Abstract
Purpose
The -1237T/C polymorphism of the Toll-like receptor 9 (TLR9) gene has been implicated in the susceptibility of inflammatory bowel diseases (IBDs), but the results remain conflicting. We further investigated this association via meta-analysis.
Materials and Methods
Multiple electronic databases were extensively searched until February, 2015. The strength of association was evaluated by calculating the pooled odds ratios (ORs) and 95% confidence intervals (CIs).
Results
A total of 2987 cases and 2388 controls from eight studies were analyzed. Overall, association was found between TLR9 -1237T/C polymorphism and the risk of IBDs when all the studies were pooled (recessive model, OR: 1.59, 95% CI: 1.02-2.47, p=0.04; homozygote comparison, OR: 1.62, 95% CI: 1.04-2.52, p=0.03; allele model, OR: 1.13, 95% CI: 1.00-1.27, p=0.05). Stratification by ethnicity indicated an association between TLR9 -1237T/C polymorphism and IBDs risk in Caucasians (recessive model, OR: 1.59, 95% CI: 1.02-2.47, p=0.04; homozygote comparison, OR: 1.62, 95% CI: 1.04-2.52, p=0.03; allele model, OR: 1.12, 95% CI: 1.00-1.27, p=0.05). When stratified by disease type, significant correlation were only found in the Crohn's disease subgroup (recessive model, OR: 1.69, 95% CI: 1.05-2.73, p=0.03; homozygote model, OR: 1.74, 95% CI: 1.07-2.82, p=0.02; allele model, OR: 1.15, 95% CI: 1.01-1.32, p=0.04).
Inflammatory bowel diseases (IBDs), which include Crohn's disease (CD) and ulcerative colitis (UC), are idiopathic and chronic inflammatory disorders of the gastrointestinal tract.1 UC is characterized by inflammation that is limited to the mucosal and sub-mucosal layers of the colon and rectum. Conversely, in CD, the inflammation may involve any part of the gastrointestinal tract in a non-continuous fashion.2 The incidence of IBD is increasing around the world, and its influence on morbidity and mortality are quite significant.3 To date, the definite etiology of IBDs remains elusive. Nevertheless, growing evidence has indicated that IBDs result from a complicated inflammatory response in which environmental and genetic factors may play important roles.45
Toll-like receptors (TLRs) represent a group of pattern recognition receptors (PRRs) that can be activated through the recognition of pathogen-associated molecular patterns (PAMPs).6 There are ten different TLRs that have been identified in humans, and TLR9 is one of them. TLR9 is characterized by recognizing unmethylated CpG DNA and acting as an effective sensor for bacterial infection.7 Different from other TLRs, the PAMP recognition of TLR9 mainly takes place on the surface of the endosomal compartment. When CpG-DNA binds to TLR9, MyD88 is recruited, leading to phosphorylation of IRAK and TRAF6, at which point the transcription factor NF-κB is finally activated.8 The gene encoding TLR9 is located on the chromosome 3p21.3, which is in the vicinity of one susceptible region for IBDs.9 Numerous single nucleotide polymorphisms (SNPs) have been identified for the TLR9 gene, and the -1237T/C polymorphism (rs5743836) is the most significant.101112 It has been proven that the rs5743836 T/C polymorphism can lead to a T-to-C exchange in the promoter region of TLR9 at position -1237, which can create a potential binding site for NF-κB.13
A number of recent case-control studies have been carried out to evaluate the association between TLR9-1237T/C polymorphism and the susceptibility of IBDs.1415161718192021 However, the results are controversial. A meta-analysis is a powerful method to deal with these ambiguities and can enhance the statistical power of genetic association studies.22 Thus, we performed this meta-analysis to determine the exact relationship between TLR9-1237T/C polymorphism and the risk of IBDs.
A comprehensive search was conducted for this meta-analysis on the association between TLR9-1237T/C polymorphism and IBDs without language restrictions. Relevant publications were selected using the following electronic databases: PubMed, Web of Knowledge, and the Chinese National Knowledge Infrastructure (CNKI), with the most recent report dated February, 2015. The following terms were used as search keywords: ("TLR9" or "Toll-like receptor 9"), ("polymorphism," "variant," or "SNP"), and ("inflammatory bowel disease," "Crohn's disease," "ulcerative colitis," "IBD," "CD," or "UC"). The reference list of all retrieved literature was carefully scanned to identify the relevant publications.
Studies were included in this meta-analysis if they met all of the following criteria: 1) evaluation of the association between TLR9-1237T/C polymorphism and the risk of IBDs; 2) a case-control design; 3) genotype distribution availability in cases and controls; and 4) consistency of the genotype distributions in the controls with Hardy-Weinberg equilibrium (HWE). Studies were excluded if they met any one of the following criteria: 1) genotype or allele frequencies could not be obtained; 2) duplicated data were used; or 3) data were only presented in reviews, case-reports, or abstracts.
Two authors (Jian Shang & Xiaobing Wang) of this article independently extracted the data from the eligible literature. Discrepancies between the reviewers were solved by discussion or a third author. The following extracted data were included: first author's name, publication year, region, ethnicity, source of control, genotyping method, number of cases and controls, and p-value for HWE. Furthermore, corresponding authors were contacted if the genotype or allele frequencies were not immediately available.
The quality of each study was independently assessed by two
authors (Jian Shang & Liping Chen) of our study. The quality
scoring criteria in this meta-analysis was modified from previous
publications (Supplementary Table 1, only online).2324 Total
quality scores ranged from 0 points (worst) to 14 points (best).
RevMan 5.2 (Cochrane Collaboration, Copenhagen, Denmark) and STATA 12.0 (Stata Corp., College Station, TA, USA) were used to conduct this meta-analysis. The strength of the association between TLR9-1237T/C polymorphism and the risk of IBDs was estimated using pooled odds ratios (ORs) and 95% confidence intervals (CIs). Five different genetic models were performed in our study: a dominant model (TC+CC vs. TT), a recessive model (CC vs. TC+TT), heterozygote comparison (TC vs. TT), homozygote comparison (CC vs. TT), and an allele model (C vs. T). Heterogeneity was estimated using Cochran's Q statistic and I2 statistic; I2 values of 25%, 50%, and 75% were defined as low, moderate, and high heterogeneity, respectively.25 If the p-value of the Q-test was >0.05 or the I2 value was ≤50%, the pooled ORs of each study were calculated using a fixed-effective model. Otherwise, a random-effective model was used.26 Publication bias was calculated using a funnel plot and Egger's test.27 A χ2 test was performed to assess whether the genotype distributions in the control groups conformed to HWE. In addition, subgroup analyses stratified by ethnicity and disease phenotype were also conducted in our study.
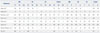
A detailed flow diagram of literature retrieval is shown in Fig. 1. After an initial comprehensive search from the selected databases, 485 articles were initially identified in our study. Among these, 266 were found to contain duplicated data. After screening the remaining 219 papers by reading the titles and abstracts, 12 studies were assessed in more detail. After reading the full texts of these studies, we excluded one paper with incomplete data and three papers with incorrect polymorphism. Ultimately, a total of eight studies assessing the association between TLR9-1237T/C polymorphism and the risk of IBDs were available in the current meta-analysis. Among these, six were performed in Caucasian populations, and two were in Asian populations. Numerous genotyping methods were used in these studies, including single-direction-sequencing (SDS), TaqMan, polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP), and matrix-assisted laser desorption/ionization time of flight (MALDI-TOF). Genotype distributions were all in accordance with HWE (Table 1). The precise characteristics of the selected literature are shown in Table 1, and the genotype and allele distributions of cases and controls are summarized in Table 2.
A summary of the meta-analysis of the relationship between TLR9-1237T/C polymorphism and the risk of IBDs is shown in Table 3. Overall, significant association was found between TLR9-1237T/C polymorphism and IBDs using recessive (OR: 1.59; 95% CI: 1.02-2.47; p=0.04) (Fig. 2) and homozygote (OR: 1.62; 95% CI: 1.04-2.52; p=0.03) (Fig. 2) genetic models. Additionally, we also found a borderline-significant association of TLR9-1237T/C polymorphism with the risk of IBDs using the allele model (OR: 1.13; 95% CI: 1.00-1.27; p=0.05) (Fig. 2).
In order to clarify the potential difference in ethnicity, a subgroup analysis stratified by population group was performed in our study. Similarly, in Caucasians, there was significant or borderline-significant association between TLR9-1237T/C polymorphism and the risk of IBDs based on recessive (OR: 1.59; 95% CI: 1.02-2.47; p=0.04) (Fig. 3), homozygote (OR: 1.62; 95% CI: 1.04-2.52; p=0.03) (Fig. 4), and allele (OR: 1.12; 95% CI: 1.00-1.27; p=0.05) (Fig. 5) models. However, no significant association was found among Asian populations.
In the subgroup analysis stratified by clinical type, significant association of TLR9-1237T/C polymorphism with CD risk was found using recessive (OR: 1.69; 95% CI: 1.05-2.73; p=0.03) (Fig. 6), homozygote (OR: 1.74; 95% CI: 1.07-2.82; p=0.02) (Fig. 7) and allele (OR: 1.15; 95% CI: 1.01-1.32; p=0.04) (Fig. 8) genetic models. Unfortunately, we failed to find any statistical evidence of association between TLR9-1237T/C polymorphism and risk of disease in the UC subgroup when all contrasts were performed.
As shown in Table 3, there was no inter-study heterogeneity
among the overall studies of TLR9-1237T/C polymorphism
for all five genetic models (dominant model: Q=7.08, p=0.42,
I2=1%; recessive model: Q=1.48, p=0.92, I2=0%; heterozygote
comparison: Q=6.13, p=0.52, I2=0%; homozygote comparison: Q=1.85, p=0.87, I2=0%; allele model: Q=7.47, p=0.38, I2=6%).
Therefore, the fixed-effective model was used in our meta-analysis.
Potential publication bias was estimated by evaluating the funnel plot's shape and Egger's test in this meta-analysis. Egger's linear regression test showed a moderate publication bias for the recessive model (CC vs. TT+TC) in the UC subgroup (p=0.019); however, no evidence of publication bias was found for any other genetic models in the overall studies and subgroups (Table 3, Fig. 9).
The two major clinical types of IBDs, CD, and UC, are complicated and recurrent intestinal inflammatory disorders that are closely related to the susceptibility of colon cancer.28 CD is characterized by a transmural inflammation of the entire gastrointestinal tract. However, the inflammation of UC is non-transmural and mainly restricted to the colon.2 It has always been considered that IBDs result from an inappropriate inflammatory response to gut microbes in genetically susceptible hosts. Meanwhile, the characteristic of familiar aggregation may indicate a common genetic background across IBDs.29 To date, numerous genetic studies have significantly advanced our understanding of the pathogenesis of IBDs, and many susceptible genes have been identified.30,31,32 Among them, TLR9 gene has been highlighted.
TLR9 is a PRR of the TLR family that can mediate the innate immunity by specifically recognizing the CpG motifs of bacteria DNA.7 The TLR9 gene, located on chromosome 3p21.3, has numerous polymorphisms on its promoter region, and the -1237T/C polymorphism has been mostly studied.9101112 Accumulating evidence has suggested that TLR9-1237T/C polymorphism is associated with multiple inflammatory diseases including asthma,33 systemic lupus erythematosus (SLE),34 and rheumatoid arthritis (RA).35 Recently, a number of case-control studies have been published to illustrate the association of TLR9-1237T/C polymorphism with the susceptibility of IBDs; however, the results are contradictory.1415161718192021 Thus, we thoroughly searched for research on this topic and performed this meta-analysis. To our knowledge, this is the first comprehensive meta-analysis that attempts to determine the exact relationship between TLR9-1237T/C polymorphism and risk of IBDs.
A total of eight publications including 2987 cases and 2388 controls were retrieved in our meta-analysis. The impacts of dominant, recessive, heterozygote, homozygote, and allele genetic models were all evaluated. In addition, considering that the differences in genetic background may have influenced the outcome of the genetic association studies, we also conducted subgroup analyses stratified by ethnicity and disease type. Overall, our results indicated that TLR9-1237T/C polymorphism might act as a risk factor in IBDs. In the recessive model, the risk of IBDs in individuals with CC genotype was 1.59-fold higher than those with TT+TC genotype. On homozygote comparison, the risk of individuals with CC genotype was 1.62-fold higher than the TT carriers. Moreover, our study also suggested an increased risk of IBDs with C allele carriers compared to the T allele carriers, although the discrepancy was only borderline significant (p=0.05).
There were two types of populations in our meta-analysis: Caucasians and Asians. Our data suggested that there was a significant difference between the two ethnicities in the association between TLR9-1237T/C polymorphism and IBD risk. Among the studies involving Caucasians, we found a significant association between rs5743836 T/C polymorphism and the risk of IBDs using the recessive model and homozygote comparison. Furthermore, a borderline-significant association of TLR9-1237T/C polymorphism with IBDs was also found in the allele model. On the other hand, there was no statistical evidence for the association between TLR9-1237T/C polymorphism and the susceptibility of IBDs in Asians.
Considering that the potential clinical type discrepancy might influence the genotype distribution, we then performed the subgroup analyses stratified by disease phenotype. Eight studies were included in the CD subgroup, and our study indicated a pathogenic role of TLR9-1237T/C polymorphism in the development of CD. These results suggested that individuals with CC genotype might have higher risk of CD than those with TT+TC and TT genotypes. Moreover, the risk of CD was also increased in C allele carriers. However, there was no association between TLR9-1237T/C polymorphism and the susceptibility of UC.
As mentioned above, one published dataset indicated that the TLR9-1237T/C polymorphism could lead to a T to C exchange at the position -1237 of the TLR9 gene promoter, which would provide a binding site for transcript factor NF-κB.13 Hence, we speculate that the TLR9-1237T/C polymorphism may influence the susceptibility of IBDs by affecting the transcription of NF-κB. The findings in the subgroup analyses by ethnicity and clinical type were not consistent, suggesting that the association between TLR9-1237T/C polymorphism and risk of IBDs was ethnicity- and disease-specific.
Heterogeneity is a limitation that exists in meta-analyses and may reduce the statistical power and distort the final results. Thus, we performed a χ2-test-based Q test to assess the interstudy heterogeneity in our meta-analysis. Interestingly, there was no evidence of existing heterogeneity among overall study data or subgroup data using all five genetic models. Regarding publication bias, the funnel plot shapes for all five comparisons of overall studies, CD subgroups, Caucasian populations, and Asian populations were symmetrical, and Egger's test similarly did not provide any statistical evidence of publication bias (Table 3). However, there was moderate publication bias in the UC subgroup towards using the recessive model, which may have distorted our results.
Results in the present meta-analysis should be interpreted with caution due to the following limitations. Firstly, the number of studies and individuals were relatively small in our study, which would reduce the statistical power of the meta-analysis determining the relationship between TLR9-1237T/C polymorphism and IBD risk. Secondly, publication bias existed in several comparisons, and this may have distorted our results, as several studies with negative results may have been ignored or may not have been published. Thirdly, we only included literature that was focused on Caucasians and Asians, and future studies should contain more ethnicities.
In summary, our results remain significant despite these limitations. The findings from the present meta-analysis indicated that the TLR9-1237T/C polymorphism might act as a risk factor in the development of IBDs, particularly in Caucasians. Furthermore, our study also suggested a pathogenic role of this polymorphism in the development of CD. However, more large-scaled case-control studies are needed to further confirm our conclusions.
Figures and Tables
Fig. 2
Forest plots for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBDs. (A) Recessive model. (B) Homozygote comparison. (C) Allele model. CI, confidence interval; IBD, inflammatory bowel disease.

Fig. 3
Forest plot for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBDs stratified by ethnicity (recessive model). CI, confidence interval; IBD, inflammatory bowel disease.

Fig. 4
Forest plot for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBDs stratified by ethnicity (homozygote comparison). CI, confidence interval; IBD, inflammatory bowel disease.

Fig. 5
Forest plots for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBD stratified by ethnicity (allele model). CI, confidence interval; IBD, inflammatory bowel disease.

Fig. 6
Forest plot for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBDs stratified by clinical type (recessive model). CI, confidence interval; IBD, inflammatory bowel disease; CD, Crohn's disease; UC, ulcerative colitis.

Fig. 7
Forest plot for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBDs stratified by clinical type (homozygote comparison). CI, confidence interval; IBD, inflammatory bowel disease; CD, Crohn's disease; UC, ulcerative colitis.

Fig. 8
Forest plot for the meta-analysis of the association between TLR9 -1237T/C polymorphism and the susceptibility of IBDs stratified by clinical type (allele model). CI, confidence interval; IBD, inflammatory bowel disease; CD, Crohn's disease; UC, ulcerative colitis.

Fig. 9
Funnel plots for TLR9 -1237T/C polymorphism and IBDs: (A) dominant model, (B) recessive model, (C) heterozygote comparison, (D) homozygote comparison, and (E) allele model. Each point represents a separate study for the indicated association. SE, standardized effect; IBD, inflammatory bowel disease; OR, odds ratio.

Table 1
Characteristics of the References Included in Our Meta-Analysis

| First author | Year | Region | Ethnicity | Source of control | Genotyping method | Cases (n) | Controls (n) |
HWE (p value) |
Quality score | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IBD | CD | UC | |||||||||
| Hong21 | 2007 | New Zealand | Caucasian | PB | PCR-RFLP | 182 | 182 | - | 188 | 0.052 | 11 |
| Hotte20 | 2012 | Canada | Caucasian | HB | SDS | 29 | 15 | 14 | 21 | 0.512 | 8 |
| Petermann19 | 2009 | New Zealand | Caucasian | PB | Taqman | 793 | 387 | 406 | 412 | 0.641 | 13 |
| Shen18 | 2010 | China | Asian | HB | PCR-RFLP | 113 | 30 | 83 | 120 | 0.963 | 10 |
| Török16 | 2004 | Germany | Caucasian | PB | PCR-RFLP | 312 | 174 | 138 | 265 | 0.662 | 10 |
| Török17 | 2009 | Germany | Caucasian | PB | PCR-RFLP | 953 | 605 | 348 | 792 | 0.239 | 13 |
| Valverde-Villegas15 | 2014 | Brazil | Caucasian | PB | PCR-RFLP | 239 | 132 | 107 | 239 | 0.893 | 11 |
| Ye14 | 2009 | Korea | Asian | PB | MALDI-TOF | 366 | 366 | - | 351 | 0.978 | 12 |
PB, population-based; HB, hospital-based; PCR-RFLP, polymerase chain reaction-restriction fragment length polymorphism; SDS, single-direction-sequencing; MALDI-TOF, matrix-assisted laser desorption/ionization time of flight; IBD, inflammatory bowel disease; CD, Crohn's disease; UC, ulcerative colitis; HWE, Hardy-Weinberg equilibrium.
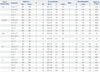
Table 2
Genotype and Allele Distributions of TLR9 -1237T/C Polymorphism in Cases and Controls
| References | IBD | CD | UC | Control | IBD | CD | UC | Control | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TT | TC | CC | TT | TC | CC | TT | TC | CC | TT | TC | CC | T | C | T | C | T | C | T | C | |
| Hong, et al.21 | 130 | 50 | 2 | 130 | 50 | 2 | - | - | - | 131 | 56 | 1 | 310 | 54 | 310 | 54 | - | - | 318 | 58 |
| Hotte, et al.20 | 21 | 6 | 2 | 11 | 4 | 0 | 10 | 2 | 2 | 15 | 5 | 1 | 48 | 10 | 26 | 4 | 22 | 6 | 35 | 7 |
| Petermann, et al.19 | 572 | 200 | 21 | 282 | 94 | 11 | 290 | 106 | 10 | 291 | 112 | 9 | 1344 | 242 | 658 | 116 | 686 | 126 | 694 | 130 |
| Shen, et al.18 | 110 | 3 | 0 | 29 | 1 | 0 | 81 | 2 | 0 | 119 | 1 | 0 | 223 | 3 | 59 | 1 | 164 | 2 | 239 | 1 |
| Török, et al.16 | 216 | 86 | 10 | 114 | 53 | 7 | 102 | 33 | 3 | 205 | 57 | 3 | 518 | 106 | 281 | 67 | 237 | 39 | 467 | 63 |
| Török, et al.17 | 691 | 245 | 17 | 435 | 159 | 11 | 256 | 86 | 6 | 593 | 189 | 10 | 1627 | 279 | 1029 | 181 | 598 | 98 | 1375 | 209 |
| Valverde-Villegas, et al.15 | 159 | 69 | 11 | 86 | 39 | 7 | 73 | 30 | 4 | 171 | 62 | 6 | 387 | 91 | 211 | 53 | 176 | 38 | 404 | 74 |
| Ye, et al.14 | 366 | 0 | 0 | 366 | 0 | 0 | - | - | - | 350 | 1 | 0 | 732 | 0 | 732 | 0 | - | - | 701 | 1 |
Table 3
Total and Subgroup Analyses of TLR9 -1237T/C Polymorphism in IBDs
ACKNOWLEDGEMENTS
This work was supported by research grants from the National Nature Science Foundation of China (No. 81270467).
References
2. Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007; 369:1641–1657.

3. Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004; 126:1504–1517.

4. Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007; 448:427–434.

5. Khor B, Gardet A, Xavier RJ. Genetics and pathogenesis of inflammatory bowel disease. Nature. 2011; 474:307–317.

8. Wagner H. Interactions between bacterial CpG-DNA and TLR9 bridge innate and adaptive immunity. Curr Opin Microbiol. 2002; 5:62–69.

9. Hampe J, Lynch NJ, Daniels S, Bridger S, Macpherson AJ, Stokkers P, et al. Fine mapping of the chromosome 3p susceptibility locus in inflammatory bowel disease. Gut. 2001; 48:191–197.

10. Omar AH, Yasunami M, Yamazaki A, Shibata H, Ofori MF, Akanmori BD, et al. Toll-like receptor 9 (TLR9) polymorphism associated with symptomatic malaria: a cohort study. Malar J. 2012; 11:168.

11. Berghöfer B, Frommer T, König IR, Ziegler A, Chakraborty T, Bein G, et al. Common human Toll-like receptor 9 polymorphisms and haplotypes: association with atopy and functional relevance. Clin Exp Allergy. 2005; 35:1147–1154.

12. Novak N, Yu CF, Bussmann C, Maintz L, Peng WM, Hart J, et al. Putative association of a TLR9 promoter polymorphism with atopic eczema. Allergy. 2007; 62:766–772.

13. Hamann L, Glaeser C, Hamprecht A, Gross M, Gomma A, Schumann RR. Toll-like receptor (TLR)-9 promotor polymorphisms and atherosclerosis. Clin Chim Acta. 2006; 364:303–307.

14. Ye BD, Yang SK, Song K, Yang DH, Yoon SM, Kim KJ, et al. [Association of Toll-like receptor gene with Crohn's disease in Koreans]. Korean J Gastroenterol. 2009; 54:377–383.

15. Valverde-Villegas JM, dos Santos BP, Machado MB, Jobim M, Jobim LF, Flores C, et al. G2848A and T-1237C polymorphisms of the TLR9 gene and susceptibility to inflammatory bowel disease in patients from southern Brazil. Tissue Antigens. 2014; 83:190–192.

16. Török HP, Glas J, Tonenchi L, Bruennler G, Folwaczny M, Folwaczny C. Crohn's disease is associated with a toll-like receptor-9 polymorphism. Gastroenterology. 2004; 127:365–366.

17. Török HP, Glas J, Endres I, Tonenchi L, Teshome MY, Wetzke M, et al. Epistasis between Toll-like receptor-9 polymorphisms and variants in NOD2 and IL23R modulates susceptibility to Crohn's disease. Am J Gastroenterol. 2009; 104:1723–1733.

18. Shen XY, Shi RH, Wang Y, Zhang HJ, Zhou XQ, Shen FC, et al. [Toll-like receptor gene polymorphisms and susceptibility to inflammatory bowel disease in Chinese Han and Caucasian populations]. Zhonghua Yi Xue Za Zhi. 2010; 90:1416–1420.
19. Petermann I, Huebner C, Browning BL, Gearry RB, Barclay ML, Kennedy M, et al. Interactions among genes influencing bacterial recognition increase IBD risk in a population-based New Zealand cohort. Hum Immunol. 2009; 70:440–446.

20. Hotte NS, Salim SY, Tso RH, Albert EJ, Bach P, Walker J, et al. Patients with inflammatory bowel disease exhibit dysregulated responses to microbial DNA. PLoS One. 2012; 7:e37932.

21. Hong J, Leung E, Fraser AG, Merriman TR, Vishnu P, Krissansen GW. TLR2, TLR4 and TLR9 polymorphisms and Crohn's disease in a New Zealand Caucasian cohort. J Gastroenterol Hepatol. 2007; 22:1760–1766.

22. Nakaoka H, Inoue I. Meta-analysis of genetic association studies: methodologies, between-study heterogeneity and winner's curse. J Hum Genet. 2009; 54:615–623.

23. Dai YE, Tang L, Healy J, Sinnett D. Contribution of polymorphisms in IKZF1 gene to childhood acute leukemia: a meta-analysis of 33 case-control studies. PLoS One. 2014; 9:e113748.

24. Thakkinstian A, D'Este C, Eisman J, Nguyen T, Attia J. Meta-analysis of molecular association studies: vitamin D receptor gene polymorphisms and BMD as a case study. J Bone Miner Res. 2004; 19:419–428.

25. Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997; 127:820–826.

26. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560.

27. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–634.

29. Bouma G, Strober W. The immunological and genetic basis of inflammatory bowel disease. Nat Rev Immunol. 2003; 3:521–533.

30. Van Limbergen J, Wilson DC, Satsangi J. The genetics of Crohn's disease. Annu Rev Genomics Hum Genet. 2009; 10:89–116.

31. Duerr RH, Taylor KD, Brant SR, Rioux JD, Silverberg MS, Daly MJ, et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science. 2006; 314:1461–1463.

32. Ogura Y, Bonen DK, Inohara N, Nicolae DL, Chen FF, Ramos R, et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn's disease. Nature. 2001; 411:603–606.

33. Lazarus R, Klimecki WT, Raby BA, Vercelli D, Palmer LJ, Kwiatkowski DJ, et al. Single-nucleotide polymorphisms in the Toll-like receptor 9 gene (TLR9): frequencies, pairwise linkage disequilibrium, and haplotypes in three U.S. ethnic groups and exploratory case-control disease association studies. Genomics. 2003; 81:85–91.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download