Abstract
Purpose
To compare prostate cancer detection rates between 12 cores transrectal ultrasound-guided prostate biopsy (TRUS-Bx) and visually estimated multiparametric magnetic resonance imaging (mp-MRI)-targeted prostate biopsy (MRI-visual-Bx) for patients with prostate specific antigen (PSA) level less than 10 ng/mL.
Materials and Methods
In total, 76 patients with PSA levels below 10 ng/mL underwent 3.0 Tesla mp-MRI and TRUS-Bx prospectively in 2014. In patients with abnormal lesions on mp-MRI, we performed additional MRI-visual-Bx. We compared pathologic results, including the rate of clinically significant prostate cancer cores (cancer length greater than 5 mm and/or any Gleason grade greater than 3 in the biopsy core).
Results
The mean PSA was 6.43 ng/mL. In total, 48 of 76 (63.2%) patients had abnormal lesions on mp-MRI, and 116 targeted biopsy cores, an average of 2.42 per patient, were taken. The overall detection rates of prostate cancer using TRUS-Bx and MRI-visual-Bx were 26/76 (34.2%) and 23/48 (47.9%), respectively. In comparing the pathologic results of TRUS-Bx and MRI-visual-Bx cores, the positive rates were 8.4% (77 of 912 cores) and 46.6% (54 of 116 cores), respectively (p<0.001). Mean cancer core lengths and mean cancer core percentages were 3.2 mm and 24.5%, respectively, in TRUS-Bx and 6.3 mm and 45.4% in MRI-visual-Bx (p<0.001). In addition, Gleason score ≥7 was noted more frequently using MRI-visual-Bx (p=0.028). The detection rate of clinically significant prostate cancer was 27/77 (35.1%) and 40/54 (74.1%) for TRUS-Bx and MRI-visual-Bx, respectively (p<0.001).
For prostate cancer diagnosis, many physicians rely on transrectal ultrasound-guided prostate biopsy (TRUS-Bx). The protocol of TRUS-Bx has recently changed to 12 cores from a previous sextant biopsy protocol, because many studies indicated that an increased number of biopsy cores could increase the detection of prostate cancer.1 However, the detection rate of prostate cancer was not improved in patients with elevated prostate specific antigen (PSA) levels even with the increase in biopsies obtained more than 12-cores.23 In addition, the false negative results of prostate biopsy in those patients with PSA levels below 10 ng/mL allow for possible disease progression and prevent possible curative therapy.45 For example, when the prostate cancer is located in the anterior region of prostate, it is not easy to find out, leading to false negative results.6 Furthermore, because this scheme is based on the randomized biopsy of prostate using the visual guidance of TRUS, the 12-core TRUS-Bx can potentially misclassify as active surveillance (AS) candidates in prostate cancer patients who need definite therapy.789 This results in the undersampling of significant prostate cancer. To reduce these limitations, many investigators have employed multiparametric magnetic resonance imaging (mp-MRI) for prostate biopsy.
Recent studies have shown that additional targeted prostate biopsies of suspicious lesions seen by mp-MRI enable more complete and precise sampling.101112131415 It has been proposed that mp-MRI-targeted prostate biopsy (mp-MRI-Bx) decreases the detection of insignificant prostate cancer while increasing detection of significant tumors.1617 Recently, many investigators use one of two types of mp-MRI-Bx: MRI-visual-Bx or MRI/TRUS-fusion-Bx.1819 With regard to overall prostate cancer detection, several studies have suggested that these two mp-MRI-Bx techniques show similar performance.16171819 According to recent studies,1819 overall prostate cancer detection rate of MRI/TRUS-fusion-Bx was 36.0–53.0% and that of MRI-visual-Bx was 32.0–47.0%. They reported that these rates were not statistically different. However, MRI/TRUS-fusion-Bx need a specific software and devices for targeting a suspicious lesion on mp-MRI. We thought that MRI-visual-Bx is a realistic alternative under the real practice in detecting clinically significant prostate cancer in patients with low PSA levels.
In this study, we investigated the ability of MRI-visual-Bx at a single center to detect clinically significant prostate cancer among patients with PSA levels less than 10 ng/mL.
This prospective single center study was done at Pusan National University Yangsan Hospital, Yangsan, Korea. Institutional Review Board (IRB) approval was granted and informed consent was obtained from patients before study inclusion. We performed in accordance with the Declaration of Helsinki (IRB number: 05-2013-007). We reviewed the records of 76 patients who underwent targeted prostate biopsy in 2014. All patients were prospectively enrolled from January to December 2014. The study inclusion criteria were: 1) PSA level lower than 10 ng/mL; 2) normal digital rectal exam; and 3) no previous prostate biopsy history. We decided these inclusion criteria to show the performance of mp-MRI-Bx in comparison with TRUS-Bx in potentially low risk prostate cancer patients who had low PSA level under 10 ng/mL without extraprostatic disease. Before prostate biopsy decision making, we explained the risks and benefits of mp-MRI-Bx to the patients. We performed mp-MRI, including T2-weighted imaging and diffusion-weighted imaging (DWI), in those patients who agreed to proceed with mp-MRI-Bx.
Initially, all patients underwent 3.0 Tesla (T) DW-MRI (Intera-Achieva 3.0 T, Phillips Medical System, Best, the Netherlands), equipped with a phased-array coil (six-channel). Two b-values (0–1000) were used and diffusion restriction was quantified through apparent diffusion coefficient (ADC) mapping. We did not add dynamic contrast imaging to our MRI protocol, because it generates additional cost and time, and we also believed that there was little benefit for prostate biopsy of patients with PSA levels below 10 ng/mL. The DWI data and ADC map were interpreted by 2 experienced uroradiologists. The uroradiologists denoted suspicious regions of interest (ROIs) on ADC maps on a Digital Imaging and Communications in Medicine (DICOM) workstation. We used a 3 grade scoring system based on visual analysis of high b-value images and ADC maps to assign suspicious lesions. In case of indistinct hypointense area in ADC map, they described these ROIs as a low suspicious lesion. ROIs of focal mildly/moderately hypointense on ADC and isointense/mildly hyperintense on high b-value DWI were indicated as a moderately suspicious lesion. And, ROIs of focal markedly hypointense on ADC and markedly hyperintense on high b-value DWI were indicated as a highly suspicious lesion, respectively.
A urologist (D.H.L) with over 10 years of experience in TRUS-Bx performed all the prostate biopsies in the study. All patients were prepared with local gel anesthetics using a BK ultrasound scanner, endfire transducer, a needle guide, and an 18-G 25-cm biopsy needle. The operator first reviewed the DWI data and ADC map. Any suspicious lesions on the ADC map were visually matched and registered on the corresponding axial TRUS image based on zonal anatomy and tissue landmarks such as the ejaculation duct, apex or seminal vesicle. If a suspicious lesion on the ADC map was clearly matched with TRUS imaging, the operator sampled one targeted biopsy core without additional specimens. If a suspicious lesion on the ADC map was not clearly matched with TRUS imaging, the operator performed prostate biopsy in the matched TRUS area using zonal anatomy and also sampled an additional core from the same prostatic area, if possible, using an adjacent area as a guide by visual estimation. In this situation, the biopsy cores were kept in the same tissue bottle. All other MRI-visual-Bx cores were marked and kept in separate bottles according to the location of the suspicious lesion on DWI. After MRI-visual-Bx, TRUS-Bx cores were taken from 12 prostatic regions and marked separately. Patients without suspicious lesions on mp-MRI underwent 12-core TRUS-Bx only.
A genitourinary pathologist reviewed and described all biopsy cores. For each positive biopsy core for prostate cancer, Gleason score, the total core length, and the cancer core length were reported. Also, atypical small acinar proliferation (ASAP), high-grade prostate intraepithelial neoplasia (HGPIN), and any sign of inflammation were reported if present. To evaluate the clinical significance of prostate cancer, we defined a clinically significant prostate cancer core as having a cancer length greater than 5 mm and/or a Gleason grade greater than 3.20
We compared the pathologic results of biopsy cores from both biopsy procedures using chi-square tests and independent t-tests for categorical and continuous variables, respectively. In comparing MRI-visual-Bx and TRUS-Bx, we analyzed the positive core rate, mean cancer core length, mean cancer core percentage and the rate of clinically significant prostate cancer core. The results of targeted prostate biopsy were stratified according to the level of suspicion on DWI. Also, we re-classified and compared prostate cancer risk using the pathologic results of TRUS-Bx, and combined the results of both biopsy procedures. All statistical analyses were performed using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA). A p-value ≤0.05 was considered statistically significant.
The clinical characteristics of patients are shown in Table 1. Among a total of 76 patients, the mean age was 65.8 years and the mean PSA was 6.43 ng/mL. At the time of MRI-visual-Bx, mean prostate volume was 38.8 mL and PSA density was 0.190. A total of 116 targeted biopsy cores, an average of 2.42 per patient, were taken, and 48 of 76 (63.2%) patients had abnormal lesions on DWI. The detection rate of prostate cancer using TRUS-Bx and MRI-visual-Bx was 26/76 (34.2%) and 23/48 (47.9%), respectively. In combining both prostate biopsy procedures, the detection rate was 29/76 (38.2%), because an additional 3 patients were diagnosed with prostate cancer by MRI-visual-Bx. Among 47 patients with negative biopsies, 2 had ASAP and 1 had HGPIN on MRI-visual-Bx.
Table 2 shows the pathologic outcomes for each biopsy procedure. When we analyzed the pathologic results using each prostate biopsy core, the detection rate of prostate cancer was 77/912 (8.44%) in TRUS-Bx cores and 54/116 (46.6%) in MRI-visual-Bx cores (p<0.001). In addition, the mean cancer core length and mean cancer core percentage were statistically different; mean cancer core length in MRI-visual-Bx cores was significantly longer than TRUS-Bx cores (p<0.001). Also, there were significant differences in the distribution of biopsy Gleason scores (p=0.028). In MRI-visual-Bx cores, Gleason score ≥7 was diagnosed more frequently than in TRUS-Bx cores. Gleason score 8 was found only in biopsy cores of MRI-visual-Bx. Furthermore, the rate of clinically significantly cancer core was significant higher in MRI-visual-Bx (p<0.001).
The results of MRI-visual-Bx according to the level of suspicion in the DWI data are shown in Table 3. As the level of suspicion increased, the detection rate of prostate cancer improved, as did the number of clearly matched lesions on TRUS. In those patients with lesions of low suspicion, there were fewer clear TRUS lesions that could be used as a target for MRI-visual-Bx. As such, the detection rate was lower than in other patients. However, if clear TRUS lesions were present, and we could perform a target for MRI-visual-Bx, even on a less suspicious lesion, the detection rate was not significantly different.
Among 26 prostate cancer patients detected by TRUS-Bx, 19 were classified as low risk and 7 patients were at intermediate risk prostate cancer. No patients were at high risk of prostate cancer. Additionally, 8 patients could be considered AS candidates by the Prostate Cancer Research International: Active Surveillance (PRIAS) protocol.21 Inclusion criteria of PRIAS protocol were 1) organ-confined Gleason score 6 disease; 2) PSA level ≤10 ng/mL; 3) PSA density ≤0.2; and 4) less than 2 positive biopsy cores. However, using the combined pathologic results of MRI-visual-Bx and TRUS-Bx, an additional 3 patients were newly diagnosed as prostate cancer patients and only 3 could be classified as AS candidates. Furthermore, 2 low risk prostate cancer patients and 2 intermediate prostate cancer patients, as determined by TRUS-Bx, were re-classified as having high risk prostate cancer (Table 4).
According to recent studies, mp-MRI-Bx and TRUS-Bx showed a similar overall detection rate of prostate cancer in men with an initial biopsy.1617 However, for patients who had a previous negative biopsy, mp-MRI-Bx showed an improved detection rate in comparison with TRUS-Bx.1617 For these reasons, many urologists have questioned whether mp-MRI-Bx should be performed for patients without a previous prostate biopsy history because of associated extra cost and effort. However, its improved detection rate of clinically significant prostate cancer in comparison to TRUS-Bx makes mp-MRI-Bx an attractive technique for both physicians and patients.16171819
Meta-analysis about mp-MRI-Bx1617 indicates that detection of clinically significant prostate cancer was higher for mp-MRI-Bx than TRUS-Bx with a relative sensitivity of 1.20 [95% confidence interval (CI) 1.09–1.32]. Additionally, detection of insignificant prostate cancer was lower for mp-MRI-Bx than TRUS-Bx with relative sensitivity of 0.56 (95% CI 0.37–0.85). Comparing with conventional TRUS-Bx, therefore, we could perform prostate biopsy with an additional intraprostatic information of DW-MRI as well as the abnormal lesion of TRUS. In other words, we could target suspicious TRUS lesion in concordance with MP-MRI finding and obtain prostate tissue more precisely. Therefore, MRI-visual-Bx might show better diagnostic performance in identifying clinically significant prostate cancer than conventional TRUS-Bx.
This advantage of mp-MRI-Bx was also shown in comparison with the transperineal template prostate biopsy (TP-Bx). In several centers, they performed TP-Bx for the first round biopsy, repeat biopsy and also confirmatory biopsy to detect clinically significant prostate cancer after TRUS-Bx.92223 According to Ong, et al.,22 the detection rate of clinically significant prostate cancer were 81–87% in the first round and repeat biopsies. Also, 23% of patients were diagnosed as higher grade cancer in TP-Bx than that of initial TRUS-Bx.923 They reported that the biopsy-related complications were not increased in comparison with the TRUS-Bx during the TP-Bx.24 According to these above results, TP-Bx would be the alternative option of TRUS-Bx and even mp-MRI-Bx. According to the head to head comparison between TP-Bx and mp-MRI-Bx in prospective setting, however, mp-MRI-Bx showed significantly higher performance to detect clinically significant prostate cancer.2526 Considering the recent issues regarding the misclassification of AS candidates in very low risk prostate cancer patients, the above findings are invaluable in helping tailor decision-making to avoid the possibility of underestimating pathologic results from TRUS-Bx. We thought that the value of TP-Bx in comparison with mp-MRI-Bx should be needed for reevaluation, of several aspects, including MRI cost, with more prospective trials.
Generally, mp-MRI-Bx can be classified into two types of approach: MRI-visual-Bx and MRI/TRUS-fusion-Bx. In MRI-visual-Bx, operators estimate the targeted location in the prostate using real-time TRUS in concordance with the information of mp-MRI. Several investigators2728 demonstrated that this technique has better accuracy over TRUS-Bx. However, this technique relies on an experienced operator, and thus suffering from operator handling error. This error is especially prominent when targeting smaller lesions on mp-MRI. To overcome this limitation, many investigators have recently performed MRI/TRUS-fusion-Bx.293031 This technique uses unique computer software to superimpose images from mp-MRI and real-time TRUS. A novel device then can take a targeted biopsy based on this newly generated superimposed image. Even though, effective, MRI/TRUS-fusion-Bx is more expensive than MRI-visual-Bx due to its requirements of a specific device and computer software. Also, there are few prospective studies that demonstrated MRI/TRUS-fusion-Bx to be superior to MRI-visual-Bx.
There have been only two reports on the comparison of MRI-visual-Bx and MRI/TRUS-fusion-Bx.1819 In one study, MRI-visual-Bx did not show inferior detection of overall or significant prostate cancer as measured against MRI/TRUS-fusion-Bx. Puech, et al.19 compared MRI/TRUS-fusion-Bx to MRI-visual-Bx in 95 men using a 1.5 T MRI system. Although the mean PSA level of their cohort was 10.05 ng/mL (range: 1.3–52 ng/mL), they demonstrated no differences in cancer detection, cancer core length, or biopsy Gleason score in either technique. Additionally, Wysock, et al.18 demonstrated that, even though MRI/TRUS-fusion-Bx often provided more histological information than MRI-visual-Bx, it did not increase cancer detection rates. In their study, MRI/TRUS-fusion-Bx detected 20.3% of Gleason score ≥7, compared with 15.1% by MRI-visual-Bx, a statistically insignificant difference (p=0.0523). However, MRI-visual-Bx had a longer mean cancer core length than MRI/TRUS-fusion-Bx, even though they did not suggest statistical differences. Although only two studies have compared the two mp-MRI-Bx techniques, we thought that these results were sufficient evidence to indicate little difference between MRI/TRUS-fusion-Bx and MRI-visual-Bx. There are few studies thus far to support the improved detection rate of clinically significant prostate cancer in MRI-visual-Bx as compared to TRUS-Bx (Table 5). Almost all studies of MRI-visual-Bx focused on the accuracy and overall detection rate of prostate cancer compared with TRUS-Bx, and ignored the detection rate of clinically significant prostate cancer. Therefore, we thought that the results of MRI-visual-Bx would not be significantly different from those of MRI/TRUS-fusion-Bx and carried out our study with the simpler procedure.
In the present study, we compared MRI-visual-Bx and TRUS-Bx for prostate cancer detection among patients with a PSA level below 10 ng/mL. When we compared mean cancer core length, mean cancer core percentage, and biopsy Gleason score in the two biopsy procedures, mean cancer core length was longer and mean cancer core percentage was higher in MRI-visual-Bx. In addition, high Gleason scores were diagnosed more frequently in MRI-visual-Bx than TRUS-Bx. Furthermore, when we compared the pathologic results of each biopsy core by the two biopsy procedures, the cancer detection rate was significantly better in MRI-visual-Bx. Although we could not show superiority of overall cancer detection rate using the combined results of both biopsy procedures in comparison with TRUS-Bx alone, MRI-visual-Bx itself was able to diagnose more clinically significant cancer cores. These results were similar to other studies associated with mp-MRI-Bx.
In the present study, the overall prostate cancer detection rate was 34.2% in TRUS-Bx and 38.2% in the combined result of both biopsy procedures. Also, only three additional patients were diagnosed with prostate cancer by MRI-visual-Bx. Interestingly, our prostate cancer detection rate with TRUS-Bx was higher than other studies of Korean men who had PSA levels below 10 ng/mL. Seo, et al.32 reported that the prostate cancer detection rate of Korean men with PSA levels under 10 ng/mL was 19.6%. Similarly, according to Ahn, et al.,33 the detection rate of our institute during the last 13 years was 21.8%. Even with variation in the study cohorts, or the presence of selection or sampling bias, the gap in detection rate between the present study and current literatures is substantial.
It is quite likely that this difference was due to weakness of our study design. We performed MRI-visual-Bx and TRUS-Bx with the help of strictly one physician (D.H.L.). This means that random targeting in the prostate area for TRUS-Bx would be influenced by visually estimated mp-MRI targeted lesions if they were identified by the operator prior to biopsy. This could cause sampling bias for the increased detection rate of prostate cancer in TRUS-Bx. In other words, even if we performed the 12-core TRUS-Bx systematically by each divided area of the prostate, each core was more likely to target near previously identified mp-MRI-Bx lesions. To improve our study design, we would perform TRUS-Bx after MRI-visual-Bx using another physician under a blinded condition. This is the major limitation of our present study.
Other limitations exist in the present study, even though to a lesser extent. First, the study cohort used was smaller in comparison to other studies. However, the number of samples was limited a priori, since our study focused on patients with a PSA level under 10 ng/mL. Second, we could not evaluate the formal diagnostic accuracy of suspicious tumor lesions on mp-MRI because radical prostatectomy specimens were not available. Our institute does not possess the robotic surgery system used for radical prostatectomy, therefore, many patients who underwent mp-MRI-Bx were unfortunately sent to another tertiary hospital for robotic surgery. With matched prostate specimens, we could be able to report on the accuracy of visually estimated lesion targeting between mp-MRI and TRUS. In addition, we are planning a future study comparing diagnostic performance between MRI-visual-Bx, MRI/TRUS-fusion-Bx and TRUS-Bx for initial biopsy. The results will be helpful for choosing an initial biopsy technique for the diagnosis of clinically significant prostate cancer in patients who have PSA levels below 10 ng/mL.
In conclusion, our prospective study shows that MRI-visual-Bx is a superior technique to TRUS-Bx for detecting clinically significant prostate cancer, even in the initial biopsy of patients with PSA levels under 10 ng/mL. However, there was no statistical difference between two biopsy techniques in overall prostate cancer detection rate. We believe that large cohort studies should be conducted to more definitively characterize the benefit for patients with low PSA levels.
Figures and Tables
Table 1
Baseline Patient Characteristics (n=76)

Table 2
Pathologic Results of Two Prostate Biopsy Procedures

Table 3
Detection Rate of Prostate Cancer According to Concordance between a Matched Lesion on TRUS and a Suspicious Lesion on mp-MRI

Table 4
Prostate Cancer Risk Re-Classification Using the Pathologic Results of mp-MRI Targeted Biopsy
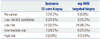
Table 5
The Published Clinicopathologic Data of Visually Estimated Magnetic Resonance Imaging Targeted Prostate Biopsy

| Investigators | No. of patients | Patients characteristics | MRI protocol | The detection rate of any caner (%) | The detection rate of clinically significant cancer (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Prior biopsy |
Age (SD or range) |
PSA (SD or range) |
PV (SD or range) |
Field strength | Sequence | TRUS-Bx | MR-visual-Bx | TRUS-Bx | MR-visual-Bx | ||
| Belas, et al.11 | 71 | Initial biopsy | 66 (47–76) | 7.0 (4.0–10.0) | 45 (15–150) | 1.5 T | T2WI, DCE, DWI | 46.4 | 70.2 | 83 | 96 |
| Delongchamps, et al.12 | 131 | Initial biopsy | 64.5±6.7 | 8.3±4.1 | 55.7±35.1 | 1.5 T | T2WI, DCE, DWI | 45.8 | 82.1 | NR | NR |
| Haffner, et al.13 | 555 | Initial biopsy | 64 (47–83) | 6.8 (0.18–100) | 46 (15–200) | 1.5 T | T2WI, DCE | 52.2 | 42.5 | 95 | 95 |
| Puech, et al.19 | 95 | Initial biopsy+previous negative biopsy | 65 (49–76) | 10.0 (1.3–52.0) | 52 (21–156) | 1.5 T | T2WI, DCE, DWI | 59 | 47 | 23.2 | NR |
| Wysock, et al.18 | 67 | Initial biopsy | 65 (56–71) | 5.1 (3.50–7.31) | 46 (31–63) | 3.0 T | T2WI, DCE, DWI | 55.2 | 34.3 | 41.8 | 75 |
| Present study | 76 | Initial biopsy | 66 (43–83) | 6.4 (3.30–9.80) | 39 (17–127) | 3.0 T | T2WI, DWI | 34.2 | 38.7 | 35.1 | 74.1 |
SD, standard deviation; PSA, prostate specific antigen; PV, prostate volume; T, tesla; MRI, magnetic resonance imaging; T2WI, T2-weighted image; DCE, dynamic contrast enhanced image; DWI, diffusion weighted image; TRUS-Bx, transrectal ultrasound-guided prostate biopsy; MR-visual-Bx, visually estimated magnetic resonance imaging targeted prostate biopsy; NR, not reported.
References
1. Elabbady AA, Khedr MM. Extended 12-core prostate biopsy increases both the detection of prostate cancer and the accuracy of Gleason score. Eur Urol. 2006; 49:49–53.

2. Eichler K, Hempel S, Wilby J, Myers L, Bachmann LM, Kleijnen J. Diagnostic value of systematic biopsy methods in the investigation of prostate cancer: a systematic review. J Urol. 2006; 175:1605–1612.

3. Pepe P, Aragona F. Saturation prostate needle biopsy and prostate cancer detection at initial and repeat evaluation. Urology. 2007; 70:1131–1135.

4. Heidenreich A, Abrahamsson PA, Artibani W, Catto J, Montorsi F, Van Poppel H, et al. Early detection of prostate cancer: European Association of Urology recommendation. Eur Urol. 2013; 64:347–354.

5. Ukimura O, Coleman JA, de la Taille A, Emberton M, Epstein JI, Freedland SJ, et al. Contemporary role of systematic prostate biopsies: indications, techniques, and implications for patient care. Eur Urol. 2013; 63:214–230.

6. Lawrentschuk N, Haider MA, Daljeet N, Evans A, Toi A, Finelli A, et al. 'Prostatic evasive anterior tumours': the role of magnetic resonance imaging. BJU Int. 2010; 105:1231–1236.

7. Dahabreh IJ, Chung M, Balk EM, Yu WW, Mathew P, Lau J, et al. Active surveillance in men with localized prostate cancer: a systematic review. Ann Intern Med. 2012; 156:582–590.

8. Lecornet E, Ahmed HU, Hu Y, Moore CM, Nevoux P, Barratt D, et al. The accuracy of different biopsy strategies for the detection of clinically important prostate cancer: a computer simulation. J Urol. 2012; 188:974–980.

9. Taira AV, Merrick GS, Bennett A, Andreini H, Taubenslag W, Galbreath RW, et al. Transperineal template-guided mapping biopsy as a staging procedure to select patients best suited for active surveillance. Am J Clin Oncol. 2013; 36:116–120.

10. Delongchamps NB, Lefèvre A, Bouazza N, Beuvon F, Legman P, Cornud F. Detection of significant prostate cancer with magnetic resonance targeted biopsies--should transrectal ultrasound-magnetic resonance imaging fusion guided biopsies alone be a standard of care? J Urol. 2015; 193:1198–1204.

11. Belas O, Klap J, Cornud F, Beuvon F, Peyromaure M, Zerbib M, et al. [Prebiopsy multiparametric MRI of the prostate: the end of randomized biopsies?]. Prog Urol. 2012; 22:583–589.
12. Delongchamps NB, Peyromaure M, Schull A, Beuvon F, Bouazza N, Flam T, et al. Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol. 2013; 189:493–499.

13. Haffner J, Lemaitre L, Puech P, Haber GP, Leroy X, Jones JS, et al. Role of magnetic resonance imaging before initial biopsy: comparison of magnetic resonance imaging-targeted and systematic biopsy for significant prostate cancer detection. BJU Int. 2011; 108(8 Pt 2):E171–E178.

14. Kuru TH, Roethke MC, Seidenader J, Simpfendörfer T, Boxler S, Alammar K, et al. Critical evaluation of magnetic resonance imaging targeted, transrectal ultrasound guided transperineal fusion biopsy for detection of prostate cancer. J Urol. 2013; 190:1380–1386.

15. Siddiqui MM, Rais-Bahrami S, Truong H, Stamatakis L, Vourganti S, Nix J, et al. Magnetic resonance imaging/ultrasound-fusion biopsy significantly upgrades prostate cancer versus systematic 12-core transrectal ultrasound biopsy. Eur Urol. 2013; 64:713–719.

16. Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MG. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol. 2015; 68:438–450.

17. Valerio M, Donaldson I, Emberton M, Ehdaie B, Hadaschik BA, Marks LS, et al. Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur Urol. 2015; 68:8–19.

18. Wysock JS, Rosenkrantz AB, Huang WC, Stifelman MD, Lepor H, Deng FM, et al. A prospective, blinded comparison of magnetic resonance (MR) imaging-ultrasound fusion and visual estimation in the performance of MR-targeted prostate biopsy: the PROFUS trial. Eur Urol. 2014; 66:343–351.

19. Puech P, Rouvière O, Renard-Penna R, Villers A, Devos P, Colombel M, et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy--prospective multicenter study. Radiology. 2013; 268:461–469.

20. Ploussard G, Epstein JI, Montironi R, Carroll PR, Wirth M, Grimm MO, et al. The contemporary concept of significant versus insignificant prostate cancer. Eur Urol. 2011; 60:291–303.

21. Lee DH, Jung HB, Lee SH, Rha KH, Choi YD, Hong SJ, et al. Comparison of pathological outcomes of active surveillance candidates who underwent radical prostatectomy using contemporary protocols at a high-volume Korean center. Jpn J Clin Oncol. 2012; 42:1079–1085.

22. Ong WL, Weerakoon M, Huang S, Paul E, Lawrentschuk N, Frydenberg M, et al. Transperineal biopsy prostate cancer detection in first biopsy and repeat biopsy after negative transrectal ultrasound-guided biopsy: the Victorian Transperineal Biopsy Collaboration experience. BJU Int. 2015; 116:568–576.

23. Onik G, Miessau M, Bostwick DG. Three-dimensional prostate mapping biopsy has a potentially significant impact on prostate cancer management. J Clin Oncol. 2009; 27:4321–4326.

24. Grummet JP, Weerakoon M, Huang S, Lawrentschuk N, Frydenberg M, Moon DA, et al. Sepsis and 'superbugs': should we favour the transperineal over the transrectal approach for prostate biopsy? BJU Int. 2014; 114:384–388.

25. Radtke JP, Kuru TH, Boxler S, Alt CD, Popeneciu IV, Huettenbrink C, et al. Comparative analysis of transperineal template saturation prostate biopsy versus magnetic resonance imaging targeted biopsy with magnetic resonance imaging-ultrasound fusion guidance. J Urol. 2015; 193:87–94.

26. Kasivisvanathan V, Dufour R, Moore CM, Ahmed HU, Abd-Alazeez M, Charman SC, et al. Transperineal magnetic resonance image targeted prostate biopsy versus transperineal template prostate biopsy in the detection of clinically significant prostate cancer. J Urol. 2013; 189:860–866.

27. Moore CM, Kasivisvanathan V, Eggener S, Emberton M, Fütterer JJ, Gill IS, et al. Standards of reporting for MRI-targeted biopsy studies (START) of the prostate: recommendations from an International Working Group. Eur Urol. 2013; 64:544–552.

28. Hambrock T, Somford DM, Hoeks C, Bouwense SA, Huisman H, Yakar D, et al. Magnetic resonance imaging guided prostate biopsy in men with repeat negative biopsies and increased prostate specific antigen. J Urol. 2010; 183:520–527.

29. Natarajan S, Marks LS, Margolis DJ, Huang J, Macairan ML, Lieu P, et al. Clinical application of a 3D ultrasound-guided prostate biopsy system. Urol Oncol. 2011; 29:334–342.

30. Fiard G, Hohn N, Descotes JL, Rambeaud JJ, Troccaz J, Long JA. Targeted MRI-guided prostate biopsies for the detection of prostate cancer: initial clinical experience with real-time 3-dimensional transrectal ultrasound guidance and magnetic resonance/transrectal ultrasound image fusion. Urology. 2013; 81:1372–1378.

31. Mozer P, Rouprêt M, Le Cossec C, Granger B, Comperat E, de Gorski A, et al. First round of targeted biopsies using magnetic resonance imaging/ultrasonography fusion compared with conventional transrectal ultrasonography-guided biopsies for the diagnosis of localised prostate cancer. BJU Int. 2015; 115:50–57.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download