Abstract
Periprosthetic fractures after total knee arthroplasty (TKA) are gradually increasing, reflecting extended lifespan, osteoporosis, and the increasing proportion of the elderly during the past decade. Supracondylar periprosthetic femoral fracture is a potential complication after TKA. Generally, open reduction and internal fixation are the conventional option for periprosthetic fracture after TKA. However, the presence of severe comminution with component loosening can cause failure of internal fixation. Although the current concept for periprosthetic fracture is open reduction and internal fixation, we introduce an unusual case of revision arthroplasty using a MUTARS® prosthesis for a comminuted periprosthetic fracture in the distal femur after TKA, with technical tips.
Total joint arthroplasty procedures are constantly increasing, reflecting extended lifespan, osteoporosis, and the increased elderly population and leading to the increased prevalence of periprosthetic fracture. Periprosthetic fractures after total knee arthroplasty (TKA) are also gradually increasing.12345 Of the patients who undergo primary TKA, 0.3–2.5% are reported to sustain a periprosthetic fracture as a catastrophic complication of primary TKA.12346
Successful treatment of periprosthetic femur fractures requires careful understanding of the fracture pattern and bone quality in order to identify and execute a rational treatment approach and provide an appropriate postoperative recovery protocol.1 Generally, open reduction and internal fixation are the conventional option for periprosthetic fracture after TKA. However, the presence of severe comminution with loosening around the prosthesis can cause failure of internal fixation. Herein, we introduce a method of revision arthroplasty using a MUTARS® (Modular Universal Tumor And Revision System, Implantcast, Buxtehude, Germany) prosthesis for a comminuted periprosthetic fracture in the distal femur.
A 70-year-old woman underwent TKA for degenerative osteoarthritis in October 2009 at another hospital. In April 2014, she visited our emergency room for left knee pain after a passenger traffic accident. She had severe swelling around the knee, though no external wound. She had no problems in gait before the accident. There was no laboratory test evidence of infection. Laboratory investigation on admission revealed a white blood cell count of 9200/mL, an erythrocyte sedimentation rate of 10 mm/h, and a C-reactive protein level of 0.8 mg/dL. Abnormal findings were not observed in routine laboratory investigations. She had no osteoporosis: T-scores of L1–4 and the total femur were -1.3 and -0.9, respectively. Plain radiographs showed periprosthetic fracture of the distal femur with severe comminution; however, loosening of the femoral component was not observed clearly. The supracondylar fracture extended proximally to one third of the femoral shaft in the diaphysis combined with longitudinal splitting. The type of fracture was classified as type III (loose or failing prosthesis, regardless of fracture displacement) in the Lewis and Rorabeck classification and also type III (extended distally to the proximal border of the femoral component) in the Su classification (Fig. 1).78
The former arthroplasty was a PS-type TKA system (Maxim® total knee system; Biomet, Warsaw, IN, USA). After admission, we applied skeletal traction for the proximal tibia to decrease knee joint swelling before surgery. Surgery was performed 7 days after admission. Due to the severe comminution of the distal femur and the possibility of loosening of the implant, we prepared prostheses for both internal fixation and total revision arthroplasty.
The surgical approach was via the previous anterior midline incision extending to the proximal area. The knee was opened through a standard medial parapatellar arthrotomy with eversion of the patella. We extended the incision proximally to expose the diaphyseal fracture of the femur. We paid careful attention to the patellar tendon attachment to the tibial tubercle during all maneuvers, particularly during knee flexion and patellar retraction. The joint capsule was dissected off the posterior portion of the distal femur and tibia. Then, the collateral ligaments were detached from their femoral origin without neurovascular injury. We fixed the long spiral fracture of the diaphysis primarily with three cables, then attempted internal fixation of the distal femur in an intraoperative procedure. However, poor bone quality and severe comminution interfered with the rigid fixation. Furthermore, the design of the femoral component had a very high box-cutting level, making it impossible to attain bicondylar fixation using a lateral plate and screws.
Another option for this fracture to overcome severe comminution would have been preferred. Unfortunately, there was no option for this implant to fix or revise the femoral component extending the diaphysis. We waived the internal fixation using conventional lateral plating to prevent nonunion and fixation failure around the previous femoral component. However, it would normally be required for total revision to another implant (Fig. 2).
Therefore, we attempted to use a MUTARS® prosthesis to overcome these problems. Although another extended-revision prosthesis was considered, it was more difficult to fix a combined diaphyseal fracture using a conventional revision femoral component than when using a tumor prosthesis system. In addition, a conventional revision component could cause several complications including nonunion and fixation loss using bone cement. Thus, we used a cementless femoral tumor prosthesis to overcome these problems.
Before the removal of the former femoral component, we checked the transverse cutting level of the femoral diaphysis to adjust limb length, calculating the length of the revising femoral prosthesis (stem length 120 mm, component length 120 mm, diameter 15 mm) from the upper margin of the joint line. However, we focused on the stability of the femoral component rather than adjusting the limb length discrepancy. It was essential to maintain adequate tension around the cementless femoral prosthesis for bone ingrowth, as well as accurate adjustment for limb length so as to align with the contralateral limb. After the removal of the former distal femoral prosthesis with the comminuted bone fragments, a diaphyseal transverse cut was made perpendicular to the anatomical axis of the femoral shaft.
Then, the tibial component was removed using a conventional method, preserving as much tibial bone as possible. The direction of the former tibial component was checked. Once all of the components had been removed, the size of the deficit was measured to estimate the size of the femoral and tibial components for implanting.
The tibia was then cut, and the tibia deficit was built up in the standard fashion, using a tibial resection stylus and cutting block. After checking the quality of the cut, the cutting surface was drilled with the peg holes to complete the tibial bone preparation. The tibial components were then cemented with Palacos® R and G cement (Heraeus, Hanau, Germany) using a standard technique, based on the direction of the former tibial component to adjust tibial rotation.
Then, the femoral trial was applied and assembled on the tibial component to secure the hinge-type locking mechanism. Rotation of the femoral component was assessed by flexing and extending the knee and observing the patella tracking. The patella, which had previously been replaced, was retained. The rotation of the femoral implant was controlled and measured using the femoral component trial, according to the location of patella, without resulting in patella subluxation. After removing the femoral trial, cementless femoral stem fixation and femoral component insertion were performed with restoration of the femoral length. Care was taken to ensure that the leg was not lengthened.
After surgery, the patient wore thigh-length anti-embolic stockings, and the use of an ankle pump was applied in bed during hospitalization. Pharmacological prophylaxis for venous thromboembolism was conducted perioperatively using a subcutaneous injection of low-molecular-weight heparin (dalteparin) until self-ambulation with an assisted device was achieved. Three days after surgery, closed suction drainage was removed, and the patient was wheelchair-mobile. The patient walked with restricted weight bearing and the use of assistive devices (wheelchair, walker, crutches, or cane) at 7 days after surgery. Full weight bearing was allowed at 8 weeks postoperatively, confirming callus formation around the diaphyseal fracture site. After discharge, the patient was routinely followed to check radiographs at 6 weeks, 3, 6, and 12 months after surgery, and every 3 months thereafter. At her 12-month follow-up, she had resumed her previous level of activity.9 Range of motion was measured as a flexion contracture of 5 degrees, with further flexion of 95 degrees. There was no sign of infection around the knee at the final 24-month follow-up. The limb length discrepancy was measured as +1.5 cm at the final follow-up on physical examination. However, the patient did not recognize the difference. The Modified Hospital for Special Surgery knee score was measured as 86 points. Radiographs of the implant revealed stable fixation with diaphyseal bony union. Osteolysis or loosening was not observed (Fig. 3).
Periprosthetic supracondylar fractures of the femur after TKA represent a devastating complication for the patient and a technical challenge for the surgeon.110 Locking plating has become the treatment method of choice for many surgeons. This device offers many theoretical advantages, as the multiple locked distal screws provide both a fixed angle to prevent varus collapse and the ability to address distal fractures.111213 However, if it is impossible to perform internal fixation using a conventional method due to severe comminution, a tumor prosthesis system or an extended-revision system can be an alalternative option. In addition, allograft prosthesis composite is also a good alternative for periprosthetic fracture. However, it is much more technically difficult to operate than a tumor prosthesis, as it cannot solve the simultaneous problems of both diaphyseal femoral fracture and severe comminuted fracture around the femoral prosthesis. There are similar reports regarding the use of a distal femoral replacement for non-tumorous cases, including fractures.141516171819 We treated the patients successfully using a MUTARS® prosthesis for distal femur periprosthetic fracture with severe comminution. No other report has described the use of this system primarily for distal femur periprosthetic fracture.
Metal augmentation is generally required in the revision of a femoral component with periprosthetic fracture, due to the inevitable bone deficiency following component removal. Furthermore, it is recommended to use femoral stems routinely, as the stems engage the femoral diaphysis for both alignment and stable fixation.120 In this case, we prepared both internal fixation and revision replacement systems. Initially, we attempted open reduction and internal fixation to save the intact tibial component, despite severe comminution of the unstable femoral component. However, it was impossible to maintain stable fixation using a locking plate and screws, as the distal part of the fracture was too close to the implant and notable loosening was evident. Furthermore, the box-cutting level of the former implant was too high for the conventional femoral component; thus, it was difficult to advance screws from the lateral condyle to the medial condyle in order to achieve sufficient fixation. We waived internal fixation and instead performed total revision surgery using a MUTARS® prosthesis.
Successful treatment of periprosthetic fractures of the distal femur is very difficult and challenging, particularly considering that such fractures are associated with compromised bone stock, loss of ligamentous attachments, and elderly patients who do not tolerate prolonged immobility.117 The goal of surgery for these periprosthetic fractures is to restore the limb's structural ability to bear weight, ligamentous integrity, and knee range of motion, while minimizing complications.
We successfully treated a patient with a distal femur periprosthetic fracture with severe comminution using a MUTARS® prosthesis without notable complications. We recommend that surgeons could consider total revision surgery when it is impossible to obtain sufficient fixation in periprosthetic fracture around the distal femoral component.
Figures and Tables
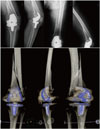 | Fig. 1Preoperative plain radiographs show distal femur periprosthetic fracture with severe comminution and implant loosening. Three-dimensional reconstruction of preoperative computed tomography showed severe comminuted fracture around the prosthesis, combining diaphyseal extension. |
References
2. McGraw P, Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol. 2010; 11:135–141.

4. Ayers DC. Supracondylar fracture of the distal femur proximal to a total knee replacement. Instr Course Lect. 1997; 46:197–203.
5. Yoo JH, Park SH, Han CD, Oh HC, Park JY, Choi SJ. Radiologic outcomes according to varus deformity in minimally invasive surgery total knee arthroplasty. Yonsei Med J. 2016; 57:225–231.

6. Meek RM, Norwood T, Smith R, Brenkel IJ, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011; 93:96–101.

7. Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg. 2004; 12:12–20.

8. Rorabeck CH, Taylor JW. Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am. 1999; 30:209–214.

9. Ji HM, Lee YK, Ha YC, Kim KC, Koo KH. Little impact of antiplatelet agents on venous thromboembolism after hip fracture surgery. J Korean Med Sci. 2011; 26:1625–1629.

10. Refaat M, Coleman S, Meehan JP, Jamali AA. Periprosthetic supracondylar femur fracture treated with spanning external fixation. Am J Orthop (Belle Mead NJ). 2015; 44:90–93.
11. Leonidou A, Moazen M, Lepetsos P, Graham SM, Macheras GA, Tsiridis E. The biomechanical effect of bone quality and fracture topography on locking plate fixation in periprosthetic femoral fractures. Injury. 2015; 46:213–217.

12. Streubel PN, Gardner MJ, Morshed S, Collinge CA, Gallagher B, Ricci WM. Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? J Bone Joint Surg Br. 2010; 92:527–534.

13. Kolb K, Koller H, Lorenz I, Holz U, Marx F, Grützner P, et al. Operative treatment of distal femoral fractures above total knee arthroplasty with the indirect reduction technique: a long-term follow-up study. Injury. 2009; 40:433–439.

14. Jassim SS, McNamara I, Hopgood P. Distal femoral replacement in periprosthetic fracture around total knee arthroplasty. Injury. 2014; 45:550–553.

15. Berend KR, Lombardi AV Jr. Distal femoral replacement in nontumor cases with severe bone loss and instability. Clin Orthop Relat Res. 2009; 467:485–492.

16. Appleton P, Moran M, Houshian S, Robinson CM. Distal femoral fractures treated by hinged total knee replacement in elderly patients. J Bone Joint Surg Br. 2006; 88:1065–1070.

17. Saidi K, Ben-Lulu O, Tsuji M, Safir O, Gross AE, Backstein D. Supracondylar periprosthetic fractures of the knee in the elderly patients: a comparison of treatment using allograft-implant composites, standard revision components, distal femoral replacement prosthesis. J Arthroplasty. 2014; 29:110–114.

18. Moran MC. Treatment of periprosthetic fractures around total hip arthroplasty with an extensively coated femoral component. J Arthroplasty. 1996; 11:981–988.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download