Abstract
A 50-year-old peri-menopausal woman presented with hard palpable mass on her lower abdomen and anemia from heavy menstrual bleeding. Ultrasonography showed a 13×12 cm sized hypoechoic solid mass in pelvis and a 2.5×2 cm hypoechoic cystic mass in uterine endometrium. Abdomino-pelvic computed tomography revealed a hypodense pelvic mass without enhancement, suggesting a leiomyoma of intraligamentary type or sex cord tumor of right ovary with submucosal myoma of uterus. Laparoscopy revealed a large Sertoli-Leydig cell tumor of right ovary with a very rare entity of intra-endometrial uterine leiomyoma accompanied by adenomyosis. The final diagnosis of ovarian sex-cord tumor (Sertoli-Leydig cell), stage Ia with intra-endometrial leiomyoma with adenomyosis, was made. Considering the large size of the tumor and poorly differentiated nature, 6 cycles of chemotherapy with Taxol and Carboplatin regimen were administered. There is neither evidence of major complications nor recurrence during 20 months' follow-up.
A case of intra-endometrial uterine leiomyoma (IEUL) accompanied by large Sertoli-Leydig cell tumor (SLCT) of ovary is presented. An IEUL is rare and completely different from a relatively common submucosal type of leiomyoma.1 SLCT is also a rare sex cord stromal tumor of ovary, characterized by virilization and pelvic mass in most patients. Although virilization is the most common manifestation, it is unfortunately not in all cases, and secondary amenorrhea could be the only symptom in many cases.2 The majority of SLCT are benign, therefore, young patient at early stage could prefer fertility preserving conservative surgeries, those with risk factors should receive chemotherapy and long-term follow up.3456 The large SLCT in this case did not cause any hormonal imbalance, therefore, the tumor was diagnosed late. Herein, we describe a rare case of intra-endometrial leiomyoma presenting heavy menstrual bleeding accompanied by SLCT with poor prognostic factors.
A 50-year-old gravida 7 para 2 woman was referred with palpable pelvic mass and heavy menstrual bleeding. She had no virilization signs and no history of menstrual irregularity, which is often preceded by the virilization. Pelvic examination revealed a hard enlarged uterus and about fetal head sized mass. The ultrasonography revealed a solid hypoechoic mass of 13×12 cm size with cystic lesion and increased vascularity (Fig. 1A). The uterus enlarged to gestational 3 month size with mixed echogenicity, compatible to the findings of adenomyosis. Notably, about 2.5×2 cm hypoechoic solid mass with internal cystic lesion was noted in near endometirum (Fig. 1B). Left ovary was normal, however, right ovary was not found. Computed tomography revealed a hypodense pelvic mass without enhancement, suggesting a leiomyoma of intraligamentary type or sex cord tumor of right ovary (Fig. 1C). Enlarged uterus with isodense mass protruding into uterine cavity with internal cystic lesion was noted. Laboratory data, including testosterone, estrogen, thyroid stimulating hormone, and CA-125, were within normal limit, with the exception of decreased hemoglobin level (6.8 g/dL). A provisional diagnosis was ovarian fibroma or intraligamentary leiomyoma accompanied by uterine adenomyosis with degenerated submucosal myoma. Laparoscopy revealed a solid, yellow-tan colored, smooth-surface mass with intact capsule abundant of blood vessels (Fig. 2A). Frozen biopsy for the right ovarian mass revealed benign ovarian tumor, and laparoscopically assisted vaginal hysterectomy with right oophorectomy was performed.
The right ovarian mass was yellow colored solid tumor (Fig. 2B). Cut section of the uterus revealed white to gray tan-colored tumor-like lesion with cystic degeneration in submucosal layer (Fig. 2C and D). Histopathologically, several discrete nodular lesions composed of spindle-shaped smooth muscle cells were present within the endometrium (Fig. 3A and B). Ovarian tumor revealed predominantly spindle cell growth pattern characterized by minimal differentiation of Sertoli cells. Only focal area showed nests and thin cords resembling sex cords (Fig. 3C). Immunohistochemically, tumor cells were positive for α-inhibin, and some Leydig cells were highlighted by the calretinin stain (Fig. 3D and E).
Considering the high-risk factors (poor differentiation, large tumor size, and old age) of this patient, we decided to perform the second laparoscopy for complete staging of ovarian tumor. Abdominal cavity was explored systematically, however, there was no tumor deposit anywhere else in the cavity and peritoneal washing cytology was negative for malignant cells. Left salpingo-oophorectomy and cholecystectomy were performed simultaneously for multiple gallbladder stones.
The postoperative course was uneventful. The final pathologic diagnosis was poorly differentiated SLCT of ovary stage Ia and IEUL with adenomyosis. We had a detailed discussion about treatment options and decided to initiate chemotherapy considering the large size of tumor and poorly differentiated nature. Six cycles of chemotherapy with Taxol and Carboplatin regimen were administered 3 times a week. There is no evidence of recurrence during 20 months' follow-up.
IEUL is an extremely rare and is completely different from a submucosal leiomyoma connected to myometrium covered with submucosal layer. IEUL means multiple leiomyoma islands embedded in submucosal layer without connection with myometrium. These foci have sometimes been referred as smooth muscle metaplasia. A pleuripotential cell in uterus can differentiate into endometrial stroma and smooth muscle.7 Other differential diagnosis includes endometrial polyp, adenomyomatous polyp, and atypical polypoid adenomyoma. Adenomyomatous polyp is very similar to IEUL since adenomyomatous polyp has a mixture of myomatous stroma and glands. However, it can be excluded because there is no discrete nodular lesion formed by the smooth muscle cells in the endometrium. Atypical polypoid adenomyoma can also be excluded because it has irregular gland architecture in addition to a myomatous stroma.
SLCT is a rare sex cord stromal tumor of the ovary, characterized by virilization and pelvic mass. It is typically diagnosed in young women.2 However, in this case, it manifested late in her 50's. Poorly differentiaed cells in this case did not release testosterone or estrogen. It did not cause any hormonal disturbance, which is shown in about two thirds of SLCT cases. Normal serum hormonal status may delay the diagnosis until the tumor is growing to 13 cm, a relatively large size compared with the other reported SLCTs.28 The large tumors (over 10 cm), tumor rupture, and tumors of poor differentiation are known to be related with no endocrine changes and more aggressive behaviors.910 Most SLCT are benign, and few cases are low grade malignancy and stage I at the time of surgery. Well-differentiated SLCT are benign and there is no recurrence. However, 59% of poorly differentiated SLCT and 11% of those with intermediate differentiation are malignant.9 Total hysterectomy and bilateral salpingo-oophorectomy are recommended for women who finished childbearing. For early staged young women who want preserve fertility, conservative surgery of unilateral salpingo-oophorectomy could be an alternative treatment option. The necessity of pelvic lymphadenectomy is controversial.11 Postoperative chemotherapy has not demonstrated the benefit, and the optimal regimen still remain unclear. In this case, however, considering high-risk factors (poor differentiation, large tumor size, and old age) we counseled thoroughly with the patient and conducted 6 cycles of chemotherapy. In this case, we could learn the rare entity of IEUL which can present as a degenerated submucosal leiomyoma. Although the clinical symptom and prognosis of IEUL are not different from those of submucosal myoma, the histologic location of the tumor in submucosal layer is distinct from each other. The hormone which is known to be secreted from SLCT is not estrogen, but androgen. Therefore, the co-occurrence of IEUL is thought to be not related to the presence of SLCT. We should think of the possibility of SLCT whenever we encounter a hypoechoic solid pelvic mass in ultrasonography, and should perform a thorough physical examination, including virilization signs which are usually accompanied in most cases, although it was not manifested in this case.
Figures and Tables
Fig. 1
Preoperative ultrasonographic and computed tomography findings. (A) A 13×12 cm solid hypoechoic mass with multiple cystic lesions was noted on the right pelvic area accompanied by blood flow shadow. (B) About 2.5×2 cm hypoechoic solid mass (arrowheads) with internal cystic lesion was noted in the near endometrium. (C) A ring like hypodense mass in uterine cavity (arrow) and a large pelvic mass without enhancement, suggesting a leiomyoma of intraligamentary type or sex cord tumor of right ovary.

Fig. 2
Pelviscopic findings. (A) A 13×12 cm sized, yellow-tan colored ovarian tumor with multiple vessel engorgement. (B) Multiple fragments of yellow-tan colored ovarian tumor. (C) Cut section of the uterus shows white-gray tan tumor like-lesion with focal cystic degeneration centered in the submucosal layer of uterine corpus. (D) Enlarged photo of endometrial cystic mass (arrowheads).
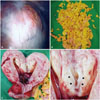
Fig. 3
Pathologic examination. (A) Scanning view of the endometrial tumor shows proliferative endometrioid-type glands varying in number and shape. Two discrete nodular lesions formed by smooth muscle are identified in the endometrium (arrowheads). (B) High-power view shows spindle-shaped smooth muscle cells arranged in fascicles (H&E, ×200). (C) Tumor shows diffuse sarcomatoid growth pattern focally associated with cord formation of Sertoli cells (arrowheads). Leydig cells are not conspicuous (H&E, ×100). (D) Tumor cells are immunoreactive for α-inhibin (×100). (E) Calretinin immunohistochemistry shows Leydig cells which are focally found in peripheral clusters (arrowheads) (×100). H&E, hematoxylin and eosin.

References
1. Crum CP, Nucci MR, Lee KR. Diagnostic Gynecologic and Obstetric Pathology. 2nd ed. Philadelphia: Saunders;2011.
2. Young RH, Scully RE. Ovarian Sertoli-Leydig cell tumors. A clinicopathological analysis of 207 cases. Am J Surg Pathol. 1985; 9:543–569.
3. Zhang M, Cheung MK, Shin JY, Kapp DS, Husain A, Teng NN, et al. Prognostic factors responsible for survival in sex cord stromal tumors of the ovary--an analysis of 376 women. Gynecol Oncol. 2007; 104:396–400.

4. Bhat RA, Lim YK, Chia YN, Yam KL. Sertoli-Leydig cell tumor of the ovary: analysis of a single institution database. J Obstet Gynaecol Res. 2013; 39:305–310.

5. Roth LM, Anderson MC, Govan AD, Langley FA, Gowing NF, Woodcock AS. Sertoli-Leydig cell tumors: a clinicopathologic study of 34 cases. Cancer. 1981; 48:187–197.

6. Kurman RJ, Ellenson HL, Ronnett BM. Blaustein's Pathology of the Female Genital Tract. 6th ed. New York: Springer;2011.
7. Gui T, Cao D, Shen K, Yang J, Zhang Y, Yu Q, et al. A clinicopathological analysis of 40 cases of ovarian Sertoli-Leydig cell tumors. Gynecol Oncol. 2012; 127:384–389.

8. Lantzsch T, Stoerer S, Lawrenz K, Buchmann J, Strauss HG, Koelbl H. Sertoli-Leydig cell tumor. Arch Gynecol Obstet. 2001; 264:206–208.

9. McGuire WP, Hoskins WJ, Brady MF, Kucera PR, Partridge EE, Look KY, et al. Cyclophosphamide and cisplatin compared with paclitaxel and cisplatin in patients with stage III and stage IV ovarian cancer. N Engl J Med. 1996; 334:1–6.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download