Abstract
Recently, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) blood pressure (BP) trial enrolled 4733 participants with type 2 diabetes and randomized them to a target systolic blood pressure (SBP) of less than 120 mm Hg or 140 mm Hg. Despite the significant difference in the achieved SBP, there was no significant difference in the incidence of primary outcomes. Based on this evidence, the target SBP for diabetics has been revised in the majority of major guidelines. However, there is a steeper association between SBP and stroke in Asians than other ethnicities, with stroke being the leading cause of cardiovascular mortality. This suggests that target BP in the Asian region should be tailored towards prevention of stroke. In the ACCORD study, the intensive BP treatment was associated with significant reductions in both total stroke and non-fatal stroke. The results from the ACCORD study are supported by a subgroup analysis from the ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET) study, which showed that, in diabetic patients, the risk of stroke continues to decrease to a SBP value of 115 mm Hg with no evidence of J curve. As diabetes is highly associated with underlying coronary artery disease, there is a justified concern for adverse effects resulting from too much lowering of BP. In a post hoc analysis of 6400 diabetic subjects enrolled in the International Verapamil SR-Trandolapril (INVEST) study, subjects with SBP of less than 110 mm Hg were associated with a significant increase in all-cause mortality. In the ONTARGET study, at any levels of achieved SBP, diastolic blood pressure (DBP) below 67 mm Hg was associated with increased risk for cardiovascular outcomes. As such, a prudent approach would be to target a SBP of 130–140 mm Hg and DBP of above 60 mm Hg in diabetics with coronary artery disease. In conclusion, hypertension, in association with diabetes, has been found to be significantly correlated with an elevated risk for cardiovascular events. As the association between stroke and BP is stronger in Asians, compared to other ethnicities, consideration should be given for a target BP of 130/80 mm Hg in Asians.
Hypertension is a common comorbidity in diabetes and is a major risk factor for atherosclerotic cardiovascular disease and end-stage renal disease.1 Studies have shown that the majority of diabetics develop hypertension during their lifetime.23 In the Multiple Risk Factor Intervention Trial (MRFIT) study, a cohort of 347978 men aged 35–57 years followed up for an average of 12 years, the relative risk for cardiovascular death in diabetics, compared to non-diabetics, was increased by 1.89 to 4.40 for varying systolic blood pressure (SBP) levels.4 In a subgroup analysis of the ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET) study, diabetic patients had a significantly higher risk for primary endpoint [hazard ratio (HR): 1.48, 95% confidence interval (CI): 1.38–1.57], cardiovascular death (HR: 1.56, 95% CI: 1.42–1.71), myocardial infarction (HR: 1.30, 95% CI: 1.17–1.46), stroke (HR: 1.39, 95% CI: 1.23–1.56), and congestive heart failure hospitalization (HR: 2.06, 95% CI: 1.82–2.32).5 As such, adequate treatment of hypertension is essential to reduce the high burden of cardiovascular disease and end-stage renal disease in diabetics. Until recently, a target blood pressure (BP) of 130/80 mm Hg was endorsed by major guidelines, such as the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC) VII, and the European Society of Hypertension-European Society of Cardiology (ESH-ESC) guidelines.67 However, the results from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study have resulted in the revision of the target SBP to below 140 mm Hg according to ESH-ESC, JNC VIII, and the American Diabetes Association (ADA) guidelines.8910 In this minireview, we will discuss how recent changes in the guidelines may affect the target BP of diabetics in the Asian region.
The clinical evidence for supporting a previous target BP of 130/80 mm Hg was not based on results from an adequately powered, large-scale randomized study. Rather, the major supporting evidence came from subgroup analysis of the hypertension optimal treatment (HOT) study. The objective of the HOT study was to assess the relationship between cardiovascular events and three different diastolic blood pressures (DBPs) of ≤90 mm Hg, ≤85 mm Hg, and ≤80 mm Hg. Although the intensive treatment failed to reduce the incidence of major cardiovascular events in the entire 18790 study subjects, there was a 51% reduction in the incidence of major cardiovascular events among the 1501 patients who had diabetes at the onset of the study.11 Prior to the ACCORD, the only prospective study to achieve a mean BP below 130/80 mm Hg was the normotensive Appropriate Blood Pressure Control in NIDDM (ABCD) trial study. This study randomized 480 diabetics with baseline BP below 140/90 mm Hg to intensive (10 mm Hg below the baseline DBP, mean BP: 128±0.8/75±0.3 mm Hg) versus moderate (80–89 mm Hg of DBP, mean BP: 137±0.7/81±0.3 mm Hg) BP control. During a mean follow-up of 5.3 years, the intensive treatment arm was associated with slowed progression of diabetic nephropathy, slowed progression of diabetic retinopathy, and lower incidence of stroke.12 However, the normotensive ABCD study was a small study that did not have adequate power to determine whether or not intensive BP reduction is more beneficial than conventional treatment in reducing cardiovascular outcomes in diabetics. The lack of evidence for the benefit of intensive BP lowering was the basis for the ACCORD BP trial. The ACCORD BP trial enrolled 4733 participants with type 2 diabetes and randomized them to a target SBP of less than 120 mm Hg (after 1 year mean SBP: 119.3 mm Hg) or 140 mm Hg (after 1 year mean SBP: 133.5 mm Hg). Despite the significant difference in the achieved SBP, there was no significant difference in the incidence of primary outcome, defined as cardiovascular death, non fatal myocardial infarction, or non-fatal stroke (HR: 0.88, 95% CI: 0.73–1.06, p=0.20).13 The findings from the ACCORD study are supported by a post hoc analysis of the International Verapamil SR-Trandolapril Study (INVEST study) in which 6400 diabetics patients (28%) enrolled in the INVEST study were analyzed according to the achieved mean SBP. Patients were categorized as tight control (mean SBP <130 mm Hg), usual control (130 mm Hg≤ mean SBP<140 mm Hg), and uncontrolled (mean SBP ≥140 mm Hg). The results did not demonstrate any benefit of tight BP control compared to usual control in reducing primary outcome, defined as all-cause mortality, non-fatal myocardial infarction, or non fatal stroke.14 Based on this evidence, the target SBP for diabetics has been revised by the majority of major hypertension guidelines.8910
In the Asian region, the association between BP and cardiovascular disease differs, compared to other regions. In the Asia-Pacific Cohort Studies Collaboration, a total of 425325 study participants were followed up for 3 million person-years. The study showed a steeper association between SBP and stroke in Asians, compared to an Australasian cohort (Fig. 1).15 After standardizing for age, a 10 mm Hg lower SBP was associated with 41% lower stroke in Asia and 30% lower stroke risk in Australasia.15 Also, stroke was the leading cause of cardiovascular mortality in Asians, whereas ischemic heart disease was the leading cause of mortality in Australasians (Fig. 1).15 This suggests that target BP in the Asian region should be tailored towards prevention of stroke. In the aforementioned ACCORD study, the intensive BP treatment was associated with significant reduction in both total stroke (HR: 0.59, 95% CI: 0.39– 0.89, p=0.01) (Table 1) and non-fatal stroke (HR: 0.63, 95% CI: 0.41–0.96, p=0.03) (Table 1). Although stroke was a secondary endpoint in the ACCORD study, the results may still have clinical implications on the strong association of BP and stroke in the Asian region. The results from the ACCORD study are supported by a subgroup analysis from the ONTARGET study, which showed that, in diabetic patients, the risk of stroke continued to decrease to an achieved SBP value of 115 mm Hg with no evidence of a J curve.5 Achieving SBP below 130 mm Hg, instead of 140 mm Hg, was associated with a 31.4% reduction in stroke, which is in line with the results from the ACCORD trial. In a meta-analysis of 13 randomized clinical trials involving 37376 participants with either diabetes mellitus or impaired fasting glucose, intensive SBP control (≤130 mm Hg) was associated with a greater reduction in stroke, but not in other major cardiovascular events.16 Also, in the normotensive ABCD study, intensive BP lowering (mean BP: 128±0.8/75±0.3 mm Hg) was associated with a 69% reduction in stroke (p value=0.03).12 Although only a few randomized clinical outcome studies have been performed in the Asian region, some do support the application of a lower target SBP in diabetics. In the Challenge-DM study, a nationwide registry of 16869 Japanese patients followed up for 29 months, subjects with SBP ≥130 mm Hg exhibited a 48% increased risk in primary events (p<0.001), compared to subjects with SBP <130 mm Hg.17 In a subgroup analysis from the CASE-J study, the risk of cardiovascular events was the lowest at SBP of <130 mm Hg and a DBP between 75–79 mm Hg.18
Beyond prevention of stroke, intensive treatment of BP may be beneficial in subjects with diabetic nephropathy. In a post hoc analysis of the Renal Outcomes in the Irbesartan Diabetic Nephropathy Trial (IDNT), achieving SBP was a strong predictor of renal outcomes. Subjects with SBP >149 mm Hg were associated with a 2.2-fold increase in renal events, defined as doubling of serum creatinine or end stage renal disease (ESRD), compared to subjects with SBP <134 mm Hg.19 Progressive lowering of SBP to 120 mm Hg was associated with improved renal outcomes and lower mortality, suggesting that a target SBP of 130 mm Hg is justified in subjects with diabetic nephropathy.19
Diabetes is strongly associated with underlying coronary artery disease.22 As such, there is a real and justified concern for adverse effects resulting from too much lowering of BP. In the post hoc analysis of 6400 diabetic subjects enrolled in the INVEST study, subjects with a SBP of less than 110 mm Hg were associated with a significant increase in all-cause mortality (adjusted HR: 2.18, 95% CI: 1.17–4.09, p=0.02).14 This finding is supported by a post hoc analysis in the ONTARGET study. Excluding stroke, which did not show a J curve phenomenon, all other cardiovascular endpoints were associated with a nadir of SBP of 129.6 mm Hg in diabetics.5 Also, at any levels of achieved SBP, DBP of below 67 mm Hg was associated with increased risk for cardiovascular outcomes.5 However, it should be cautioned that the post-hoc analyses were limited by the lack of randomization, and the number of patients with low or very low achieved BP was quite small.20 As J curve might be a real concern in diabetics with coronary artery disease, a prudent approach would be to target a SBP of 130–140 mm Hg and a DBP above 60 mm Hg in diabetics with coronary artery disease. In diabetic subjects without any evidence of coronary artery disease, a SBP target of 130 mm Hg may be considered in the Asian region. In subjects with baseline SBP of less than 140 mm Hg, treatment may be associated with increased cardiovascular risk. In a meta-analysis of 73738 diabetic subjects by Brunström and Carlberg,23 treatment of BP in subjects with SBP of less than 140 mm Hg was associated with increased risk of cardiovascular mortality (HR: 1.15, 95% CI: 1.00–1.32) with a tendency towards an increased risk of all-cause mortality (HR: 1.05, 95% CI: 0.95–1.16). Therefore, anti-hypertensive treatment in diabetics should be started when BP is above 140/90 mm Hg. Although the initial target should be to lower the BP to below 140/90 mm Hg, a target SBP of 130 mm Hg may be considered in Asians and patients with diabetic nephropathy without prior history of coronary artery disease. However, it would be prudent to not lower the BP below 110/60 mm Hg.
Hypertension in diabetics is associated with a significantly elevated risk for cardiovascular events. Anti-hypertensive treatment should be started in all diabetics with a BP above 140/90 mm Hg to lower the BP below 140/90 mm Hg. As the association between stroke and BP is stronger in Asians than other ethnicities, consideration should be given for a target BP of 130/80 mm Hg in Asians. However, it would be prudent to not lower the BP below 110/60 mm Hg, especially in subjects with a history of coronary artery disease.
Figures and Tables
Fig. 1
Asia Pacific Cohort Studies Collaboration: the study analyzed a total of 425325 study participants who were followed up for 3 million person-years. The study showed a steeper association between SBP and stroke in Asians, compared to an Australasian cohort. Stroke was the leading cause of car-diovascular mortality in Asians, whereas ischemic heart disease was the leading cause of mortality in Australasians. Adapted from Lawes, et al. J Hypertens 2003;21:707-16, with permission of Wolters Kluwer Health Inc.15 CI, confidence interval; SBP, systolic blood pressure.

Table 1
Primary and Secondary Outcomes of Intensive Blood Pressure Control in Type 2 Diabetes Mellitus
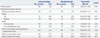
CI, confidence interval.
Adapted from ACCORD Study Group, et al. N Engl J Med 2010;362:1575-85, with permission of Massachusetts Medical Society.13
*The primary outcome was a composite of nonfatal myocardial infarction, nonfatal stroke, or death from cardiovascular causes, †Major coronary disease events, as defined in the protocol, included fatal coronary events, nonfatal myocardial infarction, and unstable angina.
ACKNOWLEDGEMENTS
This work was supported by a grant from the Korean Health Technology R&D Project, Ministry of Health & Welfare, Republic of Korea (HI13C0715)
References
1. Ravid M, Savin H, Lang R, Jutrin I, Shoshana L, Lishner M. Proteinuria, renal impairment, metabolic control, and blood pressure in type 2 diabetes mellitus. A 14-year follow-up report on 195 patients. Arch Intern Med. 1992; 152:1225–1229.

3. Lipman ML, Schiffrin EL. What is the ideal blood pressure goal for patients with diabetes mellitus and nephropathy? Curr Cardiol Rep. 2012; 14:651–659.

4. Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993; 16:434–444.

5. Redon J, Mancia G, Sleight P, Schumacher H, Gao P, Pogue J, et al. Safety and efficacy of low blood pressures among patients with diabetes: subgroup analyses from the ONTARGET (ONgoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial). J Am Coll Cardiol. 2012; 59:74–83.
6. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003; 289:2560–2572.

7. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2007; 28:1462–1536.
8. Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281–1357.
9. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520.

10. American Diabetes Association. Cardiovascular disease and risk management. Diabetes Care. 2016; 39:Suppl 1. S60–S71.
11. Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, et al. Effects of intensive blood-pressure lowering and lowdose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998; 351:1755–1762.

12. Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int. 2002; 61:1086–1097.

13. ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1575–1585.

14. Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010; 304:61–68.

15. Lawes CM, Rodgers A, Bennett DA, Parag V, Suh I, Ueshima H, et al. Blood pressure and cardiovascular disease in the Asia Pacific region. J Hypertens. 2003; 21:707–716.

16. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation. 2011; 123:2799–2810.

17. Kawamori R, Fujita T, Matsuoka H, Umemura S, Saito Y. Relation between cardiovascular complications and blood pressure/blood glucose control in diabetic patients with hypertension receiving long-term candesartan cilexetil therapy: challenge-DM study. Diabetes Res Clin Pract. 2009; 83:241–248.

18. Ogihara T, Saruta T, Rakugi H, Fujimoto A, Ueshima K, Yasuno S, et al. Relationship between the achieved blood pressure and the incidence of cardiovascular events in Japanese hypertensive patients with complications: a sub-analysis of the CASE-J trial. Hypertens Res. 2009; 32:248–254.

19. Pohl MA, Blumenthal S, Cordonnier DJ, De Alvaro F, Deferrari G, Eisner G, et al. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the irbesartan diabetic nephropathy trial: clinical implications and limitations. J Am Soc Nephrol. 2005; 16:3027–3037.

20. Chiang CE, Wang TD, Ueng KC, Lin TH, Yeh HI, Chen CY, et al. 2015 guidelines of the Taiwan Society of Cardiology and the Taiwan Hypertension Society for the management of hypertension. J Chin Med Assoc. 2015; 78:1–47.

21. Shimamoto K, Ando K, Fujita T, Hasebe N, Higaki J, Horiuchi M, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2014). Hypertens Res. 2014; 37:253–390.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download