Abstract
Purpose
Intrathecal morphine pump (ITMP) infusion therapy is efficient in managing malignant and nonmalignant chronic pain refractory to standard treatment. However, the high cost of an ITMP is the greatest barrier for starting a patient on ITMP infusion therapy. Using the revised Korean reimbursement guidelines, we investigated the cost effectiveness of ITMP infusion therapy and conducted a patient survey.
Materials and Methods
A retrospective chart review of 12 patients who underwent ITMP implantation was performed. Morphine dose escalation rates were calculated, and numeric rating scale (NRS) scores were compared before and after ITMP implantation. We surveyed patients who were already using an ITMP as well as those who were candidates for an ITMP. All survey data were collected through in-person interviews over 3 months. Data on the cost of medical treatment were collected and projected over time.
Results
The NRS score decreased during the follow-up period. The median morphine dose increased by 36.9% over the first year, and the median time required to reach a financial break-even point was 24.2 months. Patients were more satisfied with the efficacy of ITMP infusion therapy than with conventional therapy. The expected cost of ITMP implantation was KRW 4000000–5000000 in more than half of ITMP candidates scheduled to undergo implantation.
Cancer mortality rates have continuously decreased since the development of new anti-cancer drugs and advances in radiation therapy and surgical techniques. According to the Korean Ministry of Health and Welfare (2013), the number of cancer patients has exceeded 1 million in Korea, with a cancer survival rate of 64.1%.1 For this reason, some physicians believe that cancer should be reclassified as a "chronic disease." Interestingly, after receiving a cancer diagnosis, patients frequently have a greater fear of the pain they will encounter during treatment than of the difficulties of the cancer treatment process or death.23 Cancer pain control is the most critical determinant of quality of life for cancer patients; however, multiple studies have reported that 40–70% of cancer patients complained that their cancer pain was undertreated.45
Intrathecal morphine infusion is used to provide strong pain relief by directly infusing low doses of morphine into the cerebrospinal fluid surrounding the opioid receptors. This analgesic technique reduces the incidence of the adverse effects caused by systemic morphine administration, including nausea, vomiting, somnolence, constipation, dyspnea, and neurotoxicity. Intrathecal morphine provides analgesia equal to that of oral morphine alone at 1/300 the oral dose. Accordingly, intrathecal morphine infusion was introduced as a method of cancer pain management in 1979 by Wang, et al.,6 and its efficacy has been confirmed by others.7 The implantable intrathecal morphine pump (ITMP), which was invented in the 21st century, manages pain in patients with terminal cancer or idiopathic chronic pain better than oral narcotics due to its ability to continuously deliver morphine to the intrathecal space at a constant rate.89 The first surgically-implanted ITMP in Korea was in 2008, to treat cancer and chronic pain.10
In a study of intrathecal morphine administered to 119 patients with cancer-related pain, Roberts, et al.11 and Rauck, et al.12 reported that the median numeric rating scale (NRS) score decreased significantly from 6.1 to 4.2 and that the incidence of opioid-associated adverse effects was significantly lower after 1 month of therapy. Intrathecal morphine infusion is also effective in treating patients who experience insufficient pain control with previous therapies.13 However, intrathecal morphine infusion is quite expensive. A recent survey of healthcare practitioners who actively implant drug-delivery systems found that 40.5% of those surveyed believed that the cost of implantation was the greatest barrier to initiating intrathecal therapy.14 In July 2014, the Korean government began covering 50% of this cost in select patients. Reimbursement is currently approved only in patients with all of the following conditions: long-term severe pain (persistent NRS score ≥7), insufficient pain control for >6 months when using other analgesic methods (e.g., oral medications, nerve block), patient life expectancy >1 year, and cancer pain that is unresponsive to high doses of oral morphine or an equivalent dose of another narcotic analgesic. This last criterion may also be fulfilled in patients with a >1-year life expectancy who are unable to tolerate opioid analgesics due to related adverse effects. Therefore, we expect that more patients will receive ITMP implants, as the costs are covered.
In this study, we conducted a retrospective chart review of patients who had received an ITMP implant since the introduction of the device in Korea. Analyses focused on the clinical condition of patients after implantation and on a variety of clinical outcomes related to the intrathecal morphine infusion treatment processes. Furthermore, we conducted a survey of patients eligible for reimbursement (based on official reimbursement guidelines for intrathecal morphine infusion therapy) and investigated their intention to undergo ITMP implantation.
This study was performed in two phases. In the first phase, patients who previously underwent implantation of an ITMP were surveyed, and their medical records were retrospectively reviewed. In the second phase, patients who were likely candidates for future implantation were surveyed. In patients who had already undergone ITMP implantation, surgical treatment before ITMP placement was examined, and NRS pain scores were compared before and after implantation. The change in morphine dose during ITMP treatment was also investigated.
Hospital administration data were surveyed to investigate the costs associated with the analgesic protocol. Payments for medical services performed at facilities other than Seoul National University Hospital were not included in our study. Medication costs were investigated at pharmacies close to Seoul National University Hospital. The total cost prior to ITMP implantation included the costs of medical services, interventions, procedures, and medications. The total cost after ITMP implantation included outpatient medical costs, analgesics for breakthrough pain, and ITMP refills. The cost of medical services during the treatment period, expressed in KRW/day, was divided into pre- and post-ITMP implantation segments. Annual percent escalation in daily opioid dosage was calculated as a yearly average of all patients using the starting dose, final dose, and duration throughout the year. The survey was conducted by the Department of Anesthesiology and Pain Medicine at Seoul National University Hospital in patients who underwent ITMP implantation between 2008 and 2014. Patient satisfaction following ITMP implantation was rated on a five-point Likert scale. Among the 19 patients who had an ITMP implanted, eight had cancer pain, six had complex regional pain syndrome (CRPS), four had failed back surgery syndrome (FBSS), and one had diabetic neuropathy. In-person surveys could not be conducted in seven patients, as six had died and one could not be contacted. In the remaining patients, oral permission was obtained, and the survey was administered through an in-person interview. The questionnaire for patients implanted with an ITMP is shown in Fig. 1.
A survey was also administered to patients who were potential candidates for future ITMP implantation. Patients were interviewed on an outpatient basis and selected based on the following criteria: patients with cancer pain who were unable to receive narcotic medication due to opioid-related adverse effects, patients with cancer pain using >200 mg oral morphine per day (or an equivalent dosage of another narcotic analgesic), patients experiencing continuous pain of grade 7 or higher on the 11-point NRS, and patients experiencing inadequate analgesia for longer than 6 months despite continuous and sufficient pain treatment. During the survey, the price of the implantable pump, its advantages, and the adverse effects were explained to patients, who were then given a questionnaire regarding their willingness to undergo pump implantation. If the patient was not interested, they were asked why they would decline the device. Patients completed the survey over a 3-month period (May to August 2014). The questionnaire administered to candidates for future implantation is shown in Fig. 2.
The Wilcoxon signed rank test was used to compare NRS scores before and after ITMP implantation, which are expressed as median values. The daily costs before and after ITMP implantation were compared. The medical cost before ITMP implantation was estimated assuming that daily medications remained unchanged until death. The true patient cost of ITMP implantation was divided by the post-implantation duration. The monthly median cost of analgesic treatment after ITMP implantation was determined for all patients and compared with the projected monthly median cost before ITMP implantation to determine which pain management method was more cost effective. The morphine-equivalent dose was calculated in patients who were candidates for future ITMP implantation. The statistical significance of differences between the malignant pain and non-malignant pain groups was determined using the Mann-Whitney U-test.
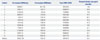
Nineteen patients were implanted with an ITMP (Medtronic SynchroMed II® pump, Medtronic, Inc., Minneapolis, MN, USA) between March 2008 and July 2014 to manage uncontrolled pain. Seven patients were excluded from analyses, as they had died or could not answer the survey questions. Therefore, 12 patients were ultimately included in the analyses. The demographic information of these 12 patients is summarized in Table 1.
All procedures were performed at the pain clinic of Seoul National University Hospital by one or two surgeons. Intrathecal access to the spine was gained under fluoroscopic guidance. In one patient (case 5), the pump and catheter were removed due to a blocked catheter, and a new pump was implanted at a different site. One patient suffered from continuous itching, and another patient complained of constipation. Nine patients reported no adverse effects following ITMP implantation. Opioid tolerance was not observed in any patient. The morphine dosage of all patients increased during the treatment period (Fig. 3). The median (25th, 75th percentiles) daily dose of morphine was initially 0.24 (0.20, 0.71) mg/day, but this increased to 1.51 (0.94, 3.5) mg/day at the last follow-up visit. The median infusion rate of morphine increased most rapidly during the first year after implantation, by 36.9%. However, in the second year, no significant increases in morphine dose were observed. In addition, 11 of 12 patients preferred ITMP over previously used pain management techniques and considered it superior to conventional treatments. Only one patient did not answer this question (Fig. 4).
The 12 patients surveyed included six patients with CRPS, four patients with FBSS, one patient with diabetic neuropathy, and one patient with breast cancer and lumbar metastasis. Seven patients with cancer pain were excluded from these analyses, as they had died from terminal cancer. All surveyed patients reported severe pain prior to ITMP implantation, as reflected by a median NRS pain score of 10 (10, 10) and shown in Table 1. After ITMP implantation, the median NRS pain score was 5 (1.62, 8), which continued to decrease during the follow-up period (Fig. 5).
The pre-implantation cost included the cost of opioid medication and pain-control procedures (e.g., interventional nerve block, analgesic injections). The post-implantation cost included ITMP drug refill, the refill kit, professional fees, and medication for breakthrough pain. The total implant cost included ITMP equipment cost, operating room fees, and professional fees. The median interval to cost effectiveness was 24.2 months (Table 2).
The results of the Patient Satisfaction Scale are shown in Table 3. Five patients were satisfied with the ITMP, six were neither satisfied nor dissatisfied with the ITMP, and one was somewhat dissatisfied. This dissatisfied patient reported that he was unable to operate the remote control by himself, making it impossible for him to immediately adjust his medication in response to sudden changes in pain.
In total, 27 patients with malignant pain and 27 patients with non-malignant pain were surveyed. The dose of oral morphine was significantly higher in the malignant pain group than in the non-malignant pain group (Fig. 6). Nausea and vomiting were the most commonly reported adverse events in both groups (Fig. 7).
Three patients reported that they were aware of ITMP implantation, leaving 51 patients who had no prior knowledge of the device. Seven of 27 patients with malignant pain and two of 27 patients with non-malignant pain indicated that they were willing to undergo ITMP implantation. Overall, 41 of 45 patients declined ITMP implantation due to the high procedural cost. The remaining four patients were uncertain as to why they did not want to receive the pump. When asked what a reasonable price would be to make them choose implantation, 51% of those who declined the procedure reported a price range of KRW 4000000–5000000 (Table 4).
Many studies have shown that an ITMP is effective in providing pain control, even at small morphine doses, indicating that this analgesic technique may help restore analgesia without alternative measures, such as opioid rotation or opioid holidays. This study also showed satisfactory pain control in patients with an ITMP implant.
Intrathecal drug dose escalation has been reported in multiple studies,15 indicating that dose escalation may be independent of the opioid delivery method. A longitudinal study examining intrathecal morphine dose escalation showed that 17% of patients with neuropathic pain and 12% of patients with other types of pain experienced dose escalation.16 In the present study, the median morphine escalation rate increased rapidly in all patients and was 36.9% during the first year of ITMP use, which was higher than that in the previous study.16 We presumed that this was due to several reasons. First, the morphine dose inevitably increases rapidly immediately after transplantation, as patients implanted with an ITMP have pain that cannot be controlled with medication or medical procedures. Their pain intensity was 10 before ITMP implantation, as shown in Table 1.
Second, the initial dose in the study was about 75% of the morphine-equivalent dose, which was calculated from oral conversion to intrathecal morphine according to standard guidelines17 in order to avoid morphine overdose complications, such as respiratory depression, pinpoint pupils, nausea, and drowsiness. Instead, patients in our study were prescribed oral morphine at a dosage equivalent to 25% of the calculated morphine dose. These observations indicated that a drug optimization process with a high escalation rate for intrathecal morphine occurred during the first year after ITMP implantation. Third, in the present study, patients with an ITMP were not prescribed any simultaneous opioid-sparing adjuvant therapy. In accordance with a previous study examining factors associated with opioid dose escalation, rapid opioid dose escalation was observed in the first 3 years after implantation in the absence of any other adjuvant therapy and in patients who had been continuously administered opioids for neuropathic pain.18
Another possible explanation for the rapid morphine escalation rates is that we predicted an initial dose for continuous ITMP based on systemic opioid usage according to old guidelines only.17 Malhotra, et al.19 attempted to minimize ongoing intrathecal dose adjustment and proposed systemic opioid dosage using the old guidelines. According to their study, to reduce potential under- or overdosing, various methods such as the use of a bolus single shot and systemic opioids using specific equations should be considered.
According to Brogan, et al.,20 the cost break-even point is reached at 7.6 months in cancer patients (n=36 patients). Essentially, in patients who are administered parenteral high-dose morphine and non-generic products, the cost of ITMP implantation is recovered at 7.6 months after implantation. As specified by the ITMP manufacturer's (Medtronic) regional data, the cost of ITMP implantation in 2014 was approximately $14900 in Korea and $35601 in the US. According to Mueller-Schwefe, et al.,21 11–22 months were required to reach the cost break-even point for patients with non-malignant pain. There are several explanations for the longer break-even point (22.4 months) observed in this study. First, outpatient medical costs and generic medications are less expensive in Korea than in the US. Second, unlike previous studies that investigated only cancer pain, this study included patients with chronic non-malignant pain. This increased the duration of the examination and treatment periods before ITMP implantation. Third, patients with chronic, non-malignant pain who were not hospitalized and who did not receive intravenous analgesics had lower costs before ITMP implantation, which lengthened the break-even point. Additionally, money spent at facilities other than Seoul National University Hospital was not included in pre-implantation costs, which may have lowered the pre-implantation costs and lengthened the break-even point.
In accordance with the Korean reimbursement guidelines announced in July 2014, 50% of ITMP costs can be reimbursed if life expectancy is greater than 1 year in patients with cancer pain who cannot take opioids due to narcotic-related adverse effects, if life expectancy is greater than 1 year in patients with cancer pain uncontrolled by high-dose opioids (oral morphine-equivalent dose ≥200 mg/day), or if the patient has refractory chronic pain that is unresponsive to other treatments for longer than 6 months. Based on our results, a median time of 24.2 months is required to reach the financial break-even point. Considering this length of time and the current ITMP costs, financial losses may occur for patients choosing to use an ITMP. Additional studies examining current ITMP-associated costs are required. One concern that cannot be ignored is that the life span of an ITMP may be less than six years.18
Patients with cancer pain who underwent ITMP implantation were administered a significantly higher oral morphine-equivalent dose and had higher incidences of morphine-related adverse effects than patients with chronic non-malignant pain. Ver Donck, et al.22 also reported that support for intrathecal drug administration is stronger for managing cancer pain than for non-cancer pain.2223 Consequently, the demand for ITMPs is expected to be higher among patients with cancer pain. However, as shown in Table 4, the cost-effectiveness of ITMP implantation must also be considered, as implantation costs are expected to be between KRW 4000000 and KRW 5000000 in over 50% of ITMP candidates.
First, only one patient with cancer pain was included in this study. Eight of nineteen patients who underwent ITMP implantation had cancer pain. However, seven of these eight patients died before completing the survey. Therefore, it is highly unlikely that the 24.2-month interval to reach cost effectiveness is applicable to cancer patients. Furthermore, this study included only patients who underwent ITMP implantation at Seoul National University Hospital, and financial outcomes may vary as a result of differences in medical care costs between hospitals.
Second, although the equivalent dose of breakthrough oral medication after ITMP implantation was very low compared to that required with ITMP, further studies are required to investigate the additional costs of controlling breakthrough pain and/or performing interventional procedures for managing additional pain in other locations that may not be covered by an IT pump.
Finally, the rate of refusal for ITMP implantation was higher than expected, largely due to the high cost of ITMP implantation. Patients were informed that the cost was KRW 15000000; however, this was before the Korean government approved a 50% reimbursement for certain patients. We expect that the reduced cost of ITMP implantation will increase the proportion of candidates who elect to undergo the procedure.
Figures and Tables
 | Fig. 2Questionnaire completed by patients who were candidates for intrathecal morphine pump implantation. |
 | Fig. 4The percentage of patients who preferred ITMP therapy over previous pain-management strategies. Data indicate the percentage (%) of patients stating that ITMP was better than conventional therapy. ITMP, intrathecal morphine pump. |
 | Fig. 5Comparison of numeric rating scale (NRS) pain scores before and after ITMP implantation. Z-statistic (based on positive ranks)=-3.068, p<0.001. ITMP, intrathecal morphine pump. |
 | Fig. 6Comparison of morphine-equivalent dose between patients with malignant and non-malignant pain. |
ACKNOWLEDGEMENTS
Korea Health Industry Development Institute (KHIDI). No.HI13C-2197-020013. We would like to thank to KHIDI for their assistance in performing this survey.
References
1. Ministry of Health and Welfare. accessed on 2014 Jul 2. Available at: http://www.mohw.go.kr.
2. Jo HS, Kwon MS, Jung SM, Lee BY. Awareness of cancer and cancer screening by Korean community residents. Asian Pac J Cancer Prev. 2014; 15:4939–4944.

3. Nuland SB. Physician-assisted suicide and euthanasia in practice. N Engl J Med. 2000; 342:583–584.

4. Von Roenn JH, Cleeland CS, Gonin R, Hatfield AK, Pandya KJ. Physician attitudes and practice in cancer pain management. A survey from the Eastern Cooperative Oncology Group. Ann Intern Med. 1993; 119:121–126.

6. Wang JK, Nauss LA, Thomas JE. Pain relief by intrathecally applied morphine in man. Anesthesiology. 1979; 50:149–151.

7. Wiffen PJ, Wee B, Moore RA. Oral morphine for cancer pain. Cochrane Database Syst Rev. 2013; 7:CD003868.

8. Onofrio BM. Treatment of chronic pain of malignant origin with intrathecal opiates. Clin Neurosurg. 1983; 31:304–315.

9. Nguyen H, Hassenbusch SJ. Cost-effectiveness of intraspinal drug delivery for chronic pain. Semin Pain Med. 2004; 2:43–45.

10. Lee SJ, Nam SK, Kim JH, Kim HJ, Lee SC, Kim YC. Implantation of an intrathecal drug administration system - a report of two cases. Korean J Pain. 2009; 22:68–73.

11. Roberts LJ, Finch PM, Goucke CR, Price LM. Outcome of intrathecal opioids in chronic non-cancer pain. Eur J Pain. 2001; 5:353–361.

12. Rauck RL, Cherry D, Boyer MF, Kosek P, Dunn J, Alo K. Long-term intrathecal opioid therapy with a patient-activated, implanted delivery system for the treatment of refractory cancer pain. J Pain. 2003; 4:441–447.

13. Upadhyay SP, Mallick PN. Intrathecal drug delivery system (IDDS) for cancer pain management: a review and updates. Am J Hosp Palliat Care. 2012; 29:388–398.

14. Deer TR, Krames E, Levy RM, Hassenbusch SJ 3rd, Prager JP. Practice choices and challenges in the current intrathecal therapy environment: an online survey. Pain Med. 2009; 10:304–309.

15. Duarte RV, Raphael JH, Haque MS, Southall JL, Ashford RL. A predictive model for intrathecal opioid dose escalation for chronic non-cancer pain. Pain Physician. 2012; 15:363–369.
16. Mekhail N, Mahboobi R, Farajzadeh Deroee A, Costandi S, Dalton J, Guirguis M, et al. Factors that might impact intrathecal drug delivery (IDD) dose escalation: a longitudinal study. Pain Pract. 2014; 14:301–308.

18. Atli A, Theodore BR, Turk DC, Loeser JD. Intrathecal opioid therapy for chronic nonmalignant pain: a retrospective cohort study with 3-year follow-up. Pain Med. 2010; 11:1010–1016.

19. Malhotra VT, Root J, Kesselbrenner J, Njoku I, Cubert K, Gulati A, et al. Intrathecal pain pump infusions for intractable cancer pain: an algorithm for dosing without a neuraxial trial. Anesth Analg. 2013; 116:1364–1370.
20. Brogan SE, Winter NB, Abiodun A, Safarpour R. A cost utilization analysis of intrathecal therapy for refractory cancer pain: identifying factors associated with cost benefit. Pain Med. 2013; 14:478–486.

21. Mueller-Schwefe G, Hassenbusch SJ, Reig E. Cost effectiveness of intrathecal therapy for pain. Neuromodulation. 1999; 2:77–87.

22. Ver Donck A, Vranken JH, Puylaert M, Hayek S, Mekhail N, Van Zundert J. Intrathecal drug administration in chronic pain syndromes. Pain Pract. 2014; 14:461–476.

23. Hayek SM, Deer TR, Pope JE, Panchal SJ, Patel VB. Intrathecal therapy for cancer and non-cancer pain. Pain Physician. 2011; 14:219–248.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download