Abstract
Purpose
To systematically update evidence on the clinical efficacy and safety of robot-assisted radical prostatectomy (RARP) versus retropubic radical prostatectomy (RRP) in patients with prostate cancer.
Materials and Methods
Electronic databases, including ovidMEDLINE, ovidEMBASE, the Cochrane Library, KoreaMed, KMbase, and others, were searched, collecting data from January 1980 to August 2013. The quality of selected systematic reviews was assessed using the revised assessment of multiple systematic reviews and the modified Cochrane Risk of Bias tool for non-randomized studies.
Results
A total of 61 studies were included, including 38 from two previous systematic reviews rated as best available evidence and 23 additional studies that were more recent. There were no randomized controlled trials. Regarding safety, the risk of complications was lower for RARP than for RRP. Among functional outcomes, the risk of urinary incontinence was lower and potency rate was significantly higher for RARP than for RRP. Regarding oncologic outcomes, positive margin rates were comparable between groups, and although biochemical recurrence (BCR) rates were lower for RARP than for RRP, recurrence-free survival was similar after long-term follow up.
Conclusion
RARP might be favorable to RRP in regards to post-operative complications, peri-operative outcomes, and functional outcomes. Positive margin and BCR rates were comparable between the two procedures. As most of studies were of low quality, the results presented should be interpreted with caution, and further high quality studies controlling for selection, confounding, and selective reporting biases with longer-term follow-up are needed to determine the clinical efficacy and safety of RARP.
Abbou, et al. first performed robot-assisted radical prostatectomy (RARP) in 2000.1 Since then, the da Vinci Surgical System (Intuitive Surgical, Sunnyvale, CA, USA) has been used in South Korea to conduct various types of urological surgery including radical prostatectomy, partial nephrectomy, and radical cystectomy, beginning in 2005.2 Radical prostatectomy is considered the gold standard of surgical treatment.3 However, the demand for RARP has increased due to better defined surgical anatomy and improved surgical maneuverability.2 Thirty-six da Vinci robotic surgery platforms are currently in use throughout 30 hospitals in Korea. A total of 24207 (24337 cases) patients underwent robotic surgery from 2005 to 2012, and the average annual growth rate for robotic surgery was 51.4% from 2005 to 2011. One-third (33.7%) of all robotic surgeries in the world were RARP; this was the most commonly performed robotic procedure.4
In 2013, the Korean government announced plans to radically enhance health insurance coverage for major conditions including cancer. Robotic surgery to treat prostatic cancer was to be included in the discretionary benefits list by as early as 2015.5 However, its inclusion has been questioned by some, since the comparative effectiveness of robotic surgery remains unclear. In previous reviews of RARP versus retropubic radical prostatectomy (RRP), RARP yielded better peri-operative outcomes.67 However, the evidence suggesting that RARP is associated with a decrease in urinary incontinence, improved potency, and reduction in biochemical recurrence (BCR), compared to RRP is limited. This is because most publications had a high risk of bias and exhibited extensive patient heterogeneity. While some experts have argued that the extension of discretionary benefits to robotic surgery increases patient choice, others point out that, without scientific evaluation, expansion of coverage will undermine the National Health Insurance system because demand will explode.8
Accordingly, the aim of the present paper was to comprehensively review and update data on the efficacy and safety of RARP versus RRP in patients with prostate cancer.
Studies eligible for inclusion consisted of randomized controlled trials and prospective and retrospective cohort studies that compared RARP and RRP. A study was excluded if it did not report any outcome of interest (i.e., safety or functional and oncological outcomes).
We systematically reviewed recent research using techniques that evaluated comparative effectiveness, as suggested by the Agency for Healthcare Research and Quality.9
Existing systematic reviews and health technology assessment reports were identified by searching ovidMEDLINE, ovidEMBASE, the Cochrane Library, KoreaMed, RISS4U, KISS, KISTI, KMbase, and NDSL from January 1980 to August 2013. We used combinations of MeSH terms and the following phrases: exp Prostatic Neoplasms/or prostatic cancer, exp Robotics/ or exp Surgery; and Computer-Assisted/or robot*/or (da vinci or davinci) (Supplementary Table 1, only online). In addition, we scanned the reference lists of relevant reviews and reports by international health technology assessment agencies to ensure comprehensive data collection. We then searched for recent studies (published from January 2010 to September 2013), because two high-quality systematic reviews (HIQA10; Ramsay, et al.11) had only searched primary studies up to March 2011. We did not restrict publication language.
Two authors independently reviewed all titles and abstracts and retrieved full-texts of all studies potentially meeting inclusion criteria. If the reviewing authors disagreed, the conflict was resolved by discussion and consensus, or by consulting a third member of the review team. We used structured data extraction forms to gather pertinent information; this included characteristics of the country of publication, study design, study participants, interventions, comparisons, outcome measures, outcome definitions, follow-up durations, and results that were statistically significant. If information was unclear or missing, we contacted the original authors by e-mail.
Two reviewers independently assessed the risk of bias. Systematic reviews were evaluated using the Revised Assessment of Multiple Systematic Reviews (R-AMSTAR) tool,12 and non-randomized studies newly published after 2010 were evaluated using the modified Cochrane Risk of Bias tool.11 The modified RoB tool is composed of seven specific domains: random sequence generation (selection bias), allocation concealment (selection bias), controlling for confounding (selection bias), blinding (performance and detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias), and other sources of bias (regarding funding source). Any disagreement was resolved by discussion.
Meta-analysis was performed using Revman 5.2 and Comprehensive Meta-Analysis (CMA) version 2.0. For continuous outcomes, weighted mean differences or standardized mean difference and 95% confidence intervals (CIs) were calculated using the random-effects model of the Dersimonian-Laird method.13 Mantel-Haenszel risk ratios (M-H RRs), with 95% CIs, derived using a random effects model, were calculated if outcomes were dichotomous.14 Heterogeneity was assessed using the I2 and Q statistics. An I2>50% was considered to indicate substantial heterogeneity.15 With the Q statistic, heterogeneity was deemed to be significant if p<0.10. Publication bias was tested by Funnel plotting and using Egger's test.16
An overview of the study selection process is provided in Fig. 1. We used two existing systematic reviews on RARP in patients with prostate cancer as the best-available evidence, which included 38 studies. An additional twenty-three studies were included through new searches for updates. Finally, we evaluated 61 articles, none of which was a randomized controlled clinical trial (Supplementary Table 2, only online). In characteristic of the included studies, the average age of the participants ranged from late fifties to sixties, which were similar between the two procedures. Of the 61 studies, 14 reported significantly different pre-operative prostate-specific antigen (PSA) levels. Also, 22.9% of the included studies reported significantly higher clinical stages for RRP patients than for RARP patients.
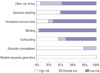
The summary of risk of bias in the cohort studies is shown in Fig. 2. In this evaluation, random sequence generation and concealment of allocation to group were considered to be important in terms of estimating any treatment effect. Most studies were flawed in this respect. Accordingly, most of the studies were susceptible to selection bias. Blinding domain was rated as a low risk of bias because of objective outcome measures or patient reported outcomes using valid and reliable questionnaires. In the selective outcome reporting domain, approximately 40% of the included studies were rated as having a high or unclear risk of bias, because those studies did not investigate all of the outcomes of interest in this review.
There was no significant difference in the rates of anastomosis site leakage (eight studies with 4880 participants; RR 0.78, 95% CI 0.47–1.28; p=0.330), infection (six studies with 7373 participants; RR 0.37, 95% CI 0.09–1.54; p=0.770), ileus (six studies with 2437 participants; RR 0.82, 95% CI 0.41–1.66; p=0.580), or deep vein thrombosis (five studies with 4576 participants; RR 0.75, 95% CI 0.39–1.46; p=0.400) between RARP and RRP in the selected studies (Supplementary Table 3, only online). However, RARP was associated with lower rates of bladder neck contracture (five studies with 2846 participants; RR 0.26, 95% CI 0.09–0.73; p=0.010), organ injury (ten studies with 6715 participants; RR 0.54, 95% CI 0.30–0.99; p=0.040), and pulmonary embolism (three studies with 3159 participants; RR 0.24, 95% CI 0.07–0.83; p=0.002), compared to RRP (Supplementary Fig. 1A, B, and C, respectively, only online). Transfusion data were reported in 25 studies (10605 participants). Although high degrees of study heterogeneity were evident, RARP was associated with a lower risk of transfusion than RRP in both prospective (12 studies with 6038 participants; RR 0.19, 95% CI 0.11–0.30; p<0.001) and retrospective studies (13 studies with 4567 participants; RR 0.14, 95% CI 0.07–0.30; p<0.001) (Supplementary Fig. 1D, only online).
Data from 19 studies (12175 participants) indicated a slight, but significant, difference in Clavien-Dindo complication rates after RARP, compared to RRP (RR 0.37, 95% CI 0.25–0.55, I2=84%; p<0.001). When complications were classified by severity, Clavien-Dindo I–II scores (11 studies with 5295 participants) and Clavien-Dindo III–V (8 studies with 6880 participants) scores suggested that RARP was associated with a decreased risk of Clavien-Dindo scores of I–II (RR 0.27, 95% CI 0.16–0.46, I2=88%; p<0.001) However, studies reporting such outcomes exhibited substantial heterogeneity (Supplementary Fig. 1E, only online).
RARP was associated with longer operating times than RRP (25 studies with 8080 participants; mean difference 32.27 min more; 95% CI: 12 to 52.54 min; p=0.002). Heterogeneity among study data was high (I2=98%) (Supplementary Fig. 1F, only online).
Hospital days were reported in 27 studies (7939 participants). Sub-group analysis was carried out by classifying countries into the US, Asia-Pacific, and Europe. RARP was associated with shorter hospital stay in the US (13 studies with 5112 participants; mean difference -0.66 days, 95% CI -1.19–-0.14; p=0.010), Asia-Pacific (five studies with 1256 participants; mean difference -3.39 days, 95% CI -4.11–-2.67; p<0.001), and Europe (nine studies with 1571 participants; mean difference -1.81 days, 95% CI -2.76–-0.86; p<0.001). Considerable heterogeneity was evident between studies (I2=99%), possibly attributable to differences in healthcare systems (Supplementary Fig. 1G, only online).
Based on the results of 11 studies (participants: 2510), RARP was associated with reduced urinary incontinence 12 months after surgery, compared to RRP (RR 0.62, 95% CI 0.42–0.93, I2=47%; p=0.020) (Fig. 3A). In order to consider differences in baseline characteristics of participants, subgroup analysis was performed. In 10 studies with a similar pre-operative PSA level between groups, urinary incontinence rate at 1 year after surgery was lower for RARP than for RRP (participants: 2214; RR 0.66, 95% CI 0.45–0.99, I2=45%; p=0.040). Also, pre-operative clinical stage for all of the studies was not significantly different between procedure groups.
Based on the results of 10 studies (participants: 2142), RARP was found to be associated with improved postoperative potency rate, compared to RRP (RR 1.41, 95% CI 1.18–1.70, I2=65%; p<0.001) (Fig. 3B). In addition, nine studies (participants: 1956) with a similar pre-operative PSA level between groups demonstrated favorable potency rate for RARP (RR 1.41, 95% CI 1.16–1.72, I2=63%; p<0.001). In eight studies (participants: 1965) with comparable pre-operative clinical stages between groups, RARP was associated with higher recovery of erectile function (RR 1.37, 95% CI 1.12–1.67, I2=69%; p=0.002).
Positive margin rates for RARP were equivalent to those for RRP in both prospective (13 studies, 6226 participants; RR 0.95, 95% CI 0.74–1.23, I2=80%; p=0.72) and retrospective studies (23 studies, 12813 participants; RR 0.88, 95% CI 0.75–1.03, I2=71%; p=0.110) (Fig. 4A). However, the heterogeneity among the results of individual studies was considerable. Sensitivity analysis was performed with only low risk studies (seven studies with 1412 participants; RR 0.93, 95% CI 0.67–1.30, I2=65%; p=0.670) (Fig. 4B) and for pT2 tumors in studies published after 2010 (7 studies with 2321 patients; RR 0.73, 95% CI 0.45–1.19, I2=73%; p=0.210) to determine the effect of removing any outliers. However, there was still moderate heterogeneity (Fig. 4C).
Fourteen studies (8259 participants) reported recurrence of prostate cancer, defined at various cut-off values of >0.4 ng/mL, >0.2 ng/mL, ≥2 ng/mL, >0.1 ng/mL, or ≥0.1 ng/mL. Therefore, the subgroup analysis was performed according to definition of PSA failure. Rates of BCR were reported in five studies (1485 participants) using the definition PSA level >0.2 ng/mL.1718192021 RARP was associated with a reduced risk of BCR, compared to RRP (RR 0.71, 95% CI 0.61–0.81, I2=0%; p<0.001) (Fig. 5A). Subgroup analysis according to follow-up duration demonstrated a similar recurrence-free survival between the two procedures upon long-term follow up (Fig. 5B).
Publication bias for each outcome was tested using Egger's regression test, and showed only one example of publication bias associated with reported transfusion rates (Supplementary Table 4, only online). So, trill and fill analysis was performed to adjust the publication bias. After excluding eight studies by trim-and-fill analysis, the risk ratio of transfusion rate was still lower in RARP than in RRP (RR 0.26, 95% CI 0.17–0.38).
To explore the supposed superiority of robotic platforms in treating prostate cancer, we performed a systematic review of all research published to 2013 that compared RARP with RRP. We found no randomized controlled study in which the two modalities were compared. Thus, we included only 61 non-randomized studies, of which 20 were prospective and 41 were retrospective. Studies were regarded as being of high quality if three of four domains (random sequence generation, confounding, blinding, and incomplete outcome reporting) were judged to have a low risk of bias. Only 13 (21.3%) publications met these criteria, and the risk of bias in most of the studies might confound the true effects of RARP.
Since 2010, 23 systematic reviews have been published, and they reported various outcomes. Our systematic review included recently published studies and reflects comprehensive primary outcomes, including perioperative outcomes, functional outcomes, and oncologic outcomes. Compared to open surgery, RARP yielded superior outcomes in terms of complications, such as organ injury, pulmonary embolism, and bladder neck contracture. In addition, the risk of overall complications assessed using the Clavien-Dindo classification was lower for RARP than RRP, although a high level of study heterogeneity was evident. Notably, the risk of complications after RARP was significantly lower than that after RRP, unlike earlier reports.711 Our findings are in line with results reported elsewhere. That is, a population-based observational cohort study using US Surveillance, Epidemiology, and End Results Medicare-linked data found that minimally invasive radical prostatectomy with or without robotic assistance was associated with lower rates of postoperative respiratory complications (4.3% vs. 6.6%; p=0.004), miscellaneous surgical complications (4.3% vs. 5.6%; p=0.03), and anastomotic stricture (5.8% vs. 14.0%; p<0.001), compared to RRP.22 In addition, RARP postoperative courses based on claims made to the South Korean Health Insurance Review and Assessment Service from September 2005 to December 2011 might be lower than RRP. Totals of 1830 and 1660 patients underwent RARP and RRP, respectively, and postoperative complication rates to 30 days as measured by re-admission to intensive care units were 0.1% and 0.2%, respectively.23 Thus, we suggest that RARP can be performed with a reasonably low complication rate.
In the present study, RARP was associated with better perioperative outcomes than RRP in terms of operation time and length of hospital stay, consistent with findings of previous systematic reviews and meta-analyses.724 In addition, claims data from South Korea showed that RARP-associated hospital stays were shorter than those for RRP (RARP 9 days vs. RRP 12.7 days). We sought to explore heterogeneity in pooled estimates of operative time by performing subgroup analysis according to the definition of operative time, but could not do so because most studies did not describe how they measured the duration of surgery. Only four studies reported durations of surgery as follows: from skin incision to skin closure time in both procedures;25 from insertion of the Veress needle (RARP) to the suture of the last laparoscopic port, and skin incision to suture (RRP);26 as the time from incision to placement of dressings;27 and as the mean operative time of hernia repair.28
Our results are comparable with those of a propensity-score matching study that adjusted for among-series differences in preoperative Gleason scores, preoperative PSA levels, and pathological stages. The cited work comprised a systematic review and meta-analysis of RRP, laparoscopic radical prostatectomy, and RARP patient series, and found that the rate of perioperative complications was significantly lower for RARP than RRP.24
The prevalence of urinary incontinence and erectile dysfunction after RARP are affected by preoperative patient characteristics (age, body mass index, and comorbidities), the experience of the surgeon, the surgical technique used, and methodological features, such as the definitions of continence and potency, outcome measures, and follow-up periods.29 To optimize our evaluation of functional outcomes, we included only outcome data obtained using objective measures or reliable and valid measurement instruments. In detail, the definition of continence was the use of no pad at all, 0–1 pads per day, or no leak measured by a validated questionnaire including the International Consultation of Incontinence Questionnaire-Urinary Incontinence; and that for erectile function a positive response to a validated questionnaire reporting erection sufficient for intercourse with or without prescription of a phosphodiesterase type 5 inhibitor or a score >17 on the Sexual Health Inventory for Men or 5-item version of the International Index of Erectile Function validated questionnaires exploring erectile dysfunction.
In this review, urinary incontinence and erectile function recovery rates measured at 12 months after RARP were lower than those after RRP. Our findings suggest positive functional outcomes of RARP, because of an increase of magnitude in effect size, compared to previous systematic review.11 The beneficial effects on the functional outcomes of RARP, compared to RRP, remained even in meta-analysis that added the study findings recently reported by Haglind, et al.30 [incontinence rate: 12 studies, 4937 participants, RR (M-H, random) 0.68, 95% CI 0.47–0.98, I2=62%; potency rate: 11 studies, 4564 participants, RR (M-H, random) 1.36, 95% CI 1.18–1.57, I2=61%].
The positive effect of functional outcomes of RARP is attributable to developments in surgical technique: nerve sparing improves both continence and potency, because the urethral rhabdosphincter receives afferent fibers from the traversing bundle.31 On robotic platforms, three-dimensional-magnified views allow meticulous dissection of both the periprostatic fascia layer and the neurovascular bundle. New insights into the multilayer structure of the periprostatic fascia and the course of the cavernous nerves have supported the development of intra- or inter-fascial surgical planes, enabling the urinary and sexual functional outcomes to be improved. Developments in RARP operative techniques improving urinary function, such as puboprostatic-sparing approaches, bladder neck preservation, selective dorsal vein complex division, nerve-sparing mechanisms, reconstruction of the posterior musculofascia, and anterior restoration of the pelvic space, are advocated. Meanwhile, several physician-reported studies showed incontinence rates ranging from 10 to 15% at 12 months after radical prostatectomy.3233 Considering that an acceptable incontinence rate is about 10%, regardless of the surgical technique, two studies included in this review might be performed by under-experienced surgeons due to a high incontinence rate, reaching 25 to 30%.3435 Urinary incontinence and erectile dysfunction are highly problematic conditions affecting many aspects of quality of life, and healthcare providers must be aware of this.363738 Although a randomized controlled study was not included in this review, our results suggest that healthcare providers should consider patient preferences in terms of recovery of urinary and erectile function when choosing between RARP and RRP, even though disparities in the receipt of RARP in terms of demographic characteristics, such as household income and insurance status, were reported.39
The rate of positive surgical margins was comparable between RARP and RRP (RR 0.95, 95% CI 0.74–1.23, I2=80%). In sensitivity analysis to explore the heterogeneity, our results did not change in the analysis restricted to studies rated as low risk of bias and for pT2 tumors studies published after 2010. The results were consistent with the findings of previous systematic reviews.22 Pooled estimates from 15 studies published from 2004 to 2011 showed that RARP is associated with a lower rate of positive surgical margins for pT2 tumors (RR 0.63, 95% CI 0.49–0.81, I2=27.7%).5 However, we suggest that our findings reflect more recent evidence of the comparative effectiveness of RARP versus RRP. Furthermore, this result was consistent with the recent cohort study investigating long-term oncologic outcomes, including positive surgical margins, in RARP compared to RRP (between group comparison p=0.230).40
In the present review, RARP was associated with a lower rate of BCR, compared to RRP, regardless of the manner in which such recurrence was defined (14 studies with 8259 patients; RR 0.71, 95% CI 0.54–0.93, I2=72%). To explore the effect of heterogeneity, we classified studies in terms of their definition of PSA failure, and selected PSA >0.2 ng/mL as an optimal criterion based on clinical practice guidelines.41 Upon subgroup analysis, RARP was superior to RRP in this context (five studies with 1485 patients; RR 0.71, 95% CI 0.61–0.81, I2=0%); heterogeneity was not an issue in this subgroup. This result is inconsistent with that of an earlier meta-analysis (hazard ratio 0.9, 95% CI 0.7–1.2, p=0.526), which reported differences in the definition of BCR-free survival.42 In additional analysis according to follow-up period, PSA failure rates were significantly lower in RARP than in RRP in a short term follow-up of 1 year or less. However, PSA failure rates between the two procedures were similar in long-term follow up.
Our present review had several limitations. First, significant oncologic and functional heterogeneity was evident; surgical skills and experience vary. Second, no randomized controlled trial has been conducted. Third, virtually no significant report on cancer-specific mortality rate following RARP has been published, because of the long follow-up needed in prognostic studies on clinically localized prostate cancer and the fact that RARP is a relatively new procedure.
In conclusion, we found that RARP might be favorable to RRP in aspects of post-operative complications, peri-operative outcomes, and functional outcomes, including urinary and erectile function. Also oncologic outcomes, such as positive margins and BCR, were comparable between two groups. However, most included studies were non-randomized studies and moderate to substantial heterogeneity was evident. Therefore, we suggest that further high quality studies minimizing selection, confounding, and selective reporting biases with longer-term follow-up are needed to determine clinical efficacy and safety of RARP.
Figures and Tables
 | Fig. 3Functional outcomes: RARP vs. RRP. (A) Incontinence rate at 12 months after surgery. (B) Potency rate at 12 months after surgery. RARP, robot-assisted radical prostatectomy; RRP, retropubic radical prostatectomy; CI, confidence interval |
 | Fig. 4Positive margin rate: RARP vs. RRP. (A) Positive margin rate. RARP, robot-assisted radical prostatectomy; RRP, retropubic radical prostatectomy; CI, confidence interval. (B) Positive margin rate of studies assessed as low risk studies. (C) Positive margin rate for pT2 tumors in studies published after 2010. RARP, robot-assisted radical prostatectomy; RRP, retropubic radical prostatectomy; CI, confidence interval |
 | Fig. 5Biochemical recurrence: RARP vs. RRP. (A) Biochemical recurrence according to definition of PSA failure. RARP, robot-assisted radical prostatectomy; RRP, retropubic radical prostatectomy; CI, confidence interval. (B) Biochemical recurrence according to follow-up duration. RARP, robot-assisted radical prostatectomy; RRP, retropubic radical prostatectomy; CI, confidence interval. |
ACKNOWLEDGEMENTS
This study was completed as part of the Health Technology Assessment Report (project no. NA 2013-007) funded by the National Evidence-based Healthcare Collaborating Agency in South Korea.
References
1. Yates DR, Vaessen C, Roupret M. From Leonardo to da Vinci: the history of robot-assisted surgery in urology. BJU Int. 2011; 108:1708–1713.

3. Heidenreich A, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V, et al. EAU guidelines on prostate cancer. Part 1: screening, diagnosis, and treatment of clinically localised disease. Eur Urol. 2011; 59:61–71.

4. Hakimi AA, Feder M, Ghavamian R. Minimally invasive approaches to prostate cancer: a review of the current literature. Urol J. 2007; 4:130–137.
5. Kang DC, Hardee MJ, Fesperman SF, Stoffs TL, Dahm P. Low quality of evidence for robot-assisted laparoscopic prostatectomy: results of a systematic review of the published literature. Eur Urol. 2010; 57:930–937.

6. Shin CM, Lee YJ, Suh HS, Jang BH, Park JE, Son HJ, et al. Safety and Effectiveness of Robot Surgery. Seoul: National Evidence-based Healthcare Collaborating Agency;2011.
7. Moran PS, O'Neill M, Teljeur C, Flattery M, Murphy LA, Smyth G, et al. Robot-assisted radical prostatectomy compared with open and laparoscopic approaches: a systematic review and meta-analysis. Int J Urol. 2013; 20:312–321.

8. Kim Y. Towards universal coverage: an evaluation of the benefit enhancement plan for four major conditions in Korean National Health Insurance. J Korean Med Assoc. 2014; 57:198–203.

9. Agency for Healthcare Research and Quality. Using existing systematic reviews to replace de novo processes in conducting comparative effectiveness reviews 2013. accessed on 2016 April 26. Available at: https://effectivehealthcare.ahrq.gov/repFiles/methodsguide/systematicreviewsreplacedenovo.pdf.
10. Health Information and Quality Authority. Health technology assessment of robot-assisted surgery in selected surgical procedures 2011. accessed on 2016 April 26. Available at: https://www.google.co.kr/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=0ahUKEwjm5pX4_KvMAhWBLKYKHftsALkQFggiMAA&url=https%3A%2F%2Fwww.hiqa.ie%2Fsystem%2Ffiles%2FHTA-robotassisted-surgery.pdf&usg=AFQjCNF33ID0LDoPAIIyxz8SEJprheEHZw&bvm=bv.120551593,d.dGo&cad=rjt.
11. Ramsay C, Pickard R, Robertson C, Close A, Vale L, Armstrong N, et al. Systematic review and economic modelling of the relative clinical benefit and cost-effectiveness of laparoscopic surgery and robotic surgery for removal of the prostate in men with localised prostate cancer. Health Technol Assess. 2012; 16:1–313.

12. Kung J, Chiappelli F, Cajulis OO, Avezova R, Kossan G, Chew L, et al. From systematic reviews to clinical recommendations for evidence-based health care: validation of revised assessment of multiple systematic reviews (R-AMSTAR) for grading of clinical relevance. Open Dent J. 2010; 4:84–91.

14. Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959; 22:719–748.
15. Schroll JB, Moustgaard R, Gøtzsche PC. Dealing with substantial heterogeneity in Cochrane reviews. Cross-sectional study. BMC Med Res Methodol. 2011; 11:22.

16. Egger M, Davey Smith G, Schneider M, Minder C. Bias in metaanalysis detected by a simple, graphical test. BMJ. 1997; 315:629–634.

17. Tewari A, Srivasatava A, Menon M; Members of the VIP Team. A prospective comparison of radical retropubic and robot-assisted prostatectomy: experience in one institution. BJU Int. 2003; 92:205–210.

18. Drouin SJ, Vaessen C, Hupertan V, Comperat E, Misraï V, Haertig A, et al. Comparison of mid-term carcinologic control obtained after open, laparoscopic, and robot-assisted radical prostatectomy for localized prostate cancer. World J Urol. 2009; 27:599–605.

19. Ou YC, Yang CR, Wang J, Cheng CL, Patel VR. Comparison of robotic-assisted versus retropubic radical prostatectomy performed by a single surgeon. Anticancer Res. 2009; 29:1637–1642.
20. Barocas DA, Salem S, Kordan Y, Herrell SD, Chang SS, Clark PE, et al. Robotic assisted laparoscopic prostatectomy versus radical retropubic prostatectomy for clinically localized prostate cancer: comparison of short-term biochemical recurrence-free survival. J Urol. 2010; 183:990–996.

21. Loeb S, Epstein JI, Ross AE, Schultz L, Humphreys EB, Jarow JP. Benign prostate glands at the bladder neck margin in robotic vs open radical prostatectomy. BJU Int. 2010; 105:1446–1449.

22. Hu JC, Gu X, Lipsitz SR, Barry MJ, D'Amico AV, Weinberg AC, et al. Comparative effectiveness of minimally invasive vs open radical prostatectomy. JAMA. 2009; 302:1557–1564.

23. Lee SH, Kim JH, Whang JS, Choi JE, Shin EH, Lee NR, et al. Clinical effectiveness and safety of robotic surgery. Seoul: National Evidence-based Healthcare Collaborating Agency;2014.
24. Novara G, Ficarra V, Rosen RC, Artibani W, Costello A, Eastham JA, et al. Systematic review and meta-analysis of perioperative outcomes and complications after robot-assisted radical prostatectomy. Eur Urol. 2012; 62:431–452.

25. Rocco B, Matei DV, Melegari S, Ospina JC, Mazzoleni F, Errico G, et al. Robotic vs open prostatectomy in a laparoscopically naive centre: a matched-pair analysis. BJU Int. 2009; 104:991–995.

26. Fracalanza S, Ficarra V, Cavalleri S, Galfano A, Novara G, Mangano A, et al. Is robotically assisted laparoscopic radical prostatectomy less invasive than retropubic radical prostatectomy? Results from a prospective, unrandomized, comparative study. BJU Int. 2008; 101:1145–1149.

27. Tomaszewski JJ, Matchett JC, Davies BJ, Jackman SV, Hrebinko RL, Nelson JB. Comparative hospital cost-analysis of open and robotic-assisted radical prostatectomy. Urology. 2012; 80:126–129.

28. Nakamura LY, Nunez RN, Castle EP, Andrews PE, Humphreys MR. Different approaches to an inguinal hernia repair during a simultaneous robot-assisted radical prostatectomy. J Endourol. 2011; 25:621–624.

29. Ficarra V, Novara G, Rosen RC, Artibani W, Carroll PR, Costello A, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol. 2012; 62:405–417.

30. Haglind E, Carlsson S, Stranne J, Wallerstedt A, Wilderäng U, Thorsteinsdottir T, et al. Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: a prospective, controlled, nonrandomised trial. Eur Urol. 2015; 68:216–225.

31. Costello AJ, Brooks M, Cole OJ. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int. 2004; 94:1071–1076.

32. McGlynn B, Al-Saffar N, Begg H, Gurun M, Hollins G, McPhee S, et al. Management of urinary incontinence following radical prostatectomy. Urol Nurs. 2004; 24:475–482. 515
33. Moore KN, Truong V, Estey E, Voaklander DC. Urinary incontinence after radical prostatectomy: can men at risk be identified preoperatively? J Wound Ostomy Continence Nurs. 2007; 34:270–279.
34. Iseki R, Ohori M, Hatano T, Tachibana M. [Urinary incontinence in early experience with robot-assisted laparoscopic prostatectomycomparison with radical retropubic prostatectomy]. Hinyokika Kiyo. 2012; 58:409–414.
35. Hohwü L, Borre M, Ehlers L, Venborg Pedersen K. A short-term cost-effectiveness study comparing robot-assisted laparoscopic and open retropubic radical prostatectomy. J Med Econ. 2011; 14:403–409.

36. Milsom I, Coyne KS, Nicholson S, Kvasz M, Chen CI, Wein AJ. Global prevalence and economic burden of urgency urinary incontinence: a systematic review. Eur Urol. 2014; 65:79–95.

37. Jannini EA, Sternbach N, Limoncin E, Ciocca G, Gravina GL, Tripodi F, et al. Health-related characteristics and unmet needs of men with erectile dysfunction: a survey in five European countries. J Sex Med. 2014; 11:40–50.

38. Tewari A, Sooriakumaran P, Bloch DA, Seshadri-Kreaden U, Hebert AE, Wiklund P. Positive surgical margin and perioperative complication rates of primary surgical treatments for prostate cancer: a systematic review and meta-analysis comparing retropubic, laparoscopic, and robotic prostatectomy. Eur Urol. 2012; 62:1–15.

39. Kim J, ElRayes W, Wilson F, Su D, Oleynikov D, Morien M, et al. Disparities in the receipt of robot-assisted radical prostatectomy: between-hospital and within-hospital analysis using 2009-2011 California inpatient data. BMJ Open. 2015; 5:e007409.

40. Jackson MA, Bellas N, Siegrist T, Haddock P, Staff I, Laudone V, et al. Experienced open vs early robotic-assisted laparoscopic radical prostatectomy: a 10-year prospective and retrospective comparison. Urology. 2016; 91:111–118.

41. Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 2014; 65:467–479.

42. Novara G, Ficarra V, Mocellin S, Ahlering TE, Carroll PR, Graefen M, et al. Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur Urol. 2012; 62:382–404.

43. Ahlering TE, Woo D, Eichel L, Lee DI, Edwards R, Skarecky DW. Robot-assisted versus open radical prostatectomy: a comparison of one surgeon's outcomes. Urology. 2004; 63:819–822.

44. Breyer BN, Davis CB, Cowan JE, Kane CJ, Carroll PR. Incidence of bladder neck contracture after robot-assisted laparoscopic and open radical prostatectomy. BJU Int. 2010; 106:1734–1738.

45. Choo MS, Choi WS, Cho SY, Ku JH, Kim HH, Kwak C. Impact of prostate volume on oncological and functional outcomes after radical prostatectomy: robot-assisted laparoscopic versus open retropubic. Korean J Urol. 2013; 54:15–21.

46. Coronato EE, Harmon JD, Ginsberg PC, Harkaway RC, Singh K, Braitman L, et al. A multi-institutional comparison of radical retropubic prostatectomy, radical perineal prostatectomy, and robotassisted laparoscopic prostatectomy for treatment of localized prostate cancer. J Robot Surg. 2009; 3:175–178.

47. Di Pierro GB, Baumeister P, Stucki P, Beatrice J, Danuser H, Mattei A. A prospective trial comparing consecutive series of open retropubic and robot-assisted laparoscopic radical prostatectomy in a centre with a limited caseload. Eur Urol. 2011; 59:1–6.

48. Doumerc N, Yuen C, Savdie R, Rahman MB, Rasiah KK, Pe Benito R, et al. Should experienced open prostatic surgeons convert to robotic surgery? The real learning curve for one surgeon over 3 years. BJU Int. 2010; 106:378–384.

49. Froehner M, Novotny V, Koch R, Leike S, Twelker L, Wirth MP. Perioperative complications after radical prostatectomy: open versus robot-assisted laparoscopic approach. Urol Int. 2013; 90:312–315.

50. Ham WS, Park SY, Kim WT, Koo KC, Lee YS, Choi YD. Open versus robotic radical prostatectomy: a prospective analysis based on a single surgeon's experience. J Robot Surg. 2008; 2:235–241.

51. Hong H, Mel L, Taylor J, Wu Q, Reeves H. Effects of robotic-assisted laparoscopic prostatectomy on surgical pathology specimens. Diagn Pathol. 2012; 7:24.

52. Kordan Y, Barocas DA, Altamar HO, Clark PE, Chang SS, Davis R, et al. Comparison of transfusion requirements between open and robotic-assisted laparoscopic radical prostatectomy. BJU Int. 2010; 106:1036–1040.

53. Krambeck AE, DiMarco DS, Rangel LJ, Bergstralh EJ, Myers RP, Blute ML, et al. Radical prostatectomy for prostatic adenocarcinoma: a matched comparison of open retropubic and robot-assisted techniques. BJU Int. 2009; 103:448–453.

54. Laurila TA, Huang W, Jarrard DF. Robotic-assisted laparoscopic and radical retropubic prostatectomy generate similar positive margin rates in low and intermediate risk patients. Urol Oncol. 2009; 27:529–533.

55. Lo KL, Ng CF, Lam CN, Hou SS, To KF, Yip SK. Short-term outcome of patients with robot-assisted versus open radical prostatectomy: for localised carcinoma of prostate. Hong Kong Med J. 2010; 16:31–35.
56. Ludovico GM, Dachille G, Pagliarulo G, D'Elia C, Mondaini N, Gacci M, et al. Bilateral nerve sparing robotic-assisted radical prostatectomy is associated with faster continence recovery but not with erectile function recovery compared with retropubic open prostatectomy: the need for accurate selection of patients. Oncol Rep. 2013; 29:2445–2450.

57. Magheli A, Gonzalgo ML, Su LM, Guzzo TJ, Netto G, Humphreys EB, et al. Impact of surgical technique (open vs laparoscopic vs robotic-assisted) on pathological and biochemical outcomes following radical prostatectomy: an analysis using propensity score matching. BJU Int. 2011; 107:1956–1962.

58. Nadler RB, Casey JT, Zhao LC, Navai N, Smith ZL, Zhumkhawala A, et al. Is the transition from open to robotic prostatectomy fair to your patients? A single-surgeon comparison with 2-year follow-up. J Robot Surg. 2010; 3:201–207.

59. Philippou P, Waine E, Rowe E. Robot-assisted laparoscopic prostatectomy versus open: comparison of the learning curve of a single surgeon. J Endourol. 2012; 26:1002–1008.

60. Punnen S, Meng MV, Cooperberg MR, Greene KL, Cowan JE, Carroll PR. How does robot-assisted radical prostatectomy (RARP) compare with open surgery in men with high-risk prostate cancer? BJU Int. 2013; 112:E314–E320.

61. Schroeck FR, Sun L, Freedland SJ, Albala DM, Mouraviev V, Polascik TJ, et al. Comparison of prostate-specific antigen recurrencefree survival in a contemporary cohort of patients undergoing either radical retropubic or robot-assisted laparoscopic radical prostatectomy. BJU Int. 2008; 102:28–32.

62. Silberstein JL, Su D, Glickman L, Kent M, Keren-Paz G, Vickers AJ, et al. A case-mix-adjusted comparison of early oncological outcomes of open and robotic prostatectomy performed by experienced high volume surgeons. BJU Int. 2013; 111:206–212.

63. Smith JA Jr, Chan RC, Chang SS, Herrell SD, Clark PE, Baumgartner R, et al. A comparison of the incidence and location of positive surgical margins in robotic assisted laparoscopic radical prostatectomy and open retropubic radical prostatectomy. J Urol. 2007; 178:2385–2389.

64. Uvin P, de Meyer JM, Van Holderbeke G. A comparison of the peri operative data after open radical retropubic prostatectomy or robotic-assisted laparoscopic prostatectomy. Acta Chir Belg. 2010; 110:313–316.

65. Wang R, Wood DP Jr, Hollenbeck BK, Li AY, He C, Montie JE, et al. Risk factors and quality of life for post-prostatectomy vesicourethral anastomotic stenoses. Urology. 2012; 79:449–457.

66. White MA, De Haan AP, Stephens DD, Maatman TK, Maatman TJ. Comparative analysis of surgical margins between radical retropubic prostatectomy and RALP: are patients sacrificed during initiation of robotics program? Urology. 2009; 73:567–571.

67. Williams SB, Chen MH, D'Amico AV, Weinberg AC, Kacker R, Hirsch MS, et al. Radical retropubic prostatectomy and robotic-assisted laparoscopic prostatectomy: likelihood of positive surgical margin(s). Urology. 2010; 76:1097–1101.

68. Wood DP, Schulte R, Dunn RL, Hollenbeck BK, Saur R, Wolf JS Jr, et al. Short-term health outcome differences between robotic and conventional radical prostatectomy. Urology. 2007; 70:945–949.

69. Ficarra V, Novara G, Fracalanza S, D'Elia C, Secco S, Iafrate M, et al. A prospective, non-randomized trial comparing robot-assisted laparoscopic and retropubic radical prostatectomy in one European institution. BJU Int. 2009; 104:534–539.

70. Kim SC, Song C, Kim W, Kang T, Park J, Jeong IG, et al. Factors determining functional outcomes after radical prostatectomy: robot-assisted versus retropubic. Eur Urol. 2011; 60:413–419.

71. Burgess SV, Atug F, Castle EP, Davis R, Thomas R. Cost analysis of radical retropubic, perineal, and robotic prostatectomy. J Endourol. 2006; 20:827–830.

72. D'Alonzo RC, Gan TJ, Moul JW, Albala DM, Polascik TJ, Robertson CN, et al. A retrospective comparison of anesthetic management of robot-assisted laparoscopic radical prostatectomy versus radical retropubic prostatectomy. J Clin Anesth. 2009; 21:322–328.
73. Durand X, Vaessen C, Bitker MO, Richard F. [Retropubic, laparoscopic and robot-assisted total prostatectomies: comparison of postoperative course and histological and functional results based on a series of 86 prostatectomies]. Prog Urol. 2008; 18:60–67.

74. Farnham SB, Webster TM, Herrell SD, Smith JA Jr. Intraoperative blood loss and transfusion requirements for robotic-assisted radical prostatectomy versus radical retropubic prostatectomy. Urology. 2006; 67:360–363.

75. Nelson B, Kaufman M, Broughton G, Cookson MS, Chang SS, Herrell SD, et al. Comparison of length of hospital stay between radical retropubic prostatectomy and robotic assisted laparoscopic prostatectomy. J Urol. 2007; 177:929–931.

76. Ball AJ, Gambill B, Fabrizio MD, Davis JW, Given RW, Lynch DF, et al. Prospective longitudinal comparative study of early healthrelated quality-of-life outcomes in patients undergoing surgical treatment for localized prostate cancer: a short-term evaluation of five approaches from a single institution. J Endourol. 2006; 20:723–731.

77. Bolenz C, Gupta A, Hotze T, Ho R, Cadeddu JA, Roehrborn CG, et al. Cost comparison of robotic, laparoscopic, and open radical prostatectomy for prostate cancer. Eur Urol. 2010; 57:453–458.

78. Bolenz C, Gupta A, Hotze T, Ho R, Cadeddu JA, Roehrborn CG, et al. The influence of body mass index on the cost of radical prostatectomy for prostate cancer. BJU Int. 2010; 106:1188–1193.

79. Carlsson S, Nilsson AE, Schumacher MC, Jonsson MN, Volz DS, Steineck G, et al. Surgery-related complications in 1253 robot-assisted and 485 open retropubic radical prostatectomies at the Karolinska University Hospital, Sweden. Urology. 2010; 75:1092–1097.

80. Chan RC, Barocas DA, Chang SS, Herrell SD, Clark PE, Baumgartner R, et al. Effect of a large prostate gland on open and robotically assisted laparoscopic radical prostatectomy. BJU Int. 2008; 101:1140–1144.

81. Malcolm JB, Fabrizio MD, Barone BB, Given RW, Lance RS, Lynch DF, et al. Quality of life after open or robotic prostatectomy, cryoablation or brachytherapy for localized prostate cancer. J Urol. 2010; 183:1822–1828.

82. Miller J, Smith A, Kouba E, Wallen E, Pruthi RS. Prospective evaluation of short-term impact and recovery of health related quality of life in men undergoing robotic assisted laparoscopic radical prostatectomy versus open radical prostatectomy. J Urol. 2007; 178(3 Pt 1):854–858.

83. Truesdale MD, Lee DJ, Cheetham PJ, Hruby GW, Turk AT, Badani KK. Assessment of lymph node yield after pelvic lymph node dissection in men with prostate cancer: a comparison between robotassisted radical prostatectomy and open radical prostatectomy in the modern era. J Endourol. 2010; 24:1055–1060.

84. Choi D, Kim D, Kyung YS, Lim JH, Song SH, You D, et al. Clinical experience with limited lymph node dissection for prostate cancer in Korea: single center comparison of 247 open and 354 robotassisted laparoscopic radical prostatectomy series. Korean J Urol. 2012; 53:755–760.

85. Gainsburg DM, Wax D, Reich DL, Carlucci JR, Samadi DB. Intraoperative management of robotic-assisted versus open radical prostatectomy. JSLS. 2010; 14:1–5.

86. Lallas CD, Pe ML, Thumar AB, Chandrasekar T, Lee FC, McCue P, et al. Comparison of lymph node yield in robot-assisted laparoscopic prostatectomy with that in open radical retropubic prostatectomy. BJU Int. 2011; 107:1136–1140.

87. Martinschek A, Heinzelmann K, Ritter M, Heinrich E, Trojan L. Radical prostatectomy after previous transurethral resection of the prostate: robot-assisted laparoscopic versus open radical prostatectomy in a matched-pair analysis. J Endourol. 2012; 26:1136–1141.

88. Minniti D, Chiadò Piat S, Di Novi C. Robot-assisted versus open radical prostatectomy: an evidence-based comparison. Technol Health Care. 2011; 19:331–339.

89. Mirza M, Art K, Wineland L, Tawfik O, Thrasher JB. A comparison of radical perineal, radical retropubic, and robot-assisted laparoscopic prostatectomies in a single surgeon series. Prostate Cancer. 2011; 2011:878323.

90. Na HS, Kim HY, Do SH, Jeon YT, Hwang JW, Oh AY. Review of anesthesia for robotic-assisted radical prostatectomy: in comparison with radical retropubic prostatectomy. Anesth Pain Med. 2009; 4:364–367.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download