Abstract
Purpose
Data comparing the clinical benefits of medical treatment with those of percutaneous coronary intervention (PCI) in an elderly population with angina pectoris are limited. Therefore, we evaluated the efficacy of elective PCI versus optimal medical treatment (OMT) in elderly patients (between 75 and 84 years old) with angina pectoris.
Materials and Methods
One hundred seventy-seven patients with significant coronary artery stenosis were randomly assigned to either the PCI group (n=90) or the OMT group (n=87). The primary outcome was a composite of major adverse events in the 1-year follow-up period that included cardiovascular death, non-fatal myocardial infarction, coronary revascularization, and stroke.
Results
Major adverse events occurred in 5 patients (5.6%) of the PCI group and in 17 patents (19.5%) of the OMT group (p=0.015). There were no significant differences between the PCI group and the OMT group in cardiac death [hazard ratio (HR) for the PCI group 0.454; 95% confidence interval (CI) 0.041–5.019, p=0.520], myocardial infarction (HR 0.399; 95% CI 0.039–4.050, p=0.437), or stroke (HR 0.919; 95% CI 0.057–14.709, p=0.952). However, the PCI group showed a significant preventive effect of the composite of major adverse events (HR 0.288; 95% CI 0.106–0.785, p=0.015) and against the need for coronary revascularization (HR 0.157; 95% CI 0.035–0.703, p=0.016).
The proportion of older patients within the general population is gradually increasing, especially in advanced countries. Coronary artery disease is the leading cause of death in the elderly, and chronic conditions associated with coronary artery disease are an important health issue.1 In daily clinical practice, medical treatment rather than percutaneous coronary intervention (PCI) is typically preferred in elderly patients due to a higher incidence of multiple extra-cardiac comorbidities, fragile physical performance, and an increased risk of complications resulting from this invasive procedure in this population. Therefore, elderly patients have mostly been excluded from study populations in randomized PCI trials. Nevertheless, data indicate that PCI is an effective treatment option for myocardial infarction in elderly patients.23 As the technical skills of those administering PCI advance along with the device technology itself, PCI-related adverse cardiovascular events have progressively decreased over time in elderly patients.456 Indeed, a recent observational study reported that PCI reduced mortality in older patients with acute coronary syndrome.7 Furthermore, PCI may alleviate symptoms and improve the quality of life in elderly patients. However, there is limited data directly comparing the effects of PCI to that of medical treatment in elderly patients with angina pectoris. Therefore, the objective of this study was to compare clinical outcomes of elderly patients (≥75 years old) with angina pectoris who were treated with optimal medical treatment (OMT) to those who were treated with elective PCI with drug-eluting stent implantation.
This study was a prospective, multicenter, randomized clinical trial conducted at six centers in Korea (ClinicalTrials.gov, NCT01508663). Inclusion criteria were patients between 75 and 84 years of age; a clinical diagnosis of stable angina or unstable angina (Braunwald classification IB); and significant stenosis in at least one proximal epicardial coronary artery (diameter stenosis of ≥70% by visual estimation). Exclusion criteria were a clinical diagnosis of unstable angina (Braunwald classification IIB or IIIB) or acute myocardial infarction; left ventricular ejection fraction less than 30%; history of prior PCI within 6 months; small vessel lesions not suitable for PCI; or a non-cardiac morbidity with a life expectancy less than 2 years. This study was approved by the Institutional Review Board of each institute, and written informed consent was obtained from each patient.
Using an interactive web-based response system, patients were randomly assigned into either the PCI group or the OMT group. In the PCI group, patients were randomly assigned in a 1:1 ratio to receive the Resolute zotarolimus-eluting stent (Endeavor-Resolute stent, Medtronic vascular, Santa Rosa, CA, USA) or the everolimuseluting stent (Xience, Abbott Vascular, Santa Clara, CA, USA). All patients in the PCI group received at least 75 mg of aspirin and a loading dose of 300 mg of clopidogrel at least 12 hours pre-PCI. Unfractionated heparin was administered to maintain the activated clotting time >250 seconds. All PCI procedures were performed according to current standard techniques. Post-procedure, dual antiplatelet therapy with aspirin (100 mg) and clopidogrel (75 mg) daily was prescribed for 12 months. Procedural success was defined as the achievement of a final in-stent diameter stenosis of 30% or less by online quantitative coronary angiographic analysis or visual assessment over the entire stent length, with normal coronary-artery flow. Medical treatment in both PCI and OMT groups included aspirin, statin, isosorbide nitrate, calcium-channel blocker, long-acting beta-blocker, and angiotensin converting enzyme inhibitor or angiotensin receptor blocker alone or in combination. All patients were scheduled to visit the clinic at 3, 6, 9, and 12 months after coronary angiography. Revascularization was recommended when patients had recurrent or refractory angina symptom after discharge from treatment by randomization.
Data were collected from and documented in electronic clinical research forms by dedicated research coordinators. The primary end point was the composite of cardiovascular death, stroke, non-fatal myocardial infarction, and coronary revascularization for 1 year after the randomization. Clinical events were defined according to the Academic Research Consortium.8 All deaths were considered cardiac deaths unless a definite non-cardiac cause was established. Myocardial infarction was defined as the presence of clinical symptoms, electrocardiographic changes, or abnormal imaging findings of myocardial infarction, combined with an increase in the creatine kinase myocardial band fraction above the upper normal limits or an increase in troponin-T/troponin-I to greater than the 99th percentile of the upper normal limit. Clinical assessment was performed during a scheduled visit to an outpatient clinic.
In the PCI group, quantitative coronary angiographic analysis was performed using an off-line quantitative coronary angiographic system (CASS system, Pie Medical Instruments, Maastricht, the Netherlands), before and after stent implantation, by analysts in an independent core laboratory at the Cardiovascular Research Center, Seoul, Korea. Using the guiding catheter for magnification-calibration, the diameters of the reference vessel and the minimal luminal diameter were measured before and after stenting from diastolic frames in a single matched view showing the smallest minimal luminal diameter.
The sample size was calculated using a two-sample inequality test. Based on previous data showing the composite of cardiovascular death, stroke, nonfatal myocardial infarction, or coronary revascularization occurred in 23.5% of the PCI-treated group and in 30.0% of the OMT-treated group,910 we assumed that PCI would reduce the composite events by 6.5% compared to the OMT group in our study. Assuming a two-sided alpha level of 0.05, statistical power of 80%, and estimated dropout rate of 10%, we calculated 800 hundred patients were needed for each arm.
For comparing categorical variables we conducted the χ2 test or Fisher's exact test. To compare continuous variables the Student t-test was conducted. Cumulative incidences of composite events at 12 months (the primary outcomes) were calculated using Kaplan-Meier estimates. Comparison between the two groups was performed using the log-rank test. Univariate and multivariate logistic regression models were applied to determine risk factors for the composite events. Statistical analysis was performed using the SPSS software (version 18.0.0; SPSS Inc., Chicago, IL, USA). A value of p<0.05 was considered statistically significant.
Patients were enrolled between December 2010 and June 2012. The recruitment process was prematurely terminated due to difficulty in enrolling patients due to physician or patient preference. During the study period, 182 patients were included in this study. A total of 5 patients were excluded. Three patients withdrew informed consent, and 2 patients violated study protocol. Of the remaining 177 patients, 87 OMT group patients and 90 PCI group patients (zotarolimus-eluting stent in 46 patients and everolimus-eluting stent in 44 patients) were included in the final analysis. Baseline clinical characteristics were similar between the two groups (Table 1). Lesion and procedural characteristics of the PCI group are listed in Table 2. The transradial approach was performed at a similar rate between two groups (58.9% in PCI and 60.9% in OMT, p=0.783). All PCI procedures were successfully performed without complications.
One year clinical outcomes between of both groups are shown in Table 3. Although cardiac mortality, myocardial infarction, and stroke were not statistically different between the two groups, coronary revascularization was significantly greater in the OMT group than in the PCI group (13.8% vs. 2.2%, respectively, p=0.016). The composite of adverse events during the one-year follow-up period occurred in five patients (5.6%) in the PCI group and in 17 patients (19.5%) in OMT group (log rank p=0.010) (Fig. 1). The improved outcome primarily resulted from the difference of coronary revascularization due to recurrent angina in elderly patients.
Of these patients in the PCI group, major adverse events included one stroke in a patient with a zotarolimus-eluting, one cardiac death, one myocardial infarction, and two target-lesion revascularization procedures were conducted in everolimuseluting stent-treated patients (p=0.152). By multivariate Cox regression analysis, PCI was an independent predictor for the composite of adverse events (hazard ratio=0.285, 95% confidence interval 0.102–0.796, p=0.017) (Table 4).
This prospective randomized study showed that, compared to OMT, PCI reduces major adverse outcomes in elderly patients ≥75 years of age.
The Trial of Invasive versus Medical Therapy in Elderly Patients with Chronic Symptomatic Coronary Artery Disease (TIME) trial was the first randomized controlled trial to compare invasive revascularization including PCI and coronary artery bypass surgery with OMT in elderly patients (≥75 years) with stable angina. In that study, invasive revascularization reduced adverse cardiovascular events, an effect mainly due to reduced re-hospitalization with medically uncontrolled angina symptoms during the 6 months of follow-up.11 However, it is important to note that differences in symptom control and quality of life improvement between the two study groups were not observed within 1 year of follow-up.12 Furthermore, after 4 years of follow-up, the long term survival rate was similar between the invasive and medically treated groups.13 However, symptom relief and improved quality of life in the invasive treatment group, compared to the medical treatment group, was maintained over the duration of the 4-year follow-up period.13 In the TIME trial, coronary revascularization, including both PCI and coronary bypass graft surgery, was compared with medical therapy. This made it difficult to evaluate the effect of PCI alone on long-term clinical outcomes. Furthermore, PCI was performed with a bare-metal stent. With evolving PCI technologies and techniques, as well as adjunctive medical therapy, adverse cardiovascular events after PCI have significantly decreased over time in elderly patients.456 In the current study, PCI using second-generation drug-eluting stents was directly compared with medical therapy in elderly patients.
The importance of statin therapy for the treatment and prevention of coronary artery disease has been increasingly emphasized over the last decade. In the TIME trial, about 20% of patients were on statin treatment, while in our study, almost all patients took a statin. In the TIME trial, major adverse cardiovascular events during the 1-year follow-up occurred in 25.5% of the invasive revascularization group and in 64.2% of the medical treatment group; all-cause mortality was 11.1% and 8.1%, respectively.12 In the present study, the rate of major adverse cardiovascular events was significantly lower. Advances in PCI techniques, accumulated technical experience, and advances in devices, as well as medical therapy, likely improved the clinical outcomes for elderly patients in both the PCI and OMT groups included in our study.
Over the past decade, the average life expectancy in Korea has increased about 5 years, and is now greater than 75 years.14 Furthermore, a reduced rate of disability in older Koreans has led to a substantially improved functional status of this population.15 Similar trends of prolonged survival and declined disability are observed in developed countries.161718 Despite improved physical functioning in elderly population, the prevalences of chronic diseases like ischemic heart disease have continued.1419 In elderly patients with angina pectoris, relieving angina symptoms may lead a higher quality of life over the increased life expectancy. Treating angina pectoris in elderly patients with medical treatment alone may increase in the suffering and psychological distress related to the condition. A recent study reported that the quality of life and symptom relief in octogenarian patients with coronary artery disease following PCI improved to a level similar to that observed in younger patients.20 In terms of cost-effectiveness, one study reported that invasive treatment had a similar benefit to medical management in elderly patients with chronic angina symptoms.21 However, within clinical practice, PCI is underused in older patients (≥75 years old) with acute coronary syndrome, especially in those with more complex risk factors.7
Advanced age is an independent risk factor for mortality and morbidity in PCI.422 This safety issue is an important factor when considering PCI in elderly patients. The higher prevalence of diffuse disease, severe calcification, and tortuosity in the elderly may explain the high risk of complications and procedural failure in this population. Over the last 10 years, therapeutic developments have improved clinical outcomes following PCI.45623 Increased frequency of the transradial approach has reduced vascular complications and major bleeding.2425 Elderly patients have a significantly higher risk of arterial access complications. Therefore, a lower incidence of vascular complications may be particularly beneficial in this patient population.26 In the present study, transradial PCI was performed in about 60% of patients without any resulting complications. Moreover, a recent study from the SHINANO registry, in which 63.2% of the procedures were transradial, reported that the procedure success rate and in-hospital major adverse cardiovascular outcomes in an octogenarian cohort were similar to those observed in younger patients who underwent elective PCI.27 Similarly, elective PCI in elderly patients had favorable clinical outcomes in a study from the New York State Angioplasty Registry.22 In the present study, PCI had favorable outcomes and did not increase procedure-related or bleeding complications.
The present study has limitations. First, statistical power was reduced because of the small number of patients enrolled in this study. Second, the results of this study may not be applicable to patients with myocardial infarction or asymptomatic patients. Third, the decision of revascularization in re-admitted patients was at the discretion of physicians, although we recommended revascularization in patients with recurrent angina. Furthermore, we have not assessed quality of life, but most recurrently symptomatic patients were treated by revascularization.
In summary, PCI improved chest symptoms and reduced re-admission related to recurrent angina, compared to optimal medical treated elderly patients; meanwhile, no reductions in mortality and myocardial infarction were noted. These data indicate that PCI is effective and feasible in symptomatic elderly patients with angina pectoris. Chronological age alone should not be considered as a contraindication for PCI, and PCI should be considered as a primary treatment strategy in this patient population.
Figures and Tables
Fig. 1
Rate of composite adverse events for the 1 year follow-up duration. OMT, optimal medical treatment; PCI, percutaneous coronary intervention; CI, confidence interval.
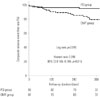
Table 1
Baseline Clinical Characteristics

Table 2
Angiographic & Procedural Characteristics in PCI Group

Table 3
Clinical Outcomes through 1 Year

Table 4
Univariate and Multivariate Cox Regression Analysis for Prediction of Major Adverse Cardiac Events

ACKNOWLEDGEMENTS
This study was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare&Family Affairs, Republic of Korea (Nos. A085136 and A102064) and the Cardiovascular Research Center, Seoul, Korea.
References
1. Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2010. Natl Vital Stat Rep. 2013; 61:1–117.
2. Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The Task Force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2011; 32:2999–3054.
3. Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al. 2011 ACCF/AHA Focused Update Incorporated Into the ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2011; 123:e426–e579.
4. Batchelor WB, Anstrom KJ, Muhlbaier LH, Grosswald R, Weintraub WS, O'Neill WW, et al. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: results in 7,472 octogenarians. National Cardiovascular Network Collaboration. J Am Coll Cardiol. 2000; 36:723–730.

5. From AM, Rihal CS, Lennon RJ, Holmes DR Jr, Prasad A. Temporal trends and improved outcomes of percutaneous coronary revascularization in nonagenarians. JACC Cardiovasc Interv. 2008; 1:692–698.

6. Rao SV, Hess CN, Dai D, Green CL, Peterson ED, Douglas PS. Temporal trends in percutaneous coronary intervention outcomes among older patients in the United States. Am Heart J. 2013; 166:273–281.e4.

7. Di Bari M, Balzi D, Fracchia S, Barchielli A, Orso F, Sori A, et al. Decreased usage and increased effectiveness of percutaneous coronary intervention in complex older patients with acute coronary syndromes. Heart. 2014; 100:1537–1542.

8. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–2351.
9. Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007; 356:1503–1516.

10. Teo KK, Sedlis SP, Boden WE, O'Rourke RA, Maron DJ, Hartigan PM, et al. Optimal medical therapy with or without percutaneous coronary intervention in older patients with stable coronary disease: a pre-specified subset analysis of the COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive druG Evaluation) trial. J Am Coll Cardiol. 2009; 54:1303–1308.
11. TIME Investigators. Trial of invasive versus medical therapy in elderly patients with chronic symptomatic coronary-artery disease (TIME): a randomised trial. Lancet. 2001; 358:951–957.
12. Pfisterer M, Buser P, Osswald S, Allemann U, Amann W, Angehrn W, et al. Outcome of elderly patients with chronic symptomatic coronary artery disease with an invasive vs optimized medical treatment strategy: one-year results of the randomized TIME trial. JAMA. 2003; 289:1117–1123.

13. Pfisterer M. Trial of Invasive versus Medical therapy in Elderly patients Investigators. Long-term outcome in elderly patients with chronic angina managed invasively versus by optimized medical therapy: four-year follow-up of the randomized Trial of Invasive versus Medical therapy in Elderly patients (TIME). Circulation. 2004; 110:1213–1218.

14. Yang S, Khang YH, Harper S, Davey Smith G, Leon DA, Lynch J. Understanding the rapid increase in life expectancy in South Korea. Am J Public Health. 2010; 100:896–903.

15. Jang SN, Kim DH. Trends in the health status of older Koreans. J Am Geriatr Soc. 2010; 58:592–598.

16. Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002; 288:3137–3146.

17. Aijänseppä S, Notkola IL, Tijhuis M, van Staveren W, Kromhout D, Nissinen A. Physical functioning in elderly Europeans: 10 year changes in the north and south: the HALE project. J Epidemiol Community Health. 2005; 59:413–419.

18. Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proc Natl Acad Sci U S A. 2006; 103:18374–18379.

19. Murabito JM, Pencina MJ, Zhu L, Kelly-Hayes M, Shrader P, D'Agostino RB Sr. Temporal trends in self-reported functional limitations and physical disability among the community-dwelling elderly population: the Framingham heart study. Am J Public Health. 2008; 98:1256–1262.

20. Johnman C, Mackay DF, Oldroyd KG, Pell JP. Quality of life following percutaneous coronary interventions in octogenarians: a systematic review. Heart. 2013; 99:779–784.

21. Claude J, Schindler C, Kuster GM, Schwenkglenks M, Szucs T, Buser P, et al. Cost-effectiveness of invasive versus medical management of elderly patients with chronic symptomatic coronary artery disease. Findings of the randomized trial of invasive versus medical therapy in elderly patients with chronic angina (TIME). Eur Heart J. 2004; 25:2195–2203.
22. Feldman DN, Gade CL, Slotwiner AJ, Parikh M, Bergman G, Wong SC, et al. Comparison of outcomes of percutaneous coronary interventions in patients of three age groups (<60, 60 to 80, and >80 years) (from the New York State Angioplasty Registry). Am J Cardiol. 2006; 98:1334–1339.

23. Choi YJ, Kim JB, Cho SJ, Cho J, Sohn J, Cho SK, et al. Changes in the Practice of Coronary Revascularization between 2006 and 2010 in the Republic of Korea. Yonsei Med J. 2015; 56:895–903.

24. Achenbach S, Ropers D, Kallert L, Turan N, Krähner R, Wolf T, et al. Transradial versus transfemoral approach for coronary angiography and intervention in patients above 75 years of age. Catheter Cardiovasc Interv. 2008; 72:629–635.

25. Louvard Y, Benamer H, Garot P, Hildick-Smith D, Loubeyre C, Rigattieri S, et al. Comparison of transradial and transfemoral approaches for coronary angiography and angioplasty in octogenarians (the OCTOPLUS study). Am J Cardiol. 2004; 94:1177–1180.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download