Abstract
Purpose
Materials and Methods
Results
Figures and Tables
Fig. 1
The mean profile graph of the toric and LRI groups. Toric group, toric foldable iris-fixated phakic intraocular lens implantation; LRI group, non-toric foldable iris-fixated phakic intraocular lens implantation with limbal relaxing incisions.

Fig. 2
Comparison of astigmatism severity before and 6 months after surgery in the (A) toric and (B) LRI groups. Toric group, toric foldable iris-fixated phakic intraocular lens implantation; LRI group, non-toric foldable iris-fixated phakic intraocular lens implantation with limbal relaxing incisions; D, diopters.

Fig. 3
Scatter plots of the J0 and J45 vectors [in diopters (D)], calculated by power vector analysis, in the (A) toric and (B) LRI groups. Black diamonds and grey squares indicate preoperative and 6-month postoperative values, respectively. Toric group, toric foldable iris-fixated phakic intraocular lens implantation; LRI group, non-toric foldable iris-fixated phakic intraocular lens implantation with limbal relaxing incisions.

Fig. 4
Relationship between the target-induced astigmatism vector and the surgically induced astigmatism vector in the (A) toric and (B) LRI groups. The dashed line represents the ideal situation, in which the intended and achieved cylindrical corrections are equal. Toric group, toric foldable iris-fixated phakic intraocular lens implantation; LRI group, non-toric foldable iris-fixated phakic intraocular lens implantation with limbal relaxing incisions; D, diopters; TIA, target-induced astigmatism; SIA, surgically induced astigmatism.

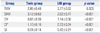
Table 1
Preoperative Demographic and Ocular Characteristics of the Subjects (n=146)

Toric group, toric foldable iris-fixated phakic intraocular lens implantation; LRI group, non-toric foldable iris-fixated phakic intraocular lens implantation with limbal relaxing incisions; LRI, limbal relaxing incision; D, diopters; ACD, anterior chamber depth; ECD, endothelial cell density.
Data are expressed as means±standard deviations unless indicated otherwise.
Table 2
Vector Analyses of Astigmatism at 6 Months Postoperatively
| Group | Toric group | LRI group | p value |
|---|---|---|---|
| TIAV | 2.85±0.48 | 2.77±0.53 | 0.303 |
| SIAV | 3.12±0.63 | 2.02±0.77 | <0.001 |
| DV | 0.67±0.39 | 1.14±0.56 | <0.001 |
| CI* | 1.10±0.16 | 0.72±0.24 | <0.001 |
| SI | 0.24±0.14 | 0.42±0.21 | <0.001 |
Toric group, toric foldable iris-fixated phakic intraocular lens implantation; LRI group, non-toric foldable iris-fixated phakic intraocular lens implantation with limbal relaxing incisions; LRI, limbal releasing incision; TIAV, target-induced astigmatism vector; SIAV, surgically induced astigmatism vector; DV, difference vector; CI, correction index (SIAV/TIAV); SI, success index (DV/TIAV).
Data are expressed as means±standard deviations.
*<1.0 indicates undercorrection and >1.0 indicates overcorrection.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download