Abstract
Refinement of surgical techniques has allowed hearing preservation after tumor resection to be prioritized. Moreover, restoration of hearing after tumor removal can be attempted in patients with bilateral vestibular schwannomas or those with a schwannoma in the only-hearing ear. Cochlear implantation (CI) has emerged as a proper method of acoustic rehabilitation, provided that the cochlear nerve remains intact. Studies of electrical promontory stimulation in patients after vestibular schwannoma resection have demonstrated favorable results. We describe herein two cases of hearing rehabilitation via CI implemented at the time of vestibular schwannoma resection. Tumors were totally removed, and cochlear implant electrodes were successfully inserted in both cases. Also, post operative CI-aided hearing showed improved results.
The treatment options for small to medium sized vestibular schwannomas include observation, radiotherapy, and surgery.1 Recent refinement of surgical techniques has made it possible to prioritize hearing preservation after tumor resection.2 Moreover, hearing after tumor removal can be restored in patients with bilateral vestibular schwannomas or those with a schwannoma in the only-hearing ear.3
The standard treatment for unilateral hearing loss after unilateral vestibular schwannoma resection has been bone conducting or bone anchoring hearing aids (BCHA or BAHA), though cochlear implantation (CI) has emerged as an alternative method of acoustic rehabilitation, provided that the cochlear nerve remains intact.4 Studies of electrical promontory stimulation in patients after vestibular schwannoma resection have demonstrated favorable results.56
Since the indications for CI have recently expanded, CI has been suggested by many as an appropriate adjunctive treatment to vestibular schwannoma resection.789 Patients with bilateral vestibular schwannomas or with a schwannoma in the only-hearing ear are candidates for CI. In addition, patients with good hearing in the contralateral side are also candidates for the quality of life. Early cochlear degeneration can limit hearing rehabilitation via CI, particularly if there is significant delay after schwannoma resection, despite of sparing the cochlear nerve.4
We describe herein two cases of hearing rehabilitation via CI implemented at the time of vestibular schwannoma resection.
A 72-year-old woman presented with moderate to severe bilateral hearing impairment. She had used conventional hearing aids in the left ear for eight years, but presented for evaluation of deteriorating hearing secondary to worsening otorrhea. Otoscopic examination revealed a small perforation and discharge at the left tympanic membrane. A pure tone audiogram revealed right sensorineural and left mixed hearing loss (Fig. 1A). Speech discrimination scores were 72% in the right ear at the most comfortable listening (MCL) level, and immeasurable in the left ear. Temporal magnetic resonance imaging (MRI) scan was thus obtained, revealing an 8 mm intracanalicular schwannoma on the left (Fig. 1C and D).
Due to the patient's age and small tumor size, our initial management was conservative, consisting of observation and infection control. However, as the patient desired improvement of hearing in her left ear, we opted for tumor resection with simultaneous CI. Six months pre-operatively, we performed a tympanomastoidectomy on the left ear, which resulted in controlled infection and a well-tympanized eardrum. The bone conduction of the left ear was reserved, and the air-bone gap of left ear was reduced. Subsequently, we resected the tumor via a translabyrinthine approach with concurrent CI (SONATATI100, MedEL, Innsbruck, Austria) via facial recess approach (Fig. 1E and F). We were able to preserve the cochlear nerve, as well as achieve total tumor resection.
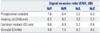
Two years post-operatively, pure tone audiometry demonstrated a threshold of 38.8 dB in the CI augmented left ear and 30.0 dB in the hearing aid augmented right ear (Fig. 1B). The results of the Korean Hearing in Noise test (K-HINT), which measures the binaural hearing performance in a noisy environment, are described in Table 1. A 1 dB decrease in the signal to noise ratio (SNR) corresponds to a 9% improvement in binaural hearing.1011 On average, patients who received CI showed a 19.8% improvement in binaural hearing under front noise; in bimodal mode, a 36% improvement was shown under front noise, and 27% improvement under composite noise.
A 58-year-old man who had undergone canal wall down tympanomastoidectomy in his right ear presented with bilateral hearing impairment. He complained of chronic hearing loss in the right ear, as well as abrupt hearing loss in the left. A pure tone audiogram revealed bilateral mixed hearing loss with an average air conduction threshold of 43 dB in the right ear and 72 dB in the left (Fig. 2A). Speech discrimination scores were 92% in the right ear at 86 dB MCL and 88% in the left ear at 102 dB MCL. A year later, a follow-up pure tone audiogram showed complete hearing loss (scale out) in the left ear, along with an unmeasurable speech discrimination score. A left internal auditory canal intracanalicular mass lesion was noted on the preoperative brain MRI scan, with diameter of 6 mm and width of 13 mm (Fig. 2C and D).
We proposed two surgical approaches: mass excision via translabyrinthine approach, followed by either BAHA or CI. This patient and his family opted for the latter option. We conducted canal wall down mastoidectomy, subtotal petrosectomy and EAC closure for infection control, and the tumor was totally resected via translabyrinthine approach, with successful electrode insertion via round window approach (CONCERTO08363, MedEL, Austria) (Fig. 2E-H). At three month follow-up, CI-aided pure tone audiogram revealed an average sound field threshold of 48.8 dB in the left ear (Fig. 2B). Notably, his tinnitus was also markedly reduced.
In considering surgical resection of small or medium sized vestibular schwannomas, priority should be given to the preservation or restoration of hearing. BCHA or BAHA have been standard treatments for post-surgical unilateral hearing impairment, but are limited in their capacity to improve hearing in the affected ear. Reports from several centers on CI and labyrinthectomy or vestibular schwannoma resection show a favorable prognosis for concurrent or post-operative CI.79121314 In fact, the prognosis was similar to that of unilaterally deaf patients treated with CI.
Candidacy criteria for CI with tumor resection include total tumor removal, preservation of the cochlear nerve anatomy and function, and surgeon experience. Anatomical preservation of cochlear nerve cannot assure its functional preservation, therefore, intraoperative monitoring can be useful. However, in the present case, we couldn't monitor for several reasons.
MRI can be used post-operatively to evaluate remnant tumor tissue prior to CI implementation, if performed years after resection. In such cases, however, cochlear ossification and cochlear nerve atrophy can present complications. In our cases, complete tumor resection was not necessary for MRI evaluation, therefore, an enhanced CT was used instead for follow-up.
Arriaga and Marks10 were the first to report on concurrent CI and schwannoma resection with favorable outcomes. Successful hearing restoration with CI depends on survival of the spiral ganglion nerve fibers, as well as the patency of the cochlea. The rapid and significant improvement in speech recognition with CI suggests that, despite the presence of tumor in the cochlear nerve and potential intra-operative injuries, the number of surviving spiral ganglion axons is sufficient for CI rehabilitation. There are thus far no reports comparing outcomes between concurrent and staged procedures. Nevertheless, since calcification of inner ear structures can occur as a post-operative complication, earlier implementation of CI operation should be sought for hearing restoration and improvement of quality of life.
Figures and Tables
Fig. 1
(A) Preoperative pure tone audiogram revealed moderate sensorineural hearing loss on the right and severe mixed hearing loss on the left. (B) Postoperative aided hearing threshold. Right ear was aided by hearing aid, and left ear was aided by CI. (C) The right side was aided by hearing aid and the left side by cochlear implant. Low signal on T2 and high signal enhanced T1 (D) indicate that the tumor (arrow) is a schwannoma. (E) The tumor (arrow) was totally removed via a translabyrinthine approach. The cochlear nerve was anatomically preserved during the operation. (F) Cochlear implantation was performed simultaneously. The internal device electrode was inserted through a posterior tympanotomy site (arrow). To prevent cerebrospinal fluid leakage, the tympanotomy site was plugged with a small piece of temporalis muscle after implantation.

Fig. 2
(A) Preoperative pure tone audiogram revealed bilateral sensorineural hearing loss. The right side showed moderate and the left side showed profound hearing loss. (B) Postoperative bimodal aided hearing threshold. Right side was aided by hearing aid and left side was aided by CI. (C) Low signal on T2 image and high signal on gadolinium-enhanced T1 (D) indicate that the tumor (arrow) has a high possibility of schwannoma. (E) The tumor (T) was separated and dissected from CN VIII (white arrow). (F) After tumor removal via a translabyrinthine approach, a well-preserved cochleo-vestibular nerve (arrow) and intact facial nerve (white arrowhead) were noted. (G) After repair of the dura with abdominal fat, the round window of the cochlea (arrowhead) was identified. (H) Cochlear implantation was performed simultaneously. The internal device electrode (arrow) was inserted through the round window.

References
1. Lustig LR, Yeagle J, Niparko JK, Minor LB. Cochlear implantation in patients with bilateral Ménière's syndrome. Otol Neurotol. 2003; 24:397–403.

2. Cohen NL, Lewis WS, Ransohoff J. Hearing preservation in cerebellopontine angle tumor surgery: the NYU experience 1974-1991. Am J Otol. 1993; 14:423–433.

3. Arístegui M, Denia A. Simultaneous cochlear implantation and translabyrinthine removal of vestibular schwannoma in an only hearing ear: report of two cases (neurofibromatosis type 2 and unilateral vestibular schwannoma). Otol Neurotol. 2005; 26:205–210.

4. Zanetti D, Campovecchi CB, Pasini S, Nassif N. Simultaneous translabyrinthine removal of acoustic neuroma and cochlear implantation. Auris Nasus Larynx. 2008; 35:562–568.

5. Lambert PR, Ruth RA, Halpin CF. Promontory electrical stimulation in labyrinthectomized ears. Arch Otolaryngol Head Neck Surg. 1990; 116:197–201.

6. Kartush JM, Linstrom CJ, Graham MD, Kulick KC, Bouchard KR. Promontory stimulation following labyrinthectomy: implications for cochlear implantation. Laryngoscope. 1990; 100:5–9.
7. Hoffman RA, Kohan D, Cohen NL. Cochlear implants in the management of bilateral acoustic neuromas. Am J Otol. 1992; 13:525–528.
8. Shin YJ, Fraysse B, Sterkers O, Bouccara D, Rey A, Lazorthes Y. Hearing restoration in posterior fossa tumors. Am J Otol. 1998; 19:649–653.
9. Tono T, Ushisako Y, Morimitsu T. Cochlear implantation in an intralabyrinthine acoustic neuroma patient after resection of an intracanalicular tumor. Adv Otorhinolaryngol. 1997; 52:155–157.

10. Lim HW, Hong SM, Choi SW, Jung JW, Shin J, Chae SW. Availability of Korean hearing in noise test (KHINT) in children. Korean J Otorhinolaryngol-Head Neck Surg. 2011; 54:462–466.

11. Moon SK, Mun HA, Jung HK, Soli SD, Lee JH, Park K. Development of sentences for Korean hearing in noise test (KHINT). Korean J Otolaryngol-Head Neck Surg. 2005; 48:724–728.
12. Arriaga MA, Marks S. Simultaneous cochlear implantation and acoustic neuroma resection: imaging considerations, technique, and functional outcome. Otolaryngol Head Neck Surg. 1995; 112:325–328.

13. Kveton JF, Abbott C, April M, Drumheller G, Cohen N, Poe DS. Cochlear implantation after transmastoid labyrinthectomy. Laryngoscope. 1989; 99(6 Pt 1):610–613.

14. Zwolan TA, Shepard NT, Niparko JK. Labyrinthectomy with cochlear implantation. Am J Otol. 1993; 14:220–223.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download