This article has been corrected. See "Erratum to "Relationships between Isometric Muscle Strength, Gait Parameters, and Gross Motor Function Measure in Patients with Cerebral Palsy" by Shin HI, et al. (Yonsei Med J 2016;57:217-24.)" in Volume 57 on page 807.
Abstract
Purpose
This study investigated the correlation between isometric muscle strength, gross motor function, and gait parameters in patients with spastic cerebral palsy and to find which muscle groups play an important role for gait pattern in a flexed knee gait.
Materials and Methods
Twenty-four ambulatory patients (mean age, 10.0 years) with spastic cerebral palsy who were scheduled for single event multilevel surgery, including distal hamstring lengthening, were included. Preoperatively, peak isometric muscle strength was measured for the hip flexor, hip extensor, knee flexor, and knee extensor muscle groups using a handheld dynamometer, and three-dimensional (3D) gait analysis and gross motor function measure (GMFM) scoring were also performed. Correlations between peak isometric strength and GMFM, gait kinematics, and gait kinetics were analyzed.
Results
Peak isometric muscle strength of all muscle groups was not related to the GMFM score and the gross motor function classification system level. Peak isometric strength of the hip extensor and knee extensor was significantly correlated with the mean pelvic tilt (r=-0.588, p=0.003 and r=-0.436, p=0.033) and maximum pelvic obliquity (r=-0.450, p=0.031 and r=-0.419, p=0.041). There were significant correlations between peak isometric strength of the knee extensor and peak knee extensor moment in early stance (r=0.467, p=0.021) and in terminal stance (r=0.416, p=0.043).
Conclusion
There is no correlation between muscle strength and gross motor function. However, this study showed that muscle strength, especially of the extensor muscle group of the hip and knee joints, might play a critical role in gait by stabilizing pelvic motion and decreasing energy consumption in a flexed knee gait.
Muscle weakness is a common impairment among patients with cerebral palsy (CP) and is associated with difficulties performing functional activities.12 It is known that the weakness found in CP is attributable to both altered neural mechanisms and muscle tissue changes.3 Lower limb muscle strength is reduced by 6-59% compared with peers of typical development, depending on the muscle group.4
Many clinicians have regarded spasticity as a major factor that contributes to functional limitations and abnormal movement patterns.56 However, recent studies now recognize weakness as a prominent impairment observed in patients with CP.178 Therefore, many researchers have reported a relationship between muscle strength and motor function, and there is increasing interest in measuring muscle strength among patients with CP.24791011 A number of studies have shown that muscle strength is significantly associated with gross motor function and that strength is more highly related to function than spasticity.7 In addition, various studies have reported that muscle-strengthening exercises may result in functional improvements.281213 On the other hand, some studies reported that muscle-strengthening training did not improve functional activity,1415 and other components, such as balance and coordination, may influence the functional ability to a greater degree than muscle strength alone. Therefore, it is questionable whether muscle strength is actually related to motor function.
This study investigated the correlations between isometric muscle strength and gross motor function, gait kinematics, and gait kinetics among ambulatory patients with spastic CP. In addition, we aimed to identify the muscle groups that play an important role in gait pattern in a flexed knee gait.
This study was approved by the Institutional Review Board at our institution (a tertiary referral center for CP). Informed consent was obtained from the patients and relevant guardians. The inclusion criteria were as follows: 1) consecutive ambulatory patients with spastic CP [gross motor function classification system (GMFCS) level I-III], 2) patients with flexed knee gait, who were scheduled for a single event multilevel surgery, including distal hamstring lengthening, 3) patients who had gross motor function measure (GMFM) scores and preoperative three-dimensional (3D) gait analysis, which are the primary and secondary outcome measures, respectively. Patients who had a history of gait correcting surgery and who were unable to accept and follow verbal instructions were excluded. Demographic data, such as gender, age, height, weight, and GMFCS, were obtained from a review of medical records.
Peak isometric muscle strength was measured in all patients using a digital force dynamometer (Compact Force Gauge®, Mecmesin Corporation, West Sussex, UK) with a range of 0-500 N. Test position was standardized for each muscle group in such a way that gravitational forces minimally influenced the assessment.16 Investigated muscle groups were knee extensor, knee flexor, hip extensor, and hip flexor, and these were evaluated bilaterally. Dynamometer was anchored to a rigid frame and was connected to a patient's limb with a strap. Peak isometric strength tests of the hip flexor and hip extensor muscle group were carried out with patients in a prone standing position with the hip and knee in 90° flexion. In this position, the patients' trunk was supported by the examination table and the standing leg, while the other leg was tested (Fig. 1A and B). Peak isometric strength tests of the knee flexor and extensor muscle group were performed with patients positioned in a supported sitting position with the hip and knee in 90° flexion (Fig. 1C and D). Children were given practice trials for each test until the investigator was confident that they understood the task. They were instructed to increase their isometric muscle strength continuously and gradually by pushing or pulling the strap until the maximum strength plateau was reached. After practicing, each child performed three trials with an interval of approximately 30 seconds for each muscle group, and the peak force values from the dynamometer were recorded. During the interval of each trial, we made efforts to relax the patients' muscle due to the presence of spasticity.
All strength tests were conducted, and scores were recorded a day before surgery by a researcher. The researcher was experienced in the measurements used in the study to assure standardization of the procedures and accuracy of the measures. The values for each muscle group were normalized by the individual's body mass (N/kg) for statistical analysis because weight has been shown to be related to force in patients with CP.17
The GMFM is a validated instrument designed to assess motor function in CP. It consists of 88 items within five dimensions: A, lying and rolling; B, sitting; C, crawling and kneeling; D, standing; and E, walking, running, and jumping.18 A percentage score of each dimension and a total percentage score are provided. The authors deemed dimensions D and E as the most relevant to this study in terms of functional abilities. Therefore, the patients included in this study were scored by their physiotherapist using GMFM dimensions D and E a few days before the surgery.
3D Gait analysis was performed a few days before surgery using a motion analysis system (Motion Analysis, Santa Rosa, CA, USA) equipped with seven charge-coupled device cameras and two force plates.19 Markers were placed for the Helen Meyer marker set20 by an experienced operator. Patients were asked to walk three times barefooted on a 9 m walkway. Average kinematic and kinetic data and temporal parameters were archived. Temporal parameters, such as stride length, cadence, and walking speed were normalized according to the patients' height for analysis.
The prior sample size for the reliability testing was calculated to determine the minimum number of patients required. The intraclass correlation coefficients (ICCs) were used for reliability testing at a target value of 0.85 and a 95% confidence interval of 0.2 for three trials. The minimal sample size needed was 20 using Bonett's approximation.21 For the purpose of statistical independence, one limb from patients with diplegia or quadriplegia and the involved limb from patients with hemiplegia were included for statistical analysis.22
Descriptive statistics were used to summarize the patients' demographics. The ICCs and their 95% confidence intervals were used to summarize the intra-session reliability of the peak isometric muscle strength of each muscle group and were calculated in the setting using a two-way random effect model, assuming a single measurement and absolute agreement.23
Differences in peak muscle strength values according to walking ability (GMFCS level) were analyzed using the Kruscal-Wallis test. Correlations between peak isometric strength in each muscle group and GMFM, gait kinematics, and gait kinetics were determined using Spearman correlation coefficients. Statistical analysis was performed using SPSS version 20.0 for Windows (IBM Co., Chicago, IL, USA), and null hypotheses of no difference were rejected if the p values were <0.05.
Thirty-three consecutive patients were initially enrolled. After testing against the exclusion criteria, 24 patients were ultimately included in this study. There were 13 male and 11 female patients. Six patients had hemiplegia and 18 had diplegia. The mean patient age was 10.0±5.2 years (range, 5.3 to 19.6 years). There were 6 with GMFCS level I, 13 with GMFCS level II, and 5 with GMFCS level III. The mean height of the patients was 129.6±19.7 cm and the mean weight was 31.8±15.6 kg (Table 1). All patients underwent distal hamstring lengthening for flexed knee deformity and tendo-Achilles lengthening for equinus foot deformity. Of these, 18 patients (75%) underwent rectus femoris transfer for a stiff knee gait due to quadriceps spasticity.
In term of intra-session reliability of the peak isometric strength measurements, the ICC values were 0.975 (95% confidence interval, 0.951 to 0.988), 0.973 (95% confidence interval, 0.948 to 0.987), 0.986 (95% confidence interval, 0.972 to 0.993), and 0.974 (95% confidence interval, 0.949 to 0.988) for the hip flexor, hip extensor, knee flexor, and knee extensor group, respectively.
There was no correlation between the GMFM score and normalized isometric strength of all muscle groups (Table 2). Peak isometric muscle strength of all muscle groups was not related to the GMFCS level (Table 3).
The mean knee flexion contracture was 1.7±4.6 degrees (range, 0 to 20 degrees) and was significantly related to knee flexion at initial contact (r=0.527, p=0.008). Peak isometric strength of hip extensor and knee extensor was significantly correlated with the mean pelvic tilt (r=-0.588, p=0.003 and r=-0.436, p=0.033) and maximum pelvic obliquity (r=-0.450, p=0.031 and r=-0.419, p=0.041) (Fig. 2). There was a significant correlation between the peak isometric strength of hip extensor and maximum hip flexion in swing (r=-0.542, p=0.008). Peak isometric strength of the knee extensor was related to the knee flexion at initial contact (r=0.477, p=0.018), minimum knee flexion in stance (r=0.527, p=0.008), and knee flexion at terminal swing (r=0.467, p=0.012) (Table 4).
There were significant correlations between peak isometric strength of the knee extensor and peak knee extensor moment in early stance (r=0.467, p=0.021) and in terminal stance (r=0.416, p=0.043). Peak knee absorption power in terminal swing was related to isometric strength of all included muscle groups (r=0.469, 0.481, 0.494, and 0.468) (Table 4).
We investigated the association between maximal isometric muscle strength and gross motor function, gait kinematics, and gait kinetics in patients with spastic CP. Our study showed no correlation between isometric muscle strength and gross motor function. However, we found that higher muscle strength, especially the hip extensor and knee extensor, decreased the pelvic tilt and the pelvic obliquity during walking, and this makes walking more energy-efficient in a flexed knee gait.
There are several limitations with our study. First, the results are valid for patients with GMFCS level I to III spastic CP. These results cannot be generalized to children with lower functional levels or with other clinical sub-types of CP. However, children at GMFCS level IV and V are unable to participate in muscle strength measurements because of muscle weakness and cognitive difficulties. Second, in measuring muscle strength, the other muscle groups that also play an important role in gait and gross motor function, such as the ankle dorsiflexor and ankle plantarflexor,724 were not included. However, all patients in this study had fixed equinus foot deformity; for these patients, it is difficult to objectively measure ankle plantar flexor and dorsiflexor strength using a digital force dynamometer. Therefore, we excluded the ankle plantar flexors and dorsiflexors and focused on the flexor and extensor muscle groups of the hip and knee joints. Third, the isometric strength assessments used do not contain any information about dynamic muscle function, and walking may differ from the isometric test results at fixed joint angles. Isokinetic strength, which involves joint movements rather than isometric muscle strength, may be more related to motor function.17 Fourth, no control was recruited for the comparison of muscle strength for typically developing persons. We hypothesized that the muscle strength of patients with CP is lower than of normally developing persons as demonstrated in previous studies.1425 Fifth, gait performance varies according to the geographical type of CP. This study included patients with hemiplegia and diplegia. However, we believe that muscle strength is more closely related to patients' functional levels than to the geographical type of CP. Therefore, the current study included ambulatory patients (GMFCS I, II, and III) with a homogenous gait pattern consisting of a flexed knee gait. Consequently, we think that investigating the relationship in this cohort is meaningful. Sixth, spasticity might be an important factor in the evaluation of gross motor function and gait pattern. However, recent studies reported that muscle strength may have a greater influence than spasticity on gross motor function and gait pattern. Therefore, we did not evaluate spasticity but instead focused on the muscle strength when investigating gait pattern.
Measuring isometric muscle strength with a dynamometer is an easy method to measure muscle strength in clinical practice. Recently, several authors have shown that it can be measured with sufficient reliability in patients with CP,11252627 including our study, which demonstrated excellent intra-session reliability with ICC values ranging from 0.973 to 0.984.
Previous studies have investigated the relationship between muscle strength and gross motor function in patients with CP (Table 5). They reported a significant correlation between muscle strength and the GMFM, indicating that muscle strength/weakness affects walking ability.24791011 They have also found a statistically significant difference in muscle strength between the GMFCS levels.428 Of these studies, Damiano and Abel2 used absolute strength values without normalization and the mean values of both extremities for the analysis. They found that the mean strength had significant correlation with total GMFM. Ross and Engsberg7 measured the isokinetic muscle strength, which may be related more to Dimensions D and E of GMFM than the isometric muscle strength. They found that aggregate strength was highly related to the total GMFM. Goh, et al.10 recruited the school-aged (range, 7 to 12 years) children with spastic diplegia, and reported that the strength of quadriceps and hamstring had significant relationships with total GMFM. However, our present study did not show a correlation between GMFM score and isometric muscle strength of the included muscle groups. In addition, there was no difference in the peak isometric muscle strength based on the patients' GMFCS levels. We believe that if the muscle strength of patients exceeds a certain level, it may not provide any additional advantage in their functional abilities. In addition, other components such as balance and coordination may influence functional ability to a greater degree than muscle strength alone.
Muscle strength has previously been found to correlate with kinematic gait variables, walking velocity, and stride length.2729 In this study, there was no correlation between isometric muscle strength and normalized temporal parameters, such as stride length, cadence, and walking speed, contrary to the results of other studies. A significant correlation was found between strength of the hip extensor and the pelvic mean anterior tilt (r=-0.14),29 and between aggregate strength and the pelvic tilt (r=-0.50).7 Our present study revealed a significant correlation between peak isometric strength of the hip extensor and knee extensor, and the pelvic tilt and pelvic obliquity. These results infer that the extensor muscles of the hip and knee joint might play a critical role in gait by stabilizing the pelvic motion during walking.
There have been several reports investigating the relationships between muscle strength and kinetic gait parameters.242930 Eek, et al.24 reported that there was a significant correlation between muscle strength in almost all muscle groups and plantarflexing gait moments and ankle generating power in children with CP, and that ankle plantarflexors were important muscles with weakness that affects the kinetic gait pattern. Desloovere, et al.29 showed weak correlations between lower limb strength and joint kinetics in children with CP. Dallmeijer, et al.30 found a significant difference between isometric hip flexor strength and the peak hip flexor moment during gait in patients with diplegic CP. No significant relationships between the isometric strength of the other lower limb muscle groups and corresponding peak moment during gait were found. In this study, the knee extensor moments in the early and terminal stances were significantly related to the isometric strength of the knee extensor. This study included only patients with a flexed knee gait. The flexed knee locates the ground reaction force posterior to the knee joint. If the extensor muscle of the hip or knee does not produce sufficient extension moments, the flexed knees become further flexed and the energy consumption is increased. Our findings demonstrated that greater strength of the knee extensor muscle produces sufficient knee extensor moments in the stance and might decrease energy consumption during walking. There is a significant correlation between isometric muscle strength in all of the measured muscle groups and the peak knee absorption power in the terminal swing. The power curves of the joint kinetics estimate the work performed at the joint during a single gait cycle.31 Therefore, these results indicate that the greater the muscle strength, the less eccentric work is performed, and that greater muscle strength makes walking more energy efficient.
In conclusion, there is no evidence of a correlation between muscle strength and gross motor function. However, this study showed that muscle strength, especially of the extensor muscle group of the hip and knee joints, might play a critical role in gait by stabilizing pelvic motion and decreasing energy consumption in a flexed knee gait. Further studies regarding changes in the muscle strength after a single event multilevel surgery and their relationships with gait kinematics and kinetics are needed.
Figures and Tables
Fig. 1
Measurement of peak isometric strength for the hip flexor (A), hip extensor (B), knee flexor (C), and knee extensor (D) muscle group. (A and B) The leg to be measured is flexed at 90° at the hip and knee joint. The patient may hold the examination table and presses toward the ground with the other leg as depicted. The dynamometer is fixed to a rigid frame. The patient presses the knee slowly forward (A) or backward (B) against the band and the pelvis stays rigid. (C and D) Knee joint to be measured is flexed at 90° and hands are relaxed or folded. The band is placed on the lower leg, with its distal border as close as possible to the ankle joint and the dynamometer is fixed to a rigid frame. The patient presses the lower legs slowly backward (C) or forward (D) against the band. The trunk remains upright and no weight shifting is allowed.

Table 1
Demographics, GMFM, and Peak Isometric Strength of Patients

Table 2
Correlations between Peak Isometric Muscle Strength and GMFM
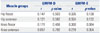
| Muscle groups | GMFM-D | GMFM-E | ||
|---|---|---|---|---|
| r | p value | r | p value | |
| Hip flexor | 0.147 | 0.503 | 0.326 | 0.130 |
| Hip extensor | 0.121 | 0.582 | 0.324 | 0.132 |
| Knee flexor | 0.178 | 0.406 | 0.360 | 0.084 |
| Knee extensor | 0.057 | 0.792 | 0.219 | 0.304 |
Table 3
Peak Isometric Muscle Strength According to GMFCS Levels

Table 4
Correlations between Peak Isometric Muscle Strength and Gait Kinetics
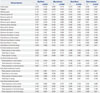
Table 5
Previous Studies on Correlation between Muscle Strength and Gross Motor Function

| Study | No. of subjects | Muscle group | GMFM total | GMFM-D | GMFM-E | |||
|---|---|---|---|---|---|---|---|---|
| r | p value | r | p value | r | p value | |||
| Damiano and Abel2 | 11 | - | 0.59 | 0.05 | - | - | - | - |
| Eek and Beckung4 | 55 | Hip extensor | 0.59 | <0.01 | 0.43 | <0.01 | 0.54 | <0.01 |
| Hip flexor | 0.73 | 0.59 | 0.61 | |||||
| Hip abductor | 0.71 | 0.61 | 0.66 | |||||
| Hip adductor | 0.64 | 0.56 | 0.63 | |||||
| Knee extensor | 0.52 | 0.48 | 0.53 | |||||
| Knee flexor | 0.76 | 0.69 | 0.77 | |||||
| Ankle dorsiflexor | 0.68 | 0.68 | 0.67 | |||||
| Ankle plantarflexor | 0.80 | 0.72 | 0.76 | |||||
| Damiano, et al.9 | 10 | Knee extensor | 0.57 | <0.05 | - | - | - | - |
| Goh, et al.10 | 27 | Knee extensor | 0.78 | <0.01 | 0.75 | <0.01 | 0.77 | <0.01 |
| Knee flexor | 0.84 | 0.82 | 0.81 | |||||
| Ross and Engsberg7 | 97 | - | 0.83 | <0.01 | 0.81 | <0.01 | - | - |
| Berry, et al.11 | 15 | Hip abductor | - | - | 0.64 | 0.014 | 0.64 | 0.014 |
| Knee extensor | 0.38 | 0.16 | 0.38 | 0.16 | ||||
| Knee flexor | 0.48 | 0.08 | 0.60 | 0.023 | ||||
References
1. Wiley ME, Damiano DL. Lower-extremity strength profiles in spastic cerebral palsy. Dev Med Child Neurol. 1998; 40:100–107.

2. Damiano DL, Abel MF. Functional outcomes of strength training in spastic cerebral palsy. Arch Phys Med Rehabil. 1998; 79:119–125.

3. Mockford M, Caulton JM. The pathophysiological basis of weakness in children with cerebral palsy. Pediatr Phys Ther. 2010; 22:222–233.

4. Eek MN, Beckung E. Walking ability is related to muscle strength in children with cerebral palsy. Gait Posture. 2008; 28:366–371.

5. Fasano VA, Broggi G, Barolat-Romana G, Sguazzi A. Surgical treatment of spasticity in cerebral palsy. Childs Brain. 1978; 4:289–305.

6. Bobath K. Neurophysiological basis for the treatment of cerebral palsy. 2nd ed. London: William Heimenamm Medical Books Ltd;1980.
7. Ross SA, Engsberg JR. Relationships between spasticity, strength, gait, and the GMFM-66 in persons with spastic diplegia cerebral palsy. Arch Phys Med Rehabil. 2007; 88:1114–1120.

8. Eek MN, Tranberg R, Zügner R, Alkema K, Beckung E. Muscle strength training to improve gait function in children with cerebral palsy. Dev Med Child Neurol. 2008; 50:759–764.

9. Damiano DL, Martellotta TL, Sullivan DJ, Granata KP, Abel MF. Muscle force production and functional performance in spastic cerebral palsy: relationship of cocontraction. Arch Phys Med Rehabil. 2000; 81:895–900.

10. Goh HT, Thompson M, Huang WB, Schafer S. Relationships among measures of knee musculoskeletal impairments, gross motor function, and walking efficiency in children with cerebral palsy. Pediatr Phys Ther. 2006; 18:253–261.

11. Berry ET, Giuliani CA, Damiano DL. Intrasession and intersession reliability of handheld dynamometry in children with cerebral palsy. Pediatr Phys Ther. 2004; 16:191–198.

12. Engsberg JR, Ross SA, Collins DR. Increasing ankle strength to improve gait and function in children with cerebral palsy: a pilot study. Pediatr Phys Ther. 2006; 18:266–275.

13. Lee JH, Sung IY, Yoo JY. Therapeutic effects of strengthening exercise on gait function of cerebral palsy. Disabil Rehabil. 2008; 30:1439–1444.

14. Scholtes VA, Dallmeijer AJ, Rameckers EA, Verschuren O, Tempelaars E, Hensen M, et al. Lower limb strength training in children with cerebral palsy--a randomized controlled trial protocol for functional strength training based on progressive resistance exercise principles. BMC Pediatr. 2008; 8:41.
15. Scianni A, Butler JM, Ada L, Teixeira-Salmela LF. Muscle strengthening is not effective in children and adolescents with cerebral palsy: a systematic review. Aust J Physiother. 2009; 55:81–87.

16. Stoll T, Huber E, Seifert B, Stucki G, Michel BA. Isometric muscle strength measurement. New York: Thieme Stuttgart;2002.
17. MacPhail HE, Kramer JF. Effect of isokinetic strength-training on functional ability and walking efficiency in adolescents with cerebral palsy. Dev Med Child Neurol. 1995; 37:763–775.

18. Russell DJ, Rosenbaum PL, Cadman DT, Gowland C, Hardy S, Jarvis S. The gross motor function measure: a means to evaluate the effects of physical therapy. Dev Med Child Neurol. 1989; 31:341–352.

19. Chesnin KJ, Selby-Silverstein L, Besser MP. Comparison of an inshoe pressure measurement device to a force plate: concurrent validity of center of pressure measurements. Gait Posture. 2000; 12:128–133.

20. Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990; 8:383–392.

21. Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002; 21:1331–1335.

22. Park MS, Kim SJ, Chung CY, Choi IH, Lee SH, Lee KM. Statistical consideration for bilateral cases in orthopaedic research. J Bone Joint Surg Am. 2010; 92:1732–1737.

23. Lee KM, Lee J, Chung CY, Ahn S, Sung KH, Kim TW, et al. Pitfalls and important issues in testing reliability using intraclass correlation coefficients in orthopaedic research. Clin Orthop Surg. 2012; 4:149–155.

24. Eek MN, Tranberg R, Beckung E. Muscle strength and kinetic gait pattern in children with bilateral spastic CP. Gait Posture. 2011; 33:333–337.

25. van der Linden ML, Aitchison AM, Hazlewood ME, Hillman SJ, Robb JE. Test-retest repeatability of gluteus maximus strength testing using a fixed digital dynamometer in children with cerebral palsy. Arch Phys Med Rehabil. 2004; 85:2058–2063.

26. Crompton J, Galea MP, Phillips B. Hand-held dynamometry for muscle strength measurement in children with cerebral palsy. Dev Med Child Neurol. 2007; 49:106–111.

27. Taylor NF, Dodd KJ, Graham HK. Test-retest reliability of handheld dynamometric strength testing in young people with cerebral palsy. Arch Phys Med Rehabil. 2004; 85:77–80.

28. Thompson N, Stebbins J, Seniorou M, Newham D. Muscle strength and walking ability in diplegic cerebral palsy: implications for assessment and management. Gait Posture. 2011; 33:321–325.

29. Desloovere K, Molenaers G, Feys H, Huenaerts C, Callewaert B, Van de Walle P. Do dynamic and static clinical measurements correlate with gait analysis parameters in children with cerebral palsy. Gait Posture. 2006; 24:302–313.

30. Dallmeijer AJ, Baker R, Dodd KJ, Taylor NF. Association between isometric muscle strength and gait joint kinetics in adolescents and young adults with cerebral palsy. Gait Posture. 2011; 33:326–332.

31. Gage JR. The clinical use of kinetics for evaluation of pathologic gait in cerebral palsy. Instr Course Lect. 1995; 44:507–515.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download