was performed in only one case in this study. In the future, OCT evaluations of both the main vessel and the SB are required to confirm our findings.
In conclusion, PCB treatment of de novo coronary lesions of main vessels resulted in an increase in the SB ostial lumen area at 9-months. Therefore, a PCB treatment approach to main vessels with SBs may be an option to avoid compromise of the SB ostium, when compared to PCI with stents.
Figures and Tables
Fig. 1
Pre-procedure (A), post-procedure (B) and follow-up angiographic images (C) coupled to corresponding OCT images. OCT images were captured in corresponding segments through main vessel (D and G) and SB (E, F, H, and I) (i.e., same OCT segment is depicted between post-procedure, and follow-up) by means of a software synchronization tool. Pre-procedure angiographic image shows a true bifurcation lesion. After the procedure, the OCT image demonstrates dissection of main vessel, and SB ostium shows compromise from the dissected flap of the main vessel (D). At follow-up, the lumen area of the main vessel (G and H) and SB ostium (H and I) increases further due to the drug effect. The dissections as seen on OCT at the SB ostium have healed (G). The arrows and asterisks represent SB ostium. OCT, optical coherence tomography; SB, side-branch.

Fig. 2
Method of analysis of the SB ostium. Simpson's rule is an approximation method for calculating the area of an irregular shape. In (A), the approximate area is found by the formula: A=h/3 (df+4 dm+dl), where h=distance between successive measurements, df=first measurement, dm=middle measurement, dl=last measurement. In (B), the Simpson's rule can be derived by approximating the integrand f (x) by the quadratic interpolant P (x). We measured cross-sectional length of SB ostium with a 0.2 mm interval on still frame of OCT images (C) and calculated the lumen area of SB ostium using application of Simpson's rule (a=initial point of measurement at the intersection, b=end point of measurement at the intersection). SB, side-branch; OCT, optical coherence tomography.

Fig. 3
Study diagram of the present study. OCT, optical coherence tomography; PCB, paclitaxel-coated balloon; SB, side-branch.

Fig. 4
The changes in the main vessel lumen area (A) and the SB ostial lumen area (B) pre-procedure, post-procedure and at 9-months follow-up. SB, side-branch.

Table 1
Baseline Clinical and Procedural Characteristics

LV, left ventricular; CAD, coronary artery disease; LAD, left anterior descending artery; DG br, diagonal branch; LCX, left circumflex artery; OM br, obtuse marginal branch; RCA, right coronary artery; SB, side-branch; POBA, plain old balloon angioplasty; PCB, paclitaxel-coated balloon.
Data is presented as mean±SD or number (percentage).
Table 2
Quantitative Coronary Angiography Measurements

Table 3
OCT Analysis at Main Vessel and SB Ostium

References
1. Steigen TK, Maeng M, Wiseth R, Erglis A, Kumsars I, Narbute I, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006; 114:1955–1961.

2. Koo BK, Kang HJ, Youn TJ, Chae IH, Choi DJ, Kim HS, et al. Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005; 46:633–637.

3. Gil RJ, Vassilev D, Formuszewicz R, Rusicka-Piekarz T, Doganov A. The carina angle-new geometrical parameter associated with periprocedural side branch compromise and the long-term results in coronary bifurcation lesions with main vessel stenting only. J Interv Cardiol. 2009; 22:E1–E10.

4. Kleber FX, Rittger H, Bonaventura K, Zeymer U, Wöhrle J, Jeger R, et al. Drug-coated balloons for treatment of coronary artery disease: updated recommendations from a consensus group. Clin Res Cardiol. 2013; 102:785–797.

5. Dou K, Zhang D, Xu B, Yang Y, Yin D, Qiao S, et al. An angiographic tool for risk prediction of side branch occlusion in coronary bifurcation intervention: the RESOLVE score system (Risk prEdiction of Side branch OccLusion in coronary bifurcation interVEntion). JACC Cardiovasc Interv. 2015; 8(1 Pt A):39–46.

6. Scheller B, Speck U, Abramjuk C, Bernhardt U, Böhm M, Nickenig G. Paclitaxel balloon coating, a novel method for prevention and therapy of restenosis. Circulation. 2004; 110:810–814.

7. Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005; 1:219–227.
8. Atkinson KE. An introduction to numerical analysis. New York: Wiley & Sons;1989. p. 111–120.
9. Aliabadi D, Tilli FV, Bowers TR, Benzuly KH, Safian RD, Goldstein JA, et al. Incidence and angiographic predictors of side branch occlusion following high-pressure intracoronary stenting. Am J Cardiol. 1997; 80:994–997.

10. Park DW, Kim YH, Yun SC, Ahn JM, Lee JY, Kim WJ, et al. Frequency, causes, predictors, and clinical significance of peri-procedural myocardial infarction following percutaneous coronary intervention. Eur Heart J. 2013; 34:1662–1669.

11. Hahn JY, Chun WJ, Kim JH, Song YB, Oh JH, Koo BK, et al. Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting). J Am Coll Cardiol. 2013; 62:1654–1659.
12. Pan M, de Lezo JS, Medina A, Romero M, Segura J, Pavlovic D, et al. Rapamycin-eluting stents for the treatment of bifurcated coronary lesions: a randomized comparison of a simple versus complex strategy. Am Heart J. 2004; 148:857–864.

13. Hildick-Smith D, de Belder AJ, Cooter N, Curzen NP, Clayton TC, Oldroyd KG, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation. 2010; 121:1235–1243.

14. Sheiban I, Albiero R, Marsico F, Dharmadhikari A, Tzifos V, Pagnotta P, et al. Immediate and long-term results of "T" stenting for bifurcation coronary lesions. Am J Cardiol. 2000; 85:1141–1144.

15. Koo BK, Park KW, Kang HJ, Cho YS, Chung WY, Youn TJ, et al. Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008; 29:726–732.

16. Koo BK, Waseda K, Kang HJ, Kim HS, Nam CW, Hur SH, et al. Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010; 3:113–119.

17. Herdeg C, Oberhoff M, Baumbach A, Blattner A, Axel DI, Schröder S, et al. Local paclitaxel delivery for the prevention of restenosis: biological effects and efficacy in vivo. J Am Coll Cardiol. 2000; 35:1969–1976.

18. Kleber FX, Schulz A, Waliszewski M, Hauschild T, Böhm M, Dietz U, et al. Local paclitaxel induces late lumen enlargement in coronary arteries after balloon angioplasty. Clin Res Cardiol. 2015; 104:217–225.

19. Pires NM, Eefting D, de Vries MR, Quax PH, Jukema JW. Sirolimus and paclitaxel provoke different vascular pathological responses after local delivery in a murine model for restenosis on underlying atherosclerotic arteries. Heart. 2007; 93:922–927.

20. Gray WA, Granada JF. Drug-coated balloons for the prevention of vascular restenosis. Circulation. 2010; 121:2672–2680.

21. Axel DI, Kunert W, Göggelmann C, Oberhoff M, Herdeg C, Küttner A, et al. Paclitaxel inhibits arterial smooth muscle cell proliferation and migration in vitro and in vivo using local drug delivery. Circulation. 1997; 96:636–645.

22. Scheller B, Speck U, Schmitt A, Böhm M, Nickenig G. Addition of paclitaxel to contrast media prevents restenosis after coronary stent implantation. J Am Coll Cardiol. 2003; 42:1415–1420.

23. Speck U, Cremers B, Kelsch B, Biedermann M, Clever YP, Schaffner S, et al. Do pharmacokinetics explain persistent restenosis inhibition by a single dose of paclitaxel? Circ Cardiovasc Interv. 2012; 5:392–400.

24. Stella PR, Belkacemi A, Dubois C, Nathoe H, Dens J, Naber C, et al. A multicenter randomized comparison of drug-eluting balloon plus bare-metal stent versus bare-metal stent versus drug-eluting stent in bifurcation lesions treated with a single-stenting technique: six-month angiographic and 12-month clinical results of the drug-eluting balloon in bifurcations trial. Catheter Cardiovasc Interv. 2012; 80:1138–1146.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download