Abstract
Mycoplasma hominis (M. hominis) and Ureaplasma urealyticum (U. urealyticum) are important opportunistic pathogens that cause urogenital infections and complicate pregnancy. The aim of this study was to investigate the prevalence, effects on pregnancy outcomes, and antimicrobial susceptibilities of M. hominis and U. urealyticum. We tested vaginal swabs obtained from 1035 pregnant women for the presence of genital mycoplasmas between June 2009 and May 2014. The laboratory and clinical aspects of genital mycoplasmas infection were reviewed retrospectively, and the identification and antimicrobial susceptibility of genital mycoplasmas were determined using the Mycoplasma IST-2 kit. A total of 571 instances of M. hominis and/or U. urealyticum were detected. Of them, M. hominis was detected in two specimens, whereas U. urealyticum was detected in 472 specimens. The remaining 97 specimens were positive for both M. hominis and U. urealyticum. Preterm deliveries were frequently observed in cases of mixed infection of M. hominis and U. urealyticum, and instances of preterm premature rupture of membrane were often found in cases of U. urealyticum. The rates of non-susceptible isolates to erythromycin, empirical agents for pregnant women, showed increasing trends. In conclusion, the prevalence of M. hominis and/or U. urealyticum infections in pregnant women is high, and the resistance rate of antimicrobial agents tends to increase. Therefore, to maintain a safe pregnancy, it is important to identify the isolates and use appropriate empirical antibiotics immediately.
Genital mycoplasmas including Mycoplasma hominis (M. hominis) and Ureaplasma urealyticum (U. urealyticum) are found in the vaginal milieu of 70–80% of sexually active women.1 Although most M. hominis and U. urealyticum infections are asymptomatic, these infections are associated with an increased risk of adverse pregnancy outcomes such as miscarriage, stillbirth, and preterm labor.23 M. hominis is specifically associated with conditions such as endometritis and preterm birth,23 while U. urealyticum can cause chorioamnionitis, spontaneous abortion, stillbirth, and preterm abortion during pregnancy.2
Tetracyclines and quinolones are the drugs of choice against genital mycoplasmas;456 however, macrolides are empirically used for pregnant women, as tetracyclines and quinolones are contraindicated in pregnancy.1 However, their therapeutic efficacy may be unpredictable due to increasing resistance.7 The rate of antimicrobial resistance varies geographically according to different antimicrobial therapy policies and history of prior use of antimicrobial agents.1 The aim of this study was to investigate the prevalence, effects on pregnancy outcomes, and antimicrobial susceptibilities of M. hominis and U. urealyticum in pregnant women.
We evaluated the genital mycoplasmas from a total of 1035 vaginal swabs from pregnant women aged 15–47 years who visited the department of obstetrics in Kyung Hee University Hospital at Gangdong between June 2009 and May 2014. Duplicate specimens from the same patients were excluded. Identification and antimicrobial susceptibilities of U. urealyticum and M. hominis were determined using a commercially available Mycoplasma IST-2 kit (bioMerieux, Marcy-l'Etoile, France), according to the manufacturer's instructions. All media and the inoculated strip were incubated at 37℃ in a CO2 incubator and observed for color changes, and the results were interpreted after 24 and 48 h of incubation. The A7 plates were examined with a microscope after 24 and 48 h of incubation, simultaneously. The kit was based on the principles of the biochemical properties of mycoplasmas. A change in the color of the medium from yellow to amaranth-purple for U. urealyticum was due to urea breakdown, and for M. hominis this change was due to arginine degradation. We decided to define culture-positive as when mycoplasmas were found using both the Mycoplasma IST-2 kit and A7 agar. Antimicrobial susceptibility tests performed using the Mycoplasma IST-2 kit included tetracycline, doxycycline, erythromycin, azithromycin, clarithromycin, josamycin, ofloxacin, ciprofloxacin, and pristinamycin. The breakpoints (mg/L) according to the Clinical and Laboratory Standards Institute were as follows: tetracycline S≤4, R≥8; doxycycline S≤4, R≥8; azithromycin S≤0.12, R≥4; clarithromycin S≤1, R≥4; erythromycin S≤1, R≥4; josamycin S≤2, R≥8; ciprofloxacin S≤1, R≥2; ofloxacin S≤1, R≥4; pristinamycin R≥2. Statistical analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Categorical variables were analyzed using a chi-square test and p-values of <0.05 were considered to be statistically significant.
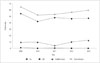
Of the 1035 specimens from pregnant women, the total positive rate of genital mycoplasmas infection was 55.2% (571 of 1035). Of the pregnant women with a positive culture for genital mycoplasmas, 472 (82.7%) had U. urealyticum only, two (0.3%) had M. hominis only, and 97 (17.0%) had both U. urealyticum and M. hominis. U. urealyticum infection (82.7%, 472 of 571) was much more prevalent than M. hominis infection. These findings are consistent with results recently reported in China;8 however, the total positive rate reported by the study from China was slightly higher than that reported in Korea.9 In our study, only two isolates were identified as a single M. hominis infection. Similarly, in a study including 96 pregnant African women, no cases were reported in which M. hominis was detected alone.1 In previous studies of patients with genital manifestation, the prevalence of single M. hominis infections (1.2%) was found to be higher than in our results (0.7%).810 Therefore, there is a possibility that U. urealyticum infections are found more frequently in patients having pelvic inflammatory disease than in asymptomatic pregnant women. The positive-culture rates of genital mycoplasmas by year are shown in Fig. 1. From 2011, the rate of positive culture for mixed infection of U. urealyticum and M. hominis showed an increasing trend.
The presence of M. hominis and U. urealyticum according to age group is shown in Table 1. The ages of pregnant women ranged from 15 to 47 years (median age 31 years). The positive rate of genital mycoplasmas for pregnant females aged 15–19 years old was the highest at 88.2% (15 of 17), and mixed infections were significantly higher (35.3%, 6 of 17) in the youngest group than in other age groups (Table 1). These findings represent a rapid increase of sexual activity in teenagers; thus, there should be greater concern regarding the maternal care of pregnant teenagers. Song, et al.8 reported similar results of high prevalence of infection in teenagers. For the oldest group (40–47 years), the rate of genital mycoplasma infection had a high value of 71.1% (27 of 38), and the infection rate of U. urealyticum was also high (65.8%, 25 of 38).
The incidence rates of adverse pregnancy outcomes are shown in Table 2. Of the 1035 pregnant women, 161 were diagnosed with preterm delivery, 336 with preterm labor, 199 with preterm premature rupture of membrane (PPROM), 26 with missed abortion, and 313 with normal pregnancy conditions. Certain pathological conditions occurred more frequently depending on which genital mycoplasmas the patients were infected with. The incidence of preterm delivery in women with infection of both U. urealyticum and M. hominis was 20.6% (20 of 97). This rate was relatively higher than that of women with infection of U. urealyticum only (15.3%, 72 of 472) and that of women who were negative for Mycoplasmas (14.6%, 68 of 464). Furthermore, the Mycoplasma IST-2 kit offered counts of genital mycoplasmas as less than or more than 104 CFU/mL, and we analyzed the differences in the incidence of preterm delivery according to the number of bacteria among the patients infected with both U. urealyticum and M. hominis. The incidence rates of preterm delivery were as follows: both M. hominis and U. urealyticum <104 CFU/mL (0 of 7, 0.0%); M. hominis <104 CFU/mL and U. urealyticum ≥104 CFU/mL (15 of 62, 19.5%); and both M. hominis and U. urealyticum ≥104 CFU/mL (5 of 8, 38.5%). There were no cases in which the number of M. hominis was more than 104 CFU/mL and that of U. urealyticum was less than 104 CFU/mL. We found that the occurrence of preterm delivery was related to the number of mycoplasmas in mixed infection (p<0.044). For the incidence of PPROM, 21.2% (100 of 472) of women were positive for U. urealyticum only, 12.4% (12 of 97) were positive for both U. urealyticum and M. hominis, and 18.8% (87 of 464) were negative for genital mycoplasmas. There were no significant differences in the incidence of still birth among all groups. In many studies, these microorganisms have been reported to cause adverse pregnancy outcomes, such as preterm labor, stillbirth, and chorioamnionitis.1112 On the other hand, they can be merely a part of normal genital flora, which makes the association of genital mycoplasmas with adverse pregnancy outcomes incomplete and confusing.12 Furthermore, the mechanism of how genital mycoplasma infections affect pregnancy has not been clearly identified. Only the identification of microbial stimuli causing inflammatory reactions in the gravid uterus, which initiates a cascade of events leading to precipitous delivery, has been described.12 In a large prospective observational study, a significant correlation was found between preterm delivery and Ureaplasma colonization.13 However, Choi, et al.14 mentioned that despite a high prevalence of Ureaplasma colonization in preterm labor cases, the rate of preterm delivery did not reach statistical significance. One of the focal points of our study was the relationship between genital mycoplasma infections and adverse pregnancy outcomes. Preterm delivery tended to be high for mixed infections, and a close correlation was shown between the count of bacteria in mixed infections and preterm delivery.
Antimicrobial susceptibilities of genital mycoplasmas are shown in Table 3. Mycoplasmas are susceptible to agents that inhibit protein synthesis.15 Macrolides are often used empirically in pregnant women,9 as several agents are teratogens, such as tetracyclines and fluoroquinolones, which are the drugs of choice.1617 There was no resistance to doxycycline, josamycin, or pristinamycin for two isolates of M. hominis; however, they were all resistant to azithromycin, clarithromycin, and erythromycin. Most of the U. urealyticum isolates were susceptible to josamycin and pristinamycin. Susceptibilities of 86.0%, 75.2%, and 64.0% for U. urealyticum were found for clarithromycin, azithromycin, and erythromycin, respectively; conversely, U. urealyticum also showed low susceptibilities to ciprofloxacin (5.3%) and ofloxacin (19.1%). For mixed infections, our results showed a high level of resistance to most of the antibiotics except tetracycline. The reason for this pattern of antibiotic resistance could be explained by previous studies reporting that mixed isolates are attributed to M. hominis.1910 These studies reported that patterns of antimicrobial susceptibilities against mixed strains were similar to the patterns displayed by M. hominis.110 However, in our study, though the josamycin susceptibility rates for M. hominis and U. urealyticum isolates were 100% and 97.9%, respectively, the josamycin susceptibility rate of mixed isolates was only 49.2%. This means that antimicrobial susceptibility against mixed infections does not simply imply susceptibility to M. hominis isolates and that mixed infections generally have a higher level of resistance than single infections. Our results showed that josamycin and pristinamycin would be the first drugs of choice for empirical therapy in pregnant women. Erythromycin is the most commonly used antibiotic and can be administered to pregnant women. However, the rate of resistance and intermediate susceptibility of U. urealyticum have tended to increase recently (Fig. 2).
A limitation of this study was that there was no consideration for coinfections of pathogens other than mycoplasmas. As the study was retrospective, it was impossible to test more subjects. Moreover, there was a possibility of enrollment bias, as collecting data from a tertiary healthcare institution could have resulted in the inclusion of many pregnant women with severe pathological conditions.
In conclusion, the prevalence of genital mycoplasma infections in pregnant women is high, and the incidence tends to increase in patients of a younger age. These infections are often associated with adverse pregnancy outcomes, such as PPROM and preterm delivery. Therefore, to maintain a safe pregnancy, it is important to identify the isolates and use appropriate antibiotics immediately. Additionally, culture identification and antibiotic susceptibility tests should be used routinely in clinical laboratories.
Figures and Tables
Table 1
Distribution of M. hominis and U. urealyticum According to Age

Table 2
Numbers of Pathological Conditions in Symptomatic Pregnant Women

Table 3
Antimicrobial Susceptibilities (%) of M. hominis and U. urealyticum from Vaginal Swabs

M. hominis, Mycoplasma hominis; U. urealyticum, Ureaplasma urealyticum; S, susceptible; I, intermediate; R, resistant.
Results are n (%). The breakpoints (mg/L) according to the Clinical and Laboratory Standards Institute are as follows: tetracycline S≤4, R≥8; doxycycline S≤4, R≥8; azithromycin S≤0.12, R≥4; clarithromycin S≤1, R≥4; erythromycin S≤1, R≥4; josamycin S≤2, R≥8; ciprofloxacin S≤1, R≥2; ofloxacin S≤1, R≥4; pristinamycin R≥2.
References
1. Redelinghuys MJ, Ehlers MM, Dreyer AW, Lombaard HA, Kock MM. Antimicrobial susceptibility patterns of Ureaplasma species and Mycoplasma hominis in pregnant women. BMC Infect Dis. 2014; 14:171.

2. Stellrecht KA, Woron AM, Mishrik NG, Venezia RA. Comparison of multiplex PCR assay with culture for detection of genital mycoplasmas. J Clin Microbiol. 2004; 42:1528–1533.

3. Kataoka S, Yamada T, Chou K, Nishida R, Morikawa M, Minami M, et al. Association between preterm birth and vaginal colonization by mycoplasmas in early pregnancy. J Clin Microbiol. 2006; 44:51–55.

4. Arai S, Gohara Y, Kuwano K, Kawashima T. Antimycoplasmal activities of new quinolones, tetracyclines, and macrolides against Mycoplasma pneumoniae. Antimicrob Agents Chemother. 1992; 36:1322–1324.

5. Hannan PC. Comparative susceptibilities of various AIDS-associated and human urogenital tract mycoplasmas and strains of Mycoplasma pneumoniae to 10 classes of antimicrobial agent in vitro. J Med Microbiol. 1998; 47:1115–1122.

6. Kenny GE, Cartwright FD. Susceptibilities of Mycoplasma hominis and Ureaplasma urealyticum to two new quinolones, sparfloxacin and WIN 57273. Antimicrob Agents Chemother. 1991; 35:1515–1516.

7. Kenny GE, Cartwright FD. Susceptibilities of Mycoplasma hominis, M. pneumoniae, and Ureaplasma urealyticum to GAR-936, dalfopristin, dirithromycin, evernimicin, gatifloxacin, linezolid, moxifloxacin, quinupristin-dalfopristin, and telithromycin compared to their susceptibilities to reference macrolides, tetracyclines, and quinolones. Antimicrob Agents Chemother. 2001; 45:2604–2608.

8. Song T, Ye A, Xie X, Huang J, Ruan Z, Kong Y, et al. Epidemiological investigation and antimicrobial susceptibility analysis of ureaplasma species and Mycoplasma hominis in outpatients with genital manifestations. J Clin Pathol. 2014; 67:817–820.

9. Koh E, Kim S, Kim IS, Maeng KY, Lee S. Antimicrobial susceptibilities of Ureaplasma urealyticum and Mycoplasma hominis in pregnant women. Korean J Clin Microbiol. 2009; 12:159–162.

10. Wang QY, Li RH, Zheng LQ, Shang XH. Prevalence and antimicrobial susceptibility of Ureaplasma urealyticum and Mycoplasma hominis in female outpatients, 2009-2013. J Microbiol Immunol Infect. 2014; 07. 28. [Epub ahead of print]. DOI: 10.1016/j.jmii.2014.06.007.

11. Capoccia R, Greub G, Baud D. Ureaplasma urealyticum, Mycoplasma hominis and adverse pregnancy outcomes. Curr Opin Infect Dis. 2013; 26:231–240.

12. Larsen B, Hwang J. Mycoplasma, Ureaplasma, and adverse pregnancy outcomes: a fresh look. Infect Dis Obstet Gynecol. 2010; 2010:DOI: 10.1155/2010/521921.
13. Breugelmans M, Vancutsem E, Naessens A, Laubach M, Foulon W. Association of abnormal vaginal flora and Ureaplasma species as risk factors for preterm birth: a cohort study. Acta Obstet Gynecol Scand. 2010; 89:256–260.

14. Choi SJ, Park SD, Jang IH, Uh Y, Lee A. The prevalence of vaginal microorganisms in pregnant women with preterm labor and preterm birth. Ann Lab Med. 2012; 32:194–200.

15. Taylor-Robinson D. The role of mycoplasmas in pregnancy outcome. Best Pract Res Clin Obstet Gynaecol. 2007; 21:425–438.

16. Raynes Greenow CH, Roberts CL, Bell JC, Peat B, Gilbert GL, Parker S. Antibiotics for ureaplasma in the vagina in pregnancy. Cochrane Database Syst Rev. 2011; (9):CD003767.
17. Bébéar C, Kempf I. Antimicrobial therapy and antimicrobial resistance. In : Blanchard A, Browning GF, editors. Mycoplasmas: Pathogenesis, Molecular Biology, and Emerging Strategies for Control. Wymondham: Horizon Bioscience;2005. p. 535–568.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download