Abstract
Purpose
We evaluated the hemodynamic statuses of patients after partial closure of atrial septal defects with fenestration due to pulmonary hypertension.
Materials and Methods
Seventeen adult patients underwent partial atrial septal defect closure and follow-up cardiac catheterization. We analyzed hemodynamic data and clinical parameters before and after closure.
Results
The median age at closure was 29 years old. The baseline Qp/Qs was 1.9±0.6. The median interval from the operation to the cardiac catheterization was 27 months. The CT ratio decreased from 0.55±0.07 to 0.48±0.06 (p<0.05). The mean pulmonary arterial pressure decreased from 50.0±11.5 mm Hg to 32.5±14.4 mm Hg (p<0.05), and the pulmonary resistance index decreased from 9.2±3.6 Wood units*m2 to 6.3±3.8 Wood units*m2 (p<0.05). Eleven patients (64.7%) continued to exhibit high pulmonary resistance (over 3.0 Wood units*m2) after closure. These patients had significantly higher pulmonary resistance indices and mean pulmonary arterial pressures based on oxygen testing before the partial closures (p<0.05). However, no significant predictors of post-closure pulmonary hypertension were identified.
Pulmonary hypertension (PH) is frequently encountered in patients of advanced age with atrial septal defects (ASD). In patients with overt PH, ASD closure might result in worse prognoses than not undergoing ASD closure.1 Based on guidelines for operability in patients with PH associated with ASD,234 shunt closure is usually discouraged in the presence of severe PH or Eisenmenger syndrome. Preoperative PH is a predictive factor for mortality and cardiac morbidity after shunt closure.56 However, recent advances in PH treatment have led to ASD closures even in patients with severe PH who are considered inoperable.78 ASD closure with fenestration is an important option for such high-risk patients.91011 Few studies have performed hemodynamic evaluations in patients after partial closures of ASDs with fenestration. We evaluated changes in hemodynamic parameters after partial closure of ASD and the clinical implications of fenestration in ASD closure in patients with PH.
This retrospective study enrolled 17 patients over 18 years of age. Fourteen patients were female, and three were male. All of the patients enrolled in our study were diagnosed with PH associated with ASD at the Samsung Medical Center and Sejong Cardiovascular Center between January 1, 2001 and December 31, 2012. PH was defined as a mean pulmonary arterial pressure (mPAP) greater 25 mm Hg as assessed by cardiac catheterization regardless of pulmonary wedge pressure or pulmonary resistance.12 The patients underwent follow-up cardiac catheterization after ASD closure with fenestration for hemodynamic evaluation. The Institutional Review Board approved this study and waived the need for consent from the patients or their parents.
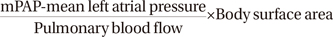
All 17 patients were diagnosed via echocardiography with ASDs that were sufficiently large enough to cause PH. We excluded patients with liver disease, lung disease, or connective tissue disease as concomitant causes of PH. PH was confirmed by invasive cardiac catheterization. The cardiac catheterizations were performed on fully conscious patients. Oxygen consumption was measured before catheterization for each patient, and pulmonary blood flow was obtained using the Fick principle. The pressure and oxygen contents were measured at the corresponding sites. The pulmonary vascular resistance index (PVRI) was derived as follows:
Vasodilator testing with 100% oxygen was performed through a properly fitted face mask. Based on pre-closure PVRI, the patients were classified as mild (≤6), moderate (6<PVRI≤9) or severe (>9 Wood units*m2) to observe the post-closure PVRI of each group.4
ASD closure was chosen if the patient had exhibited 1) a sizable ASD, 2) PH (mean PAP >25 mm Hg) with oxygen responsiveness (reduction of the PVRI by more than 20% of baseline), and 3) evidence of volume overload (Qp/Qs>1.5). The fenestrations were made with a punch on the surgical patch or via the use of a dilator on an Amplatzer Septal Occluder (ASO, St. Jude Medical Inc., St. Paul, MN, USA). The fenestration size depended on body size and the degree of PH, and was typically more than 5 mm.
We collected clinical assessments of World Health Organization functional class, age at the time of the operation, size of fenestration at the time of closure, and the prescribed pulmonary vasodilators after partial closure from medical records.
Follow-up cardiac catheterization was performed within one year after partial closure. Immediately prior to catheterization, echocardiography was performed to confirm the shunt patency.
After ASD closure, the patients were classified into two groups based on a post-closure PVRI threshold of 3.0 Wood units*m2, which is one criterion for pulmonary arterial hypertension in adults with shunt lesions.13 Pulmonary vasodilation treatment was indicated when the PH remained on echocardiography immediately after closure.
All measurements are expressed as means±the standard deviations, ranges, or medians. The nonparametric Mann-Whitney test was used to compare patients with high post-closure PVRIs to the other patients. The nonparametric Wilcoxon signed rank test and Fisher's exact test were used to quantify the differences after closure. To correlate the post-closure and pre-closure parameters, the nonparametric Spearman correlation coefficient, logistic regression analysis, and the Kruskal-Wallis test were used. p<0.05 was considered statistically significant, and the statistical analyses were performed with SPSS software, version 21.0 (SPSS Inc., Chicago, IL, USA).
The patients' primary data are summarized in Table 1. The median age at cardiac catheterization was 29 years (range, 18.0–62.0). The Qp/Qs was 1.9±0.6 (1.2–3.6). The mPAP was 49.9±11.5 (30.0–77.0), and the PVRI was 9.2±3.6 (1.3–16.7). Pulmonary vasodilator tests were performed in 15 patients. The mPAP and PVRI after the pulmonary vasodilator tests with decreased oxygen were 48.9±8.5 (34.0–66.0) and 5.89±1.99 (2.5–8.6) Wood units*m2, respectively, and both of these changes were significant (p=0.01). The ratios of the mPAP and PVRI decreases after the oxygen tests i.e., the (resting mPAP or PVRI-mPAP or PVRI after oxygen)/(resting mPAP or PVRI) were 6.1±4.9 (-2.2–14.3)% and 39.1±15.9 (8.9–72.2)%, respectively. The decrease in PVRI with oxygen was greater than 20% in all but 2 patients. There were 3 patients with mild PH, 5 patients with moderate PH, and 9 patients with severe PH.
Pulmonary vasodilators were prescribed for 7 patients at least 1 month prior to catheterization. Bosentan was the most common vasodilator (5 patients), followed by sildenafil (two patients). Beraprost was administered to 2 patients exclusively with bosentan (Table 1).
The median age at the time of the operation was 29 years. Fenestrations were made in the surgical patches in 15 patients and in the ASOs in 2 patients. The median fenestration size was 6.5 mm (5–10 mm).
Eleven patients (64.7%) exhibited improved functional class after closure. The median time interval from ASD closure to follow-up was 27 months (range, 4.0–99.0). The CT ratio decreased significantly after ASD closure (p<0.05). Additionally, the mPAP and PVRI decreased significantly after closure in all but 1 patient (p<0.05) (Fig. 1). The fenestrations maintained left-to-right flow patency in 15 of the patients with surgical patches and in 1 patient with an ASO device. Only a single patient with a fenestration in an ASO device exhibited spontaneous closure of the fenestration on follow-up echocardiography. Moreover, the post closure PVRIs exhibited strong linear correlations with the preclosure PVRIs and mPAPs (Spearman's rho coefficients=0.785 and 0.764, respectively, p<0.01). There were significant differences in the post-closure PVRIs between the patients with preclosure PVRIs ≤6, 6<PVRI≤9, and >9 (2.3±0.6 vs. 4.5±1.9 vs. 8.6±3.7 Wood units*m2, respectively; p=0.015) (Fig. 2). The PVRIs after closure with fenestration were over 3.0 Wood units*m2 in 11 patients (64.7%), and their pre-closure PVRI, mPAP with oxygen, and pre-closure Qp/Qs values were significantly different from those of the other patients (6.1±3.0 Wood units*m2 vs. 10.9±2.7 Wood units*m2, 42.8±5.5 mm Hg vs. 52.0±8.2 mm Hg, and 2.3±0.6 vs. 1.7±0.4, respectively) (Fig. 3). However, the age at the time of operation and the pre-closure mPAP were not significantly different (p=0.056 and 0.580, respectively) (Table 3). Logistic regression analysis failed to reveal any pre-closure parameters that predicted a post-closure PVRI >3.0.
Pulmonary vasodilators were prescribed for 13 patients after partial closure. A greater number of patients with post closure PVRIs >3.0 were treated with a pulmonary vasodilator after partial closure, although this difference was not significant (91% vs. 51%, p=0.099). Sildenafil was the most common vasodilator, and bosentan was the next most common (Fig. 4).
This study found that, although ASD closure with fenestration relieves symptoms, right ventricular pressure, and volume overload, 11 patients (64.7%) continued to exhibit a high PVRI value (>3). The pre-closure PVRI, mPAP with oxygen test, and Qp/Qs values of these patients differed significantly from those of the other patients.
Although recent guidelines suggest that Qp/Qs >1.5 and PVRI <5 Wood units*m2 are the upper limits for ASD closure,2 shunt closure in patients with PH remains controversial. PH after shunt closure has been reported to be associated with a worse prognosis than PH with a shunt.1 However, several promising studies of pulmonary vasodilators have led to a shift in treatment. As pulmonary vasodilators may lead to better hemodynamic status, even in patients with congenital heart disease,141516 more aggressive shunt closure can be expected. There are still no significant predictors of the immediate or long-term outcomes of ASD with PH. Postoperative pulmonary hypertensive crises in ASD patients with PH can be lethal. The placement of a small atrial shunt (i.e., a fenestration) could hopefully be a safe option to prevent this situation. This study concluded that ASD closure results in clinical improvement with no deterioration of PH after partial closure. This study indicates that it may be possible to normalize PH with the help of pulmonary vasodilators, although PH might persist and progress. There was no evidence that ASD closure with fenestration could prevent a pulmonary hypertensive crisis; nevertheless, the persistence of PH suggests the need for this procedure in the long term. Among the patients in this study, PH was considered reversible or was concomitant with severe ventricular diastolic dysfunction. The patients also exhibited PH with high PVRIs (>3.0) and Qp/Qs ratios (>1.5).
We performed vasodilator tests with 100% oxygen to evaluate reversibility and observed decreases in the PVRIs greater than 20% in all but 2 patients. The mPAPs decreased significantly after the oxygen test; however, these decreases were much less than 20% and attributed to increased pulmonary blood flow. PVRI is reflected in the evaluation of the reversibility of PH with a shunt.417 Despite inaccuracies in PVRIs that are calculated during oxygen testing, we chose oxygen as a vasodilator due to convenience. The inhaled nitric oxide (iNO) and/or the balloon occlusion tests were applied to a limited number of patients. Barst, et al.17 reported that the combination of iNO and O2 may be more effective than O2 alone in identifying responders. Additionally, the balloon occlusion test has been useful in decisions regarding shunt closure,18 although there are technical difficulties related to total occlusion in large ASDs. The operability of patients with ASD and PH is also controversial. Patient responsiveness to oxygen testing for PH with a shunt may serve as a rationale for ASD closure with fenestration. Based on our observations, the factor that was related to low pulmonary vascular resistance after closure was not the degree of responsiveness but the absolute PAP with oxygen. We used pulmonary vasodilators prior to catheterization in 7 patients; however, regrettably, we did not perform catheterization before the administration of the pulmonary vasodilators. Previously, we initiated vasodilator therapy without catheterization in some situations. Therefore, the effects of the application of pulmonary vasodilators before closure on the hemodynamic data are not clear.
The size of the fenestration depends on the patient's size, although it should be sufficiently large to prevent spontaneous closure but not large enough to cause volume loading. Generally, a 5–10 mm fenestration is acceptable in adult patients. A punch on the patch is useful because the size is accurate and persistent. In the patients in this study, all of the fenestrations were greater than 5 mm. A fenestrated ASO is another good option.919 Fenestrations can be performed with a dilator or another device, and these approaches are easy and popular; however, such fenestrations can also close naturally. The CT ratio on chest X-ray decreased significantly after ASD closure with fenestration; this finding indicates that the right ventricular volume load was alleviated. The follow-up hemodynamic data demonstrated a significant decrease in PAP in all but one patient, which also indicates that the right ventricular pressure overload was alleviated. These changes resulted in symptomatic improvement in our patients. However, 11 patients still had high PVRIs (>3.0 Wood units*m2) despite decreased mean PAPs. We were unable to observe any predictive value of the pre-closure parameters in terms of the occurrence of high postclosure PVRI. Our analysis revealed that pre-closure PVRI, shunt amount, and mPAP with oxygen were significantly different between the two groups. The pre-closure CT ratio and mPAP also exhibited weakly significant differences. However, the patients' ages and the degrees of change after the oxygen tests were not different. Yong, et al.20 reported that in most patients with ASD, PH can be alleviated after ASD closure and that the factors associated with a reduction in mPAP include age, defect size, and baseline mPAP. Moreover, although a lower baseline mPAP was found to be an independent factor associated with normalization, only 48.8% of the patients with moderate or severe PH in the study of Yong, et al. normalized in terms of PAP; this finding is similar to that of the present study. D'Alto, et al.21 observed that the baseline PVRI in patients with PH after shunt closure was 10.1±2.7 Wood units*m2, which was also similar to our results (10.9±2.7 Wood units*m2). These authors also found that a PVRI ≥6 and a PVR/SVR ≥0.33 at baseline were common among patients with PH after shunt closure. There was one patient whose follow-up mPAP and PVRI were higher than the corresponding baseline values (No. 9), but we were unable to identify the risk for this patient. However, this patient was alive and exhibited no changes at the end of the follow-up.
We prefer PVRI to mPAP as an indicator of PH after ASD closure because the fenestrations were maintained in our patients. We observed normalizations of PVRI after ASD closure with fenestration in some patients with pre-closure PVRIs ≥6 Wood units*m2. However, we found that a pre-closure PVRI ≥6 Wood units*m2 carries a high risk of post-closure PH; therefore, fenestration might be a safe option for these patients. Vasodilator therapy was applied after closure. Three (50%) patients with post-closure PVRIs <3.0 Wood units*m2 required vasodilator therapy, whereas one (10%) patient with a post-closure PVRI ≥3 did not require vasodilators. The role of vasodilators in patients with post-closure PVRIs ≥3.0 Wood units*m2 is unclear. Therefore, ASD closure with fenestration might be a reasonable treatment for patients with PH due to the uncertainty and long-term course of post-closure PH.
There are several limitations of this study due to its retrospective nature and small population. We were unable to propose uniform indications for fenestrated closure in PH associated with ASD. We considered the mPAP and PVRI values from the hemodynamic evaluations, but other factors, such as age and ventricular function, were simultaneously considered. Although hemodynamic evaluation is more accurate than echocardiographic evaluation, Fick's principle has its limits regarding pressure and resistance. Oxygen consumption could not be measured precisely, which may have confounded the oxygen test. The resistance ratio (Rp/Rs) might be a more reliable parameter, but this value was only acquired on limited occasions. The time delay between the shunt closure and the hemodynamic evaluation at follow-up was not uniform. Therefore, the time required for complete normalization could not be assessed and differed across cases. We were therefore unsure whether high PVRI values were persistent. We also liberally treated the patients with pulmonary vasodilators that might have influenced the hemodynamic statuses. The evaluation and interpretation of PH in congenital heart disease during treatment with pulmonary vasodilators are unclear. Our follow-up hemodynamic evaluation reflected not only the closure effects but also the medical effects of these vasodilators, and the latter have not been well studied.
In conclusion, although right ventricular pressure and volume overload were alleviated by ASD closure with fenestration in the patients with severe PH, the PVRIs of a significant portion of the patients did not normalize. There were no significant predictors of high post-closure PVRI; therefore, PH should be monitored even after the partial closure of ASDs.
Figures and Tables
Fig. 1
Changes in mPAP (A) and PVRI (B) of each patient. We observed significant decreases from baseline after the oxygen test and after closure. mPAP, mean pulmonary arterial pressure; PVRI, pulmonary vascular resistance index.
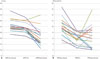
Fig. 2
Differences in post-closure PVRIs for the patients with mild, moderate, and severe pre-closure PH. PVRI, pulmonary vascular resistance index; PH, pulmonary hypertension.

Fig. 3
Significant differences in pre-closure PVRI (A), Qp/Qs (B), and pre-closure mPAP with the oxygen test (C) according to post-closure PVRI (<s3 or ≥3). mPAP, mean pulmonary arterial pressure; PVRI, pulmonary vascular resistance index; Qp/Qs, shunt ratio.

Table 1
The Data for Each Patient
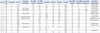
Table 2
Changes Following Atrial Septal Defect Closure

| Pre-closure | Post-closure | p value | |
|---|---|---|---|
| FC I/II/III | 0/14/3 | 9/8/0 | |
| mPAP (mm Hg) | 49.9±11.5 | 32.5±14.4 | 0.001 |
| PVRI (Wood units*m2) | 9.2±3.6 | 6.3±3.8 | 0.004 |
| CT ratio | 0.54±0.06 | 0.48±0.06 | 0.001 |
Table 3
Pre-Closure Patient Parameters According to Post Closure PVRI

References
1. van Loon RL, Roofthooft MT, Hillege HL, ten Harkel AD, van Osch-Gevers M, Delhaas T, et al. Pediatric pulmonary hypertension in the Netherlands: epidemiology and characterization during the period 1991 to 2005. Circulation. 2011; 124:1755–1764.

2. Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N, et al. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010; 31:2915–2957.

3. Beghetti M, Galiè N, Bonnet D. Can "inoperable" congenital heart defects become operable in patients with pulmonary arterial hypertension? Dream or reality? Congenit Heart Dis. 2012; 7:3–11.

4. Lopes AA, O'Leary PW. Measurement, interpretation and use of hemodynamic parameters. Cardiol Young. 2009; 19:Suppl 1. 8–12.

5. Hörer J, Müller S, Schreiber C, Kostolny M, Cleuziou J, Prodan Z, et al. Surgical closure of atrial septal defect in patients older than 30 years: risk factors for late death from arrhythmia or heart failure. Thorac Cardiovasc Surg. 2007; 55:79–83.

6. Steele PM, Fuster V, Cohen M, Ritter DG, McGoon DC. Isolated atrial septal defect with pulmonary vascular obstructive disease--long-term follow-up and prediction of outcome after surgical correction. Circulation. 1987; 76:1037–1042.

7. Beghetti M, Galiè N. Eisenmenger syndrome a clinical perspective in a new therapeutic era of pulmonary arterial hypertension. J Am Coll Cardiol. 2009; 53:733–740.
8. Hirabayashi A, Miyaji K, Akagi T. Continuous epoprostenol therapy and septal defect closure in a patient with severe pulmonary hypertension. Catheter Cardiovasc Interv. 2009; 73:688–691.

9. Althoff TF, Knebel F, Panda A, McArdle J, Gliech V, Franke I, et al. Long-term follow-up of a fenestrated Amplatzer atrial septal occluder in pulmonary arterial hypertension. Chest. 2008; 133:283–285.

10. Bruch L, Winkelmann A, Sonntag S, Scherf F, Rux S, Grad MO, et al. Fenestrated occluders for treatment of ASD in elderly patients with pulmonary hypertension and/or right heart failure. J Interv Cardiol. 2008; 21:44–49.

11. Cho YH, Jun TG, Yang JH, Park PW, Huh J, Kang IS, et al. Surgical strategy in patients with atrial septal defect and severe pulmonary hypertension. Heart Surg Forum. 2012; 15:E111–E115.

12. Kyle WB. Pulmonary hypertension associated with congenital heart disease: a practical review for the pediatric cardiologist. Congenit Heart Dis. 2012; 7:575–583.

13. McLaughlin VV, Archer SL, Badesch DB, Barst RJ, Farber HW, Lindner JR, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents and the American Heart Association developed in collaboration with the American College of Chest Physicians; American Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009; 53:1573–1619.
14. Berger RM, Beghetti M, Galiè N, Gatzoulis MA, Granton J, Lauer A, et al. Atrial septal defects versus ventricular septal defects in BREATHE-5, a placebo-controlled study of pulmonary arterial hypertension related to Eisenmenger's syndrome: a subgroup analysis. Int J Cardiol. 2010; 144:373–378.

15. Dimopoulos K, Inuzuka R, Goletto S, Giannakoulas G, Swan L, Wort SJ, et al. Improved survival among patients with Eisenmenger syndrome receiving advanced therapy for pulmonary arterial hypertension. Circulation. 2010; 121:20–25.

16. Galiè N, Beghetti M, Gatzoulis MA, Granton J, Berger RM, Lauer A, et al. Bosentan therapy in patients with Eisenmenger syndrome: a multicenter, double-blind, randomized, placebo-controlled study. Circulation. 2006; 114:48–54.
17. Barst RJ, Agnoletti G, Fraisse A, Baldassarre J, Wessel DL. NO Diagnostic Study Group. Vasodilator testing with nitric oxide and/or oxygen in pediatric pulmonary hypertension. Pediatr Cardiol. 2010; 31:598–606.

18. Sánchez-Recalde A, Oliver JM, Galeote G, González A, Calvo L, Jiménez-Valero S, et al. Atrial septal defect with severe pulmonary hypertension in elderly patients: usefulness of transient balloon occlusion. Rev Esp Cardiol. 2010; 63:860–864.

19. Dell'avvocata F, Rigatelli G, Cardaioli P, Giordan M. Home-made fenestrated amplatzer occluder for atrial septal defect and pulmonary arterial hypertension. J Geriatr Cardiol. 2011; 8:127–129.
20. Yong G, Khairy P, De Guise P, Dore A, Marcotte F, Mercier LA, et al. Pulmonary arterial hypertension in patients with transcatheter closure of secundum atrial septal defects: a longitudinal study. Circ Cardiovasc Interv. 2009; 2:455–462.

21. D'Alto M, Romeo E, Argiento P, Correra A, Santoro G, Gaio G, et al. Hemodynamics of patients developing pulmonary arterial hypertension after shunt closure. Int J Cardiol. 2013; 168:3797–3801.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download