Abstract
Purpose
Most of the reports on instrumentalists' experiences of temporomandibular disorders (TMD) have been reported not by clinical examinations but by subjective questionnaires. The aim of this study was to investigate the clinical signs and subjective symptoms of TMD in a large number of instrumentalists objectively.
Materials and Methods
A total of 739 musicians from a diverse range of instrument groups completed a TMD questionnaire. Among those who reported at least one symptom of TMD, 71 volunteers underwent clinical examinations and radiography for diag-nosis.
Results
Overall, 453 participants (61.3%) reported having one or more symptoms of TMD. The most frequently reported symptom was a clicking or popping sound, followed by temporomandibular joint (TMJ) pain, muscle pain, crepitus, and mouth opening limitations. Compared with lower-string instrumentalists, a clicking or popping sound was about 1.8 and 2 times more frequent in woodwind and brass instrumentalists, respectively. TMJ pain was about 3.2, 2.8, and 3.2 times more frequent in upper-string, woodwind, and brass instrumentalists, respectively. Muscle pain was about 1.5 times more frequent in instrumentalists with an elevated arm position than in those with a neutral arm position. The most frequent diagnosis was myalgia or myofascial pain (MFP), followed by disc displacement with reduction. Myalgia or MFP was 4.6 times more frequent in those practicing for no less than 3.5 hours daily than in those practicing for less than 3.5 hours.
Temporomandibular disorders (TMD) constitute a broad group of clinical problems that involve the muscles of mastication, the temporomandibular joint (TMJ), and associated orofacial structures. Symptoms of TMD include a decreased range of motion of the mandible, pain in the masticatory musculatures, TMJ pain, joint sounds associated with function, generalized myofascial pain (MFP), and a functional limitation or deviation in jaw opening.1 The most frequently reported symptom of TMD is pain, which is usually located in the masticatory muscles, the TMJ, and/or the preauricular area.2 Other symptoms such as neck ache, facial pain, earache, tinnitus, and perceived hearing loss have also been described.2 The frequency of TMD has been reported to range from 30% to 39.2%.3456
The etiology of TMD is multifactorial, with neuromuscular, neurobiological, biomechanical, and biopsychosocial factors having been identified.7 Certain parafunctional habits such as bruxism, tooth clenching, and chewing gum are also thought to potentially increase the risk of developing TMD.891011 TMD are closely associated with lifestyle and occupational characteristics. In particular, it has been reported that many instrumentalists experience TMD signs and symptoms that are attributable to heavy use of the jaw or mouth, and constant tension of the head and neck muscles. Due to the high physical and psychological demands when playing musical instruments, musicians are at risk of developing various health problems.12 Many musicians practice daily for several hours, and this can result in long-term, repetitive force application to the head, mandible, and facial muscles, which may lead to malocclusion and other deformations of the stomatognathic system.13
A study involving 408 musicians of the Berlin and Saxony-Anhalt orchestra found that craniomandibular disorders were common, with half of the musicians reporting orofacial pain.14 Another questionnaire study involving 73 musicians of a Finnish orchestra revealed that 56% of them reported at least one TMD symptom.15 The type of instrument played may determine which occupational disorders or diseases are more likely to affect a musician.16 For example, playing upper-string instruments such as viola and violin, which are held between the shoulder and the angle of the jaw, can induce TMD or aggravate already existing TMD by overloading the masticatory muscles and orofacial skeletal system.17 Previous studies have shown that violists or violinists often report TMD signs and symptoms.181920 The specific playing techniques used by woodwind and brass instrumentalists involve upwards and backwards movement of the mandible, which can directly impact the TMJ and compress it so as to contribute to the development of TMD.21 Playing a wind instrument is a complex neuromuscular task requiring increased respiration and orofacial muscle activity,2223 and a questionnaire study involving Lebanese musicians found TMD in 23% of 340 wind instrumentalists.24
Most previous studies on the association between playing musical instruments and TMD have considered only subjective symptoms or have been limited to small populations. Several studies have also carried out objective clinical examinations and radiography; however, such studies were limited to examining specific instrument groups such as violists, violinists, or wind instrumentalists. Thus, the present study investigated the characteristics of TMD in instrumentalists by evaluating both subjective symptoms via a TMD questionnaire and clinical diagnoses via clinical examination and radiography in a large number of instrumentalists.
In total, 841 people including professional orchestra members and high-school and college students majoring in musical instrument performance were asked to fill out a TMD questionnaire. The instruments played included the cello, double bass, viola, violin, daegeum, flute, clarinet, saxophone, bassoon, oboe, horn, trombone, trumpet, tuba, harp, percussion, and piano. Exclusion criteria comprised a previous history of orthodontic treatment or jaw trauma and failure to fill out the questionnaire completely and ultimately left 739 subjects to be analyzed in the study. Among those who reported at least one symptom of TMD, 71 subjects volunteered to visit the dental clinic (Department of Orofacial Pain and Oral Medicine, College of Dentistry, Yonsei University, Seoul, Korea) to undergo clinical examination and radiography necessary for a clinical diagnosis (Fig. 1). The present survey and examination were performed from March 2012 to December 2012.
Various subjective symptoms were evaluated using a TMD questionnaire, which consisted of five questions that queried the characteristics of TMJ pain, masticatory muscle pain, TMJ sounds (clicking/popping or crepitus), difficulty during mouth opening (MO), and oral parafunctional habits (bruxism or clenching) (Table 1).6 Information on the following background characteristics was also obtained: gender, age, instrument played, length of playing experience, and experience of orthodontic treatment or jaw trauma. The questionnaire included a number of multiple-choice questions.
According to the collected questionnaires, the suspected diagnoses of the 739 volunteers were assessed by an orofacial pain specialist in the clinic.
Clinical signs of TMD were evaluated by utilizing a combination of clinical and radiographic examinations to describe the characteristics of the symptoms of disc displacement with reduction (DD w/ R); disc displacement without reduction (DD w/o R); TMJ arthralgia, myalgia, or MFP; TMJ osteoarthritis (TMJ OA); and TMJ osteoarthrosis (TMJ O). The clinical diagnoses were made according to the Diagnostic Criteria for TMD. The clinical examinations included palpation of the TMJ, temporalis muscles, and masseter muscles. The intensity of TMJ or muscle pain was assessed with a visual analog scale ranging from 0 to 10. The presence of TMJ noise was evaluated. Ranges of jaw motion (maximum MO, protrusion, and lateral movement) were measured in millimeters using a ruler. Attrition, tongue ridging, and cheek ridging were also evaluated. Panoramic and transcranial radiography were performed. The clinical examination, radiograph test, and diagnosis were performed by a single examiner.
TMD symptoms were evaluated in relation to gender, age groups, and the length of playing experience: <10 years and ≥10 years. This cutoff corresponded to the median for the total study population.
Subjects were also evaluated in relation to the type of instrument: lower strings (cello and double bass), upper strings (viola and violin), woodwind (daegeum, flute, clarinet, saxophone, bassoon, and oboe), brass (horn, trombone, trumpet, and tuba), and other (harp, percussion, and piano).
Additionally, we compared the type of wind instrument: small mouth aperture (daegeum and flute), single reed (clarinet and saxophone), and double reed (bassoon and oboe).
Subjects were also evaluated in relation to the arm position while playing. Arm position was divided into two groups: neutral arm position (<40° elevation of the arm while playing) and elevated arm position (≥40° elevation of the arm while playing). This cutoff was chosen based on a study by Nyman, et al.25 (Fig. 2). Instruments played with a neutral arm position included the cello, double bass, clarinet, saxophone, bassoon, oboe, horn, tuba, and piano. Instruments played with an elevated arm position included the viola, violin, daegeum, flute, trombone, trumpet, harp, and percussion.
TMD symptoms were evaluated in relation to the presence of oral parafunctional habits such as bruxism or clenching.
TMD diagnoses were evaluated in relation to gender, age groups, and the length of playing experience: <14 years and ≥14 years. This cutoff corresponded to the median for the 71 instrumentalists. Subjects were also evaluated in relation to the type of instrument, the arm position, and the presence of oral parafunctional habits such as bruxism or clenching.
We also analyzed the number of hours of daily practice. The cohort was divided into two groups: <3.5 hours and ≥3.5 hours. This cutoff corresponded to the median for the 71 instrumentalists. Data for the hours of daily practice were collected during the interview at the time of the clinical examinations, as this information was not included in the TMD questionnaire.
Additionally, we compared the ranges of jaw motion according to the type of instrument.
For data on the 739 subjects who responded to the TMD questionnaire, mean and standard deviation (SD) values of age and length of playing experience were calculated. For data on the 71 subjects who underwent clinical examinations and radiography, mean and SD values of age, length of playing experience, and hours of daily practice were calculated.
Logistic regression analysis was applied. Potential confounders were considered: gender, age, length of playing experience, hours of daily practice, types of all instruments, types of wind instruments, arm position while playing, and the presence of oral parafunctional habits. Potential confounders were first examined by means of logistic regression analysis, and if found to be associated with the outcome of interest, the confounder was included in the succeeding analysis. The association between the variables and the outcome of interest was determined by performing logistic regression analysis adjusted for potential confounders, and the adjusted odds ratio and 95% confidence interval were calculated.
All statistical analyses were performed using the SPSS software package (version 21.0, IBM, Armonk, NY, USA). The cutoff for statistical significance was a probability value of p<0.05.
The 739 included subjects comprised 191 men and 548 women aged 15 to 48 years (24.3±6.9 years, mean±SD), with a length of playing experience of 12.0±7.2 years. The study participants comprised 100 lower-string instrumentalists (56 cello and 44 double bass), 289 upper-string instrumentalists (63 viola and 226 violin), 169 woodwind instrumentalists (1 daegeum, 58 flute, 44 clarinet, 7 saxophone, 28 bassoon, and 31 oboe), 160 brass instrumentalists (51 horn, 49 trombone, 52 trumpet, and 8 tuba), and 21 players of other instruments (2 harp, 17 percussion, and 2 piano).
Among them, 453 participants (61.3%) reported having one or more symptoms of TMD. The most frequently reported symptom was a clicking or popping sound (n=338, 45.7%), followed by TMJ pain (n=177, 24.0%), muscle pain (n=156, 21.1%), crepitus (n=51, 6.9%), and MO limitation (n=1, 0.1%) (Table 2, Fig. 3). No symptoms were reported by 286 of the 739 participants (38.7%).
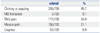
Among all variables, gender, age, type of instrument, and the presence of oral parafunctional habits were included in the succeeding analysis and were found to be statistically significant predictors of a clicking or popping sound. A clicking or popping sound was 1.7 times more frequent in females than in males. Compared with adolescents (aged 10–19 years), a clicking or popping sound was about 1.6 times more frequent in subjects aged 20–29 years. Compared with lower-string instrumentalists, a clicking or popping sound was about 1.8 and 2 times more frequent in woodwind and brass instrumentalists, respectively. A clicking or popping sound was about 1.9 times more frequent in the presence of oral parafunctional habits (Table 3). No variables were associated with crepitus or the presence of MO limitations.
Additionally, gender, type of instrument, and the presence of oral parafunctional habits were statistically significant predictors of TMJ pain, which was 1.8 times more frequent in females than in males. Compared with lower-string instrumentalists, TMJ pain was about 3.2, 2.8, and 3.2 times more frequent in upper-string, woodwind, and brass instrumentalists, respectively. TMJ pain was also about 1.8 times more frequent in the presence of oral parafunctional habits (Table 4).
Among all variables, gender, age, and arm position while playing were statistically significant predictors of muscle pain, which was 1.9 times more frequent in females than in males. Compared with adolescents (aged 10–19 years), muscle pain was about 2 and 2.5 times more frequent in subjects aged 20–29 years and 30–39 years, respectively. Muscle pain was about 1.5 times more frequent in instrumentalists with an elevated arm position than in those with a neutral arm position (Table 5).
No TMD symptoms were significantly related to the length of playing experience or the type of wind instrument (small mouth aperture, single reed, or double reed).
The 71 subjects who underwent clinical examination and radiography comprised 9 men and 62 women aged 17 to 48 years (25.1±6.9 years) with a length of playing experience of 13.5±7.0 years; they practiced for 3.8±1.5 hours daily. These subjects included 32 wind instrumentalists (1 daegeum, 7 flute, 2 clarinet, 3 bassoon, 5 oboe, 3 horn, 2 trombone, 7 trumpet, and 2 tuba) and 39 string instrumentalists (2 cello, 1 double bass, 7 viola, and 29 violin).
The most frequently diagnosed disease was myalgia or MFP (n=59, 83.1%), followed by DD w/ R (n=54, 76.1%), TMJ arthralgia (n=44, 62.0%), TMJ OA or TMJ O (n=6, 8.5%), and DD w/o R (n=1, 1.4%) (Table 6, Fig. 4).
Evaluations of the associations between the TMD diagnoses and the variables produced the outcomes described below. Among all variables, length of playing experience was included in the succeeding analysis and was a statistically significant predictor of DD w/ R, which was 3.5 times more frequent in those with ≥14 years of playing experience than in those with <14 years of playing experience (Table 7). No variables were associated with DD w/o R.
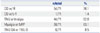
Additionally, gender and length of playing experience were statistically significant predictors of TMJ arthralgia, which was about 5.2 times more frequent in females than in males and was less common in those with ≥14 years of playing experience than in those with <14 years of playing experience (Table 8). Among all variables, the number of daily hours of practice was a statistically significant predictor of myalgia or MFP, which was 4.6 times more frequent in those practicing for ≥3.5 hours daily than in those with <3.5 hours of daily practice (Table 9). No variables were associated with the presence of TMJ OA or TMJ O. The maximum MO, protrusion, and lateral movements did not differ significantly between the two instrument groups (Table 10).
This study investigated the characteristics of TMD in instrumentalists by evaluating both subjective symptoms via a TMD questionnaire and clinical diagnoses via clinical examination and radiography in a large number of instrumentalists. Of the 739 subjects who completed the questionnaire, 453 (61.3%) reported that they had at least one TMD symptom. In previous studies, the frequency of TMD among the general population ranged from 30% to 39.2%. The present results therefore indicate that the frequency of TMD symptoms is much higher in instrumentalists than in the general population. It has been reported that the association of TMD signs and symptoms and the playing of instruments may be related to heavy use of the jaw or mouth and constant tension of the head and neck muscles.12
TMD are reportedly 1.5 to 2 times more frequent in females than in males.26 In the present study, the frequencies of clicking or popping sound, TMJ pain, and muscle pain differed significantly with gender. These symptoms were 1.7 to 1.9 times more frequent in women than in men, which is similar to the frequency observed in the general population.26
TMD are also more common in young people. In the present study, the frequencies of clicking or popping sound and muscle pain differed significantly with age. A clicking or popping sound was more common in participants aged 20–29 years, and muscle pain was more common in participants aged 20–29 years and 30–39 years.
The frequencies of clicking or popping sound and TMJ pain differed significantly with the type of instrument. A clicking or popping sound was more common in woodwind and brass instrumentalists, while TMJ pain was more frequent in upper-string, woodwind, and brass instrumentalists.
Joint problems develop frequently in wind instrumentalists, and it is thought that the act of instrumental performance may play a contributory role by increasing intra-articular pressure. Heikkilä, et al.15 reported that TMJ sounds and facial pain were more common in wind instrumentalists, due to the head and neck muscles being involved in the production of sound with a wind instrument.
Muscle pain differed significantly with the arm position while playing in the present study. The frequency of muscle pain was higher in instrumentalists playing with an elevated arm position than in those playing with a neutral arm position. This was probably related to the posture adopted while playing. When musicians of instruments requiring an elevated arm position sustain poor posture, a continuous deep pain input persists and may induce neck and shoulder pain as well as a secondary effect of inducing facial muscle pain. The TMJ pain that appears frequently in upper-string instrumentalists may be related to the finding that instrumentalists requiring an elevated arm position had greater rates of muscle pain. As a result of such muscle pain, intra-articular pressure may increase and induce TMJ pain. It has been shown that symptoms of TMD are activated and accentuated by playing and practicing as well as by non-ergonomic working conditions (e.g., poor posture and muscle tension).27
The frequency of craniomandibular disorders was reported to be particularly high in viola and violin players, reaching 74% in previous studies18192028 and 83% in the current study. Viola and violin players adopt a specific technique of holding the instrument to one side of the body, causing more frequent problems on one side of the orofacial region than on the other.1929 Cases of premature TMJ degeneration and its impact on bony facial structures have also been described in violists and violinists.3031 Attallah, et al.17 reported that clinical signs of TMD are more common in professional players than in matched controls and that playing the viola or violin seems to be a factor associated with TMD.181920 This may be attributed to the mechanical overload placed on the orofacial region32 or to the tendency to push the mandible toward the contralateral TMJ while playing the viola and violin.1833 By stabilizing the instrument with the chin, players exert pressure on the chinrest and mandible toward the right TMJ, resulting in mechanical stress to the joint.34
Steinmetz, et al.14 reported that lower-string instrumentalists whose playing technique did not involve orofacial structures reported fewer TMD symptoms, suggesting the presence of non-playing-related causes of TMD, such as stress, stage fright, or other psychological factors.
Musicians with oral parafunctional habits had a significantly higher frequency of TMJ pain in this study. Previous studies found that certain parafunctional habits such as bruxism, teeth clenching, and chewing gum might increase the risk of developing TMD.891011
The most frequent clinical diagnosis in the present study was myalgia or MFP. While 83.1% of the 71 subjects had clinical signs of myalgia or MFP, only 57.7% of the 71 subjects reported muscle pain, which is the equivalent subjective symptom of myalgia or MFP. This finding suggests that instrumentalists often confuse muscle pain with joint pain, resulting in an underreporting of the former. Musicians also often undervalue or hide their problems and neglect signals to rest or seek medical care.16 These factors may result in them not receiving appropriate treatment, resulting in an elevated frequency of TMD symptoms among affected musicians.
The relationship between hours of practice and TMD remains unclear. While several studies have found a correlation between the number of hours of practice per week and signs of TMD in violinists,35 others have found no association between the appearance of TMD in violinists and either the total duration of playing or the hours of practice.20 In the present study, the frequencies of TMJ arthralgia and DD w/ R differed significantly with the length of playing experience, with instrumentalists who had played for ≥14 years reporting a higher frequency of DD w/ R yet a lower frequency of TMJ arthralgia. It is thought that pain, unlike discs (which persist once displaced), is adaptable as time elapses; thus, instrumentalists may be capable of adjusting their methods of playing to remove painful strain on the joint.
The frequency of myalgia or MFP was also significantly related to the number of hours of practice daily, with myalgia or MFP being more common in those who practiced ≥3.5 hours daily. This may be due to overuse and tension of the muscle; therefore, reducing the playing time could alleviate TMD and other symptoms caused by muscle overuse.
The main limitations of this study were the relatively young age of subjects and the inclusion of a predominantly female population. Although a large number of instrumentalists were included, the results may have been biased, as TMD are known to be more common in young people and women. This also meant that we could not clearly define whether TMD were due to instrumental playing or the effects of age and gender. Future studies involving controlled populations of instrumentalists are needed to reduce the possibility of gender and age bias.
In conclusion, of the 739 instrumentalists, 61.3% reported having one or more symptoms of TMD. The most frequently reported subjective symptom in instrumentalists was a clicking or popping sound, and the most common clinical diagnosis in instrumentalists was myalgia or MFP. A clicking or popping sound was frequently reported by woodwind and brass instrumentalists, and TMJ pain was reported more often by upper-string, woodwind, and brass instrumentalists. Muscle pain was more common in those with an elevated arm position (≥40° elevation of the arm while playing) than in those with a neutral arm position (<40° elevation of the arm while playing).
In terms of clinical signs, the frequency of DD w/ R increased with the number of years of playing experience, while the frequency of TMJ arthralgia decreased. Additionally, instrumentalists with more hours of daily practice time were more likely to have myalgia or MFP.
Figures and Tables
 | Fig. 2Arm position was divided into two groups: neutral arm position (<40° elevation of the arm while playing: clarinet, French horn, bassoon, oboe, cello, double bass) and elevated arm position (≥40° elevation of the arm while playing: flute, trumpet, trombone, violin, viola). Adapted from Nyman, et al. Am J Ind Med 2007;50:370-6.25 |
 | Fig. 3Frequency of subjective symptoms in 739 subjects (patients could report more than one subjective symptom). MO, mouth opening; TMJ, temporomandibular joint. |
 | Fig. 4Frequency of clinical diagnoses in 71 subjects (multiple diagnoses per patient were possible). DD w/ R, disc displacement with reduction; DD w/o R, disc displacement without reduction; TMJ, temporomandibular joint; MFP, myofascial pain; TMJ OA, TMJ osteoarthritis; TMJ O, TMJ osteoarthrosis. |
Table 1
TMD Questionnaire

Table 2
Frequency of Subjective Symptoms in 739 Subjects (Patients Could Report More Than One Subjective Symptom)
| n/total | % | |
|---|---|---|
| Clicking or popping | 338/739 | 45.7 |
| MO limitation | 1/739 | 0.1 |
| TMJ pain | 177/739 | 24.0 |
| Muscle pain | 156/739 | 21.1 |
| Crepitus | 51/739 | 6.9 |
Table 3
Logistic Regression Analysis of the Potential Predictors of a Clicking or Popping Sound

Table 4
Logistic Regression Analysis of the Potential Predictors of TMJ Pain

Table 5
Logistic Regression Analysis of the Potential Predictors of Muscle Pain
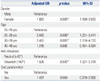
Table 6
Frequency of Clinical Diagnoses in 71 Subjects (Multiple Diagnoses per Patient Were Possible)
| n/total | % | |
|---|---|---|
| DD w/ R | 54/71 | 76.1 |
| DD w/o R | 1/71 | 1.4 |
| TMJ arthralgia | 44/71 | 62.0 |
| Myalgia or MFP | 59/71 | 83.1 |
| TMJ OA or TMJ O | 6/71 | 8.5 |
Table 7
Logistic Regression Analysis of the Potential Predictors of DD w/ R

| Adjusted OR | p value | 95% CI | |
|---|---|---|---|
| Playing experience | |||
| <14 yrs | Reference | ||
| ≥14 yrs | 3.491 | 0.037* | 1.077–11.316 |
Table 8
Logistic Regression Analysis of the Potential Predictors of TMJ Arthralgia

| Adjusted OR | p value | 95% CI | |
|---|---|---|---|
| Gender | |||
| Male | Reference | ||
| Female | 5.230 | 0.043* | 1.057–25.868 |
| Playing experience | |||
| <14 yrs | Reference | ||
| ≥14 yrs | 0.247 | 0.012* | 0.083–0.734 |
References
1. Wadhwa S, Kapila S. TMJ disorders: future innovations in diagnostics and therapeutics. J Dent Educ. 2008; 72:930–947.

2. Leeuw Rd. Orofacial pain: guidelines for assessment, diagnosis, and management. 4th ed. Chicago, London: Quintessence Books;2008.
3. Goulet JP, Lavigne GJ, Lund JP. Jaw pain prevalence among French-speaking Canadians in Québec and related symptoms of temporomandibular disorders. J Dent Res. 1995; 74:1738–1744.

4. Pow EH, Leung KC, McMillan AS. Prevalence of symptoms associated with temporomandibular disorders in Hong Kong Chinese. J Orofac Pain. 2001; 15:228–234.
5. Nekora-Azak A, Evlioglu G, Ordulu M, Is¸sever H. Prevalence of symptoms associated with temporomandibular disorders in a Turkish population. J Oral Rehabil. 2006; 33:81–84.

6. GonÇalves DA, Dal Fabbro AL, Campos JA, Bigal ME, Speciali JG. Symptoms of temporomandibular disorders in the population: an epidemiological study. J Orofac Pain. 2010; 24:270–278.
7. Suvinen TI, Reade PC, Kemppainen P, Könönen M, Dworkin SF. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005; 9:613–633.

8. Winocur E, Gavish A, Finkelshtein T, Halachmi M, Gazit E. Oral habits among adolescent girls and their association with symptoms of temporomandibular disorders. J Oral Rehabil. 2001; 28:624–629.

9. Karibe H, Goddard G, Gear RW. Sex differences in masticatory muscle pain after chewing. J Dent Res. 2003; 82:112–116.

10. Miyake R, Ohkubo R, Takehara J, Morita M. Oral parafunctions and association with symptoms of temporomandibular disorders in Japanese university students. J Oral Rehabil. 2004; 31:518–523.

11. Rossetti LM, Pereira de Araujo Cdos R, Rossetti PH, Conti PC. Association between rhythmic masticatory muscle activity during sleep and masticatory myofascial pain: a polysomnographic study. J Orofac Pain. 2008; 22:190–200.
12. Foxman I, Burgel BJ. Musician health and safety: preventing playing-related musculoskeletal disorders. AAOHN J. 2006; 54:309–316.
13. Głowacka A, Matthews-Kozanecka M, Kawala M, Kawala B. The impact of the long-term playing of musical instruments on the stomatognathic system - review. Adv Clin Exp Med. 2014; 23:143–146.

14. Steinmetz A, Zeh A, Delank KS, Peroz I. Symptoms of craniomandibular dysfunction in professional orchestra musicians. Occup Med (Lond). 2014; 64:17–22.

15. Heikkilä J, Hamberg L, Meurman JH. Temporomandibular disorders: symptoms and facial pain in orchestra musicians in Finland. Music Med. 2012; 4:171–176.

16. Zuskin E, Schachter EN, Kolcić I, Polasek O, Mustajbegović J, Arumugam U. Health problems in musicians--a review. Acta Dermatovenerol Croat. 2005; 13:247–251.
17. Attallah MM, Visscher CM, van Selms MK, Lobbezoo F. Is there an association between temporomandibular disorders and playing a musical instrument? A review of literature. J Oral Rehabil. 2014; 41:532–541.

18. Hirsch JA, McCall WD Jr, Bishop B. Jaw dysfunction in viola and violin players. J Am Dent Assoc. 1982; 104:838–843.

19. Kovero O, Könönen M. Signs and symptoms of temporomandibular disorders and radiologically observed abnormalities in the condyles of the temporomandibular joints of professional violin and viola players. Acta Odontol Scand. 1995; 53:81–84.

20. Rodríguez-Lozano FJ, Sáez-Yuguero MR, Bermejo-Fenoll A. Prevalence of temporomandibular disorder-related findings in violinists compared with control subjects. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:e15–e19.

21. Gualtieri PA. May Johnny or Janie play the clarinet? The Eastman Study: a report on the orthodontic evaluations of college-level and professional musicians who play brass and woodwind instruments. Am J Orthod. 1979; 76:260–276.
22. Prensky HD, Shapiro GI, Silverman SI. Dental diagnosis and treatment for musicians. Spec Care Dentist. 1986; 6:198–202.

23. Howard JA, Lovrovich AT. Wind instruments: their interplay with orofacial structures. Med Probl Perform Art. 1989; 4:59–72.
24. Sayegh Ghoussoub M, Ghoussoub K, Chaaya A, Sleilaty G, Joubrel I, Rifaï K. [Orofacial and hearing specific problems among 340 wind instrumentalists in Lebanon]. J Med Liban. 2008; 56:159–167.
25. Nyman T, Wiktorin C, Mulder M, Johansson YL. Work postures and neck-shoulder pain among orchestra musicians. Am J Ind Med. 2007; 50:370–376.

26. LeResche L. Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med. 1997; 8:291–305.

27. Taddey JJ. Musicians and temporomandibular disorders: prevalence and occupational etiologic considerations. Cranio. 1992; 10:241–244.

28. Kovero O, Könönen M. Signs and symptoms of temporomandibular disorders in adolescent violin players. Acta Odontol Scand. 1996; 54:271–274.

29. Steinmetz A, Ridder PH, Methfessel G, Muche B. Professional musicians with craniomandibular dysfunctions treated with oral splints. Cranio. 2009; 27:221–230.

31. Okner M, Kernozek T. Chinrest pressure in violin playing: type of music, chin rest, and shoulder pad as possible mediators. Clin Biomech (Bristol, Avon). 1997; 12:S12–S13.

32. Steinmetz A, Ridder PH, Reichelt A. Craniomandibular dysfunction and violin playing: prevalence and the influence of oral splints on head and neck muscles in violinists. Med Probl Perform Art. 2006; 21:183–189.

33. Kovero O. Degenerative temporomandibular joint disease in a young violinist. Dentomaxillofac Radiol. 1989; 18:133–135.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download