Abstract
Purpose
Glufosinate poisoning can cause neurologic complications that may be difficult to treat due to delayed manifestation. Studies assessing possible predictors of complications are lacking. Although serum ammonia level is a potential predictor of severe neurotoxicity, it has only been assessed via case reports. Therefore, we investigated factors that predict neurologic complications in acute glufosinate-poisoned patients.
Materials and Methods
We conducted a retrospective review of 45 consecutive glufosinate-poisoning cases that were diagnosed in the emergency department (ED) of Wonju Severance Christian Hospital between May 2007 and July 2014. Patients with a Glasgow Coma Scale (GCS) score of <8, seizure, and/or amnesia were defined to a neurologic complication group.
Results
The neurologic complication group (29 patients, 64.4%) comprised patients with GCS<8 (27 patients, 60.0%), seizure (23 patients, 51.1%), and amnesia (5 patients, 11.1%). Non-neurologic complications included respiratory failure (14 patients, 31.1%), intubation and ventilator care (23 patients, 51.1%), shock (2 patients, 4.4%), pneumonia (16 patients, 35.6%), acute kidney injury (10 patients, 22.2%), and death (4 patients, 8.9%). Complications of GCS<8, seizure, respiratory failure, and intubation and ventilator care appeared during latent periods within 11 hrs, 34 hrs, 14 hrs, and 48 hrs, respectively. Initial serum ammonia was a predictor of neurologic complications [odds ratio 1.039, 95% confidence interval (1.001-1.078), p=0.046 and area under the curve 0.742].
Glufosinate is a phosphorus-containing amino acid, which is an active ingredient in non-selective herbicides,1 and an analog of glutamate that inhibits glutamine synthetase in plants and blocks the synthesis of glutamine from glutamate and ammonia. Intracellular accumulation of ammonia in turn causes tissue necrosis and death of the plant.2
Since 2013, we have noticed an increase in the number patients with glufosinate poisoning admitted to the emergency department (ED) at Wonju Severance Christian Hospital, Wonju College of Medicine, Yonsei University, Wonju, Korea. We suspect that glufosinate is seeing greater use as a non-selective herbicide, because sales of Gramoxone® (paraquat) were banned in South Korea in November 2012 and glufosinate is advertised to have low toxicity to humans and the environment.
Previous reports indicate that glufosinate poisoning can cause severe complications, such as serious disturbances of consciousness, seizures, and amnesia,12345 after latent periods of 4-60 hours.5 Severe complications and the delayed manifestations of severe complications can make it difficult for clinicians to treat glufosinate-poisoned patients. Therefore, predictors of complications would assist clinicians in the treatment of glufosinate-poisoned patients. However, predictors of complications6 remain unknown, and existing reports regarding serum ammonia levels as a probable predictor of severe neurotoxicity are limited to case reports.7 Therefore, we investigated baseline characteristics, clinical presentations, complications, and factors that can be readily assessed in the ED to determine which are predictive of neurologic complications in glufosinate-poisoned patients.
This was a retrospective and observational study of consecutive patients who were diagnosed with acute glufosinate herbicide poisoning between May 2007 and July 2014 at the ED of Wonju Severance Christian Hospital, Wonju College of Medicine, Yonsei University, Wonju, Korea.
Poisoning with glufosinate was confirmed by patient or guardian statements, and verification of the agent was performed by an emergency physician who transcribed the bottle label into patient records.
Data were retrospectively collected from medical records and reviewed. The following parameters were assessed: age, gender, amount of glufosinate ingested, cause of poisoning, time elapsed from ingestion to arrival at the ED, initial symptoms, initial mental status [Glasgow Coma Scale (GCS)], electrocardiogram (ECG), initial vital signs, complications during hospitalization, and mortality. We defined the amount of glufosinate ingested as glufosinate concentration×volume of ingestion, and defined volume of ingestion as "a little" or "a spoonful" (5 mL); "a mouthful" (25 mL); "a small cup" (100 mL); and "a bottle" (300 mL).8 We also evaluated serum ammonia, arterial blood gas, serum lactate, blood urea nitrogen (BUN) and creatinine (CR) in the ED.
The patients were divided into two groups. The neurologic complication group was defined as patients with GCS<8, seizure, and/or amnesia during hospitalization, while the nonneurologic complication group included patients with none of these complications.
We investigated the baseline characteristics of the two groups and the latent periods of complications and predictors of neurologic complications among parameters that are readily assessed in the ED. Total admission days, intensive care unit (ICU) admission days, and mortality were used to compare prognoses between the two groups.
This study was approved by the Institutional Review Board of Wonju College of Medicine, Yonsei University (approval number YWMR-13-5-040).
Statistical analyses were performed using IBM SPSS, version 20 (IBM, Aramark, NY, USA). Nominal data are presented as frequencies and percentages, and continuous variables are presented as mean and standard deviation and median and interquartile range (IQR) after assessments for normality using the Shapiro-Wilk test. The chi-square test or Fisher's exact test were used for comparisons of nominal variables, while the twosample t-test or Mann-Whitney U-test were used to compare continuous variables. Predictors of neurologic complications were determined by logistic regression analysis and optimal cut-off points of predictors were evaluated by receiver operation characteristic (ROC) curves and the Youden index. p-values less than 0.05 were considered statistically significant.
A total of 45 consecutive patients were identified for inclusion in this study. Exclusion criteria were poisoning with any additional material except for alcohol (2 patients; paraquat 1, pyrethroid 1), liver diseases that can cause hyperammonemia (4 patients), and insufficient data (5 patients) (Fig. 1). Between 2007 and 2014, the total number of patients who visited the ED ranged from 28382 and 40465 patients annually.
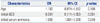
There were 32 men in the sample (71.7%), ranging from 24 to 84 years of age with a mean age of 58±15 years. All patients ingested glufosinate concentrations of 18%, and the median ingested amount of glufosinate was 27.0 (IQR 13.5-54.0) g. A total of 35 patients (77.8%) had ingested glufosinate with suicidal intentions (Table 1).
The most common initial symptoms at the ED included nausea and vomiting (29 patients, 64.4%), and other less common clinical effects included dizziness and odynophagia (Table 1). The median initial GCS was 15 (IQR 12-15), and the average initial serum ammonia was 97.0 (IQR 53.3-130.0) ug/dL (reference range: 19-54 ug/dL) (Table 1).
Complications during hospitalization after glufosinate poisoning included GCS<8 (27 patients, 60.0%), seizure (23 patients, 51.1%), amnesia (5 patients, 11.1%), respiratory failure (14 patients, 31.1%), intubation and ventilator care (23 patients, 51.1%), shock (2 patients, 4.4%), pneumonia (16 patients, 35.6%), and acute kidney injury (AKI) (10 patients, 22.2%), respectively. Average total admission length and ICU admission length were 8 (IQR 3-14) and 2 (IQR 0-7) days, respectively. Four patients (8.9%) died after admission (Table 2). Causes of mortality were respiratory failure (2 patients) and multi-organ failure (2 patients), respectively.
The neurologic complication group included 29 patients (64.4%). Patients in the non-neurologic complication and neurologic complication groups differed in terms of age, initial GCS, and initial serum ammonia, respectively. In daily patterns of serum ammonia between two groups, neurologic complication group had higher serum ammonia levels (Fig. 2). There were no differences in gender, ED arrival time after poisoning, cause of poisoning, ingested amounts, or initial vital signs between the two groups (Table 1). Shock, amnesia, pneumonia, AKI, and mortality did not appear initially, and complications of GCS<8, seizure, respiratory failure, and intubation and ventilator care appeared during latent periods within 11 hrs, 34 hrs, 14 hrs, and 48 hrs, respectively (Table 2).
Median total admission length was 3 (IQR 1-5) days and 12 (IQR 7-15) days in the non-neurologic complication group, compared to the neurologic complication group (p<0.001). Median ICU admission length was 0 (IQR 0-0) days and 6 (IQR 0-9) days in the non-neurologic complication group, compared to the neurologic complication group (p<0.001) (Table 1).
Multiple logistic regression analyses to determine factors related to the development of neurologic complications, including GCS<8, seizure, and amnesia, identified initial serum ammonia (odds ratio, 1.039; 95% confidence interval, 1.001-1.078, p=0.046) as statistically significant. The optimal point of initial serum ammonia was 86 ug/dL (sensitivity: 72%, specificity: 64%, and area under the curve 0.742) according to ROC curves and the Youden index (Table 3).
According to evidence gleaned from previous studies,1910 increases in ammonia levels may affect glufosinate-related neurotoxicity and predict severe complications, such as neurotoxicity, although these previous studies were all case reports.711 Most recently, Mao, et al.7 reported that hyperammonemia may be a potential marker of severe neurotoxicity in patients with glufosinate poisoning; however, because their report was also a case report (3 patients), the statistical power was insufficient.
In the present study, we assessed initial serum ammonia levels for 41 patients (91%) out of 45 patients with acute glufosinate poisoning treated at our ED. In this study, initial serum ammonia levels were higher in the neurologic complication group (p=0.022) (Table 1), and was also a significant predictor of neurologic complications, such as decreased mental capacity, seizure, and amnesia (Table 3). Also, complications were not present at the time of ED arrival in many patients. Severe symptoms, signs, and complications, including decreased mental change, seizure, intubation and ventilator care, can suddenly develop over a latent period in glufosinate poisoning patients (Table 2). Therefore, we propose that clinicians should check initial serum ammonia levels to predict the likelihood of neurologic complications in glufosinate-poisoned patients admitted to the ED. Inoue, et al.6 reported that severe complications following acute glufosinate poisoning were associated with two positive cases of systemic inflammatory response syndrome (SIRS); however, we did not detect any differences between patient groups in terms of the two positive SIRS criteria (Table 1). Further investigations will be needed.
In this study, a total of 64.4% of the patients in our sample were included in the neurologic complication group (GCS<8, seizure, and amnesia). Mao, et al.12 identified a severe/fatal group (respiratory failure, coma, seizure, shock, and death) of 33 patients (28.7%) out of 115 patients with oral exposure. Inoue, et al.6 defined severe complications as follows: respiratory arrest, convulsion, and severe disturbance of consciousness (GCS<8). The total number of patients with severe complications in their study was 8 (50%) out of 16 patients. In our study, the sample was enriched in terms of patients with severe disturbance of consciousness (60.0%) and seizure (51.1%) unlike the samples used in Mao, et al.12 and Inoue, et al.6 (20.9% and 50.0%, 8.7%, and 18.8%), respectively. Between our study, the Mao, et al.12 study, and the Inoue, et al.6 study, there were no significant differences in terms of age and ingested amounts [62±15 yrs vs. 60 (IQR 40-72) yrs vs. 74 (IQR 65-86) yrs; 27.0 (IQR 18.0-54.0) g vs. 30.4 (IQR 18.5-45.6) g vs. 27.8 (IQR 9.3-55.5) g]. The results of this study indicate that acute glufosinate poisoning can cause complications much more often than previously reported. Accordingly, we stress that glufosinate is not safe for human ingestion.
In this study, we found that shock was observed in only 2 patients (4.4%), unlike Mao, et al.12 (11.3%). In our sample, all of 2 patients with shock did not use adrenergic drugs. This may indicate that solvents or surfactants differ in glufosinate products, as Koyama, et al.13 reported that cardiovascular symptoms are caused by surfactants. In the present study, amnesia was observed in 5 patients (11.1%). Nevertheless, because this study was retrospective, records of amnesia may have been insufficient. We hypothesize that the actual prevalence of amnesia in our sample was greater. Therefore, prospective studies may be needed. There was no required hemodialysis in patients with AKI during hospitalization.
Hori, et al.14 reported that severe complications, such as seizure, respiratory failure, and severe disturbance of consciousness, appear after latent periods of 4-60 hours. In the present study, seizures suddenly occurred until 34 hrs after ED arrival and intubation was performed until 48 hrs after ED arrival. Therefore, patients should be monitored carefully for at least for two days after arrival. Records for 18 out of 23 patients with seizures were investigated regarding medication of seizure control. Since seizures in 10 (55.6%) out of 18 patients were not controlled by IV lorazepam, other seizure medications such as phenytoin were used. This may indicate that seizures caused by glufosinate poisoning cannot be easily controlled.
Age differed between the patient groups, with the neurologic complication group being older than the non-neurologic complication group. Mao, et al.12 also found that the severe group [60 (IQR 40-72) years] was older than the non-severe group [42 (IQR 28-54) years]. This result may be explained by the lack of physiologic functional reserve in older patients. Initial GCS scores differed between groups, perhaps because older patients have poor physiologic defense mechanisms against glufosinate poisoning. In addition, they also had longer stays in terms of total and ICU admission than patients in the non-neurologic complication group.
This study had some limitations. First, it was a retrospective study and involved only one hospital. As a result, not all relevant assessment parameters were included. In particular, we did not investigate parameters, such as vomiting before ED arrival and the amount of toxicants ingested, and ED arrival time after ingestion may have been overestimated or underestimated. Second, since the exact percentages of glufosinate, solvent, and surfactant ingested by patients are unknown, their clinical influence could not be predicted. Third, GCS can be affected by co-ingestion of alcohol as well as by glufosinate herbicide. In our study, 48.9% of patients co-ingested alcohol with glufosinate. However, there were no differences in the incidence of alcohol co-ingestion between the two groups (Table 1). In addition, the neurologic complication group included 15 of 23 patients (65.2%) who ingested glufosinate alone. This did not differ from the percentages found among all patients (64.4% in 45 patients). Even when we eliminated the effects of alcohol, patients in the neurologic complication group had lower initial GCS scores than patients in the non-neurologic complication group [13 (IQR 8-15) vs.15 (IQR 15-15), respectively, p=0.006]. Notwithstanding, the lack of evaluation of the presence of alcohol co-ingestion by serum ethanol level in all included patients is a limitation of our study. Further studies are required to clarify these details.
Neurologic complications, such as GCS<8, seizure, and amnesia, developed in 64.4% of patients with acute glufosinate poisoning, and the most common complication was severe disturbance of consciousness (GCS<8). Initial serum ammonia level may be a predictor of neurologic complications.
Figures and Tables
 | Fig. 2Daily serum ammonia levels between the non-neurologic complication and neurologic complication groups. ED, emergency department; HD, hospital day. |
Table 1
Characteristics and Laboratory Findings of Patients with Acute Glufosinate Poisoning

ED, emergency department; SBP, systolic blood pressure; PR, pulse rate; GCS, Glasgow Coma Scale; ECG, electrocardiogram; SIRS, systemic inflammatory response syndrome; BUN, blood urea nitrogen; Cr, creatinine; ICU, intensive care unit.
*Mean±standard deviation, †Median (interquartile range), ‡Initial serum ammonia level was checked in 41 patients out of 45 patients.
Table 2
Features of Complications in Acute Glufosinate Poisoning

References
1. Watanabe T, Sano T. Neurological effects of glufosinate poisoning with a brief review. Hum Exp Toxicol. 1998; 17:35–39.

2. Hoerlein G. Glufosinate (phosphinothricin), a natural amino acid with unexpected herbicidal properties. Rev Environ Contam Toxicol. 1994; 138:73–145.

3. Koyama K, Andou Y, Saruki K, Matsuo H. Delayed and severe toxicities of a herbicide containing glufosinate and a surfactant. Vet Hum Toxicol. 1994; 36:17–18.
4. Ebert E, Leist KH, Mayer D. Summary of safety evaluation toxicity studies of glufosinate ammonium. Food Chem Toxicol. 1990; 28:339–349.

5. Hack R, Ebert E, Ehling G, Leist KH. Glufosinate ammonium--some aspects of its mode of action in mammals. Food Chem Toxicol. 1994; 32:461–470.

6. Inoue Y, Onodera M, Fujita Y, Fujino Y, Kikuchi S, Endo S. Factors associated with severe effects following acute glufosinate poisoning. Clin Toxicol (Phila). 2013; 51:846–849.

7. Mao YC, Wang JD, Hung DZ, Deng JF, Yang CC. Hyperammonemia following glufosinate-containing herbicide poisoning: a potential marker of severe neurotoxicity. Clin Toxicol (Phila). 2011; 49:48–52.

8. Yang PY, Lin JL, Hall AH, Tsao TC, Chern MS. Acute ingestion poisoning with insecticide formulations containing the pyrethroid permethrin, xylene, and surfactant: a review of 48 cases. J Toxicol Clin Toxicol. 2002; 40:107–113.

9. Lluís M, Nogué S, Miró O. Severe acute poisoning due to a glufosinate containing preparation without mitochondrial involvement. Hum Exp Toxicol. 2008; 27:519–524.

10. Bosoi CR, Rose CF. Identifying the direct effects of ammonia on the brain. Metab Brain Dis. 2009; 24:95–102.

11. Ohtake T, Yasuda H, Takahashi H, Goto T, Suzuki K, Yonemura K, et al. Decreased plasma and cerebrospinal fluid glutamine concentrations in a patient with bialaphos poisoning. Hum Exp Toxicol. 2001; 20:429–434.

12. Mao YC, Hung DZ, Wu ML, Tsai WJ, Wang LM, Ger J, et al. Acute human glufosinate-containing herbicide poisoning. Clin Toxicol (Phila). 2012; 50:396–402.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download