Abstract
Purpose
Despite new treatment strategies, anemia remains the most prevalent complication in patients with end-stage renal disease (ESRD). We investigated whether 25-hydroxyvitamin D [25(OH)D3] deficiency was associated with anemia in ESRD patients.
Materials and Methods
We reviewed the medical records of 410 ESRD patients who had undergone renal transplantation (RTx) at Yonsei University Health System and who had 25(OH)D3 levels measured at the time of RTx. Patients were divided into two groups based on baseline 25(OH)D3 concentrations: group 1, 25(OH)D3 levels <10 ng/mL; and group 2, 25(OH)D3 levels ≥10 ng/mL.
Results
Using multivariate regression models, 25(OH)D3, age, and erythrocyte-stimulating agent (ESA) dose were found to be significantly associated with hemoglobin (Hb) levels [25(OH)D3: β=0.263, p<0.001; age: β=0.122, p=0.010; ESA dose: β=-0.069, p=0.005]. In addition, logistic regression analysis revealed that patients in group 1 had a significantly higher risk for developing anemia (Hb level <10 g/dL) compared to group 2 patients, even after adjusting for potential risk factors for anemia (odds ratio=3.857; confidence interval=1.091–13.632; p=0.036).
Anemia is a common finding in patients with chronic kidney disease (CKD), and its prevalence and severity are known to increase as renal function decreases. In addition, anemia is closely associated with a wide range of clinical symptoms and signs, resulting in poor quality of life and increased risk of morbidity and mortality in these patients.12345
Recently, accumulating evidence indicates that vitamin D has pleiotropic effects in various organ systems based on the distribution of vitamin D receptors in the whole body.6 In addition to its well-known effects on bone and mineral metabolism, vitamin D has been revealed to play a protective role in a number of chronic diseases, including CKD-associated anemia.7 In fact, previous studies using data from the Study to Evaluate Early Kidney Disease and the Third National Health and Nutrition Examination Survey showed that vitamin D deficiency was significantly and independently associated with anemia in patients with CKD who not require dialysis.89 However, the relationship between serum 25-hydroxyvitamin D [25(OH)D3] and hemoglobin (Hb) concentrations has not been extensively explored in patients with end-stage renal disease (ESRD).
In this study, we attempted to elucidate the correlation of 25(OH)D3 with anemia in relatively healthy patients with ESRD who were admitted to the hospital for renal transplantation (RTx). Moreover, the independent impact of 25(OH)D3 on anemia was clarified in these patients.
We reviewed the medical records of 423 patients with ESRD who had undergone RTx at Yonsei University Health System in Seoul, Korea (latitude: 37.5°N; average annual sunshine: 5.8 hours per day) between April 2002 and December 2008 and whose 25(OH)D3 levels were measured at the next date of hospital admission for RTx (about 1–2 weeks before RTx). Among these patients, 13 were excluded for being less than 18 years old (n=6) or more than 70 years old (n=7). Thus, the final analysis involved 410 RTx patients. No patients with acute illness were included in the current study. All participants were from an ethnically homogeneous Korean population.
This study was approved by the Institutional Review Board (IRB) of Yonsei University Health System Clinical Trial Center (IRB No. 4-2014-0447). All patients who participated in the current study were aware of this investigation. However, as the present study was a retrospective medical record-based study and the study subjects were de-identified, the IRB waived the need for written consent from the patients.
Although 1,25(OH)2D3 is the active form of vitamin D, its halflife is only 4–6 hours in circulation. In the clinical field, therefore, 25(OH)D3 is regarded as the best index to assess vitamin D status due to its long half-life of approximately 3 weeks.10 The serum 25(OH)D3 concentrations were determined at the time of RTx via a radioimmunoassay method using the 25-HYDROXYVITAMIN D 125I RIA KIT (68100E; DiaSorin Inc., Stillwater, MN, USA).11 According to the opinion of most experts, vitamin D deficiency is defined as serum 25(OH)D3 levels <10 ng/mL (25 nmol/L), vitamin D insufficiency as 25(OH)D3 levels of 10–29 ng/mL (25–72 nmol/L), and vitamin D sufficiency as 25(OH)D3 levels ≥30 ng/mL (73 nmol/L).10121314151617 As there were no patients with vitamin D sufficiency, the patients were divided into two groups for analysis: group 1, 25(OH)D3 <10 ng/mL and group 2, 25(OH)D3 ≥10 ng/mL.
Demographic and clinical data at the time of RTx were recorded, including age, sex, dialysis modality before RTx, duration of dialysis, comorbidities, season at the time of RTx, and erythrocyte-stimulating agent (ESA) dose. To further study the association between 25(OH)D3 levels and ESA requirements, the ESA dose/Hb index was calculated by dividing the monthly ESA dose (units) by the Hb concentration. The results of the following biochemical laboratory tests were also collected: Hb, intact parathyroid hormone (iPTH), serum iron, total iron-binding capacity (TIBC), transferrin saturation (TSAT), ferritin, alkaline phosphatase (ALP), serum phosphate, calcium, albumin, estimated glomerular filtration rate (eGFR), and high-sensitivity C-reactive protein (hs-CRP) levels.
Statistical analysis was performed using SPSS version 20.0 (SPSS Inc., Chicago, IL, USA). Continuous variables are expressed as mean±standard deviation or median±interquartile range for skewed data. The Kolmogorov-Smirnov test was used to analyze the normality of the distribution of measured parameters, and categorical variables are presented as a number (percentage). The patients were divided into two groups based on serum 25(OH)D3 concentrations (<10 ng/mL and ≥10 ng/mL). The differences between the two groups were determined using Student's t test or the Mann-Whitney U test for continuous variables and the chi-square test for categorical variables. The relationship between Hb and 25(OH)D3 levels was assessed using Pearson's correlation analysis. Univariate and multivariate linear regression analyses were also performed to determine the independent correlates of anemia. A logistic regression analysis was used to estimate odds ratios (OR) and to identify independent risk factors for anemia. The National Kidney Foundation-Kidney Disease Outcomes Quality Initiative (NKF-KDOQI) guidelines (2012) recommended that Hb targets should be in the range of 10.0–11.5 g/dL, regardless of whether the patients were receiving dialysis.18 Therefore, we defined anemia as an Hb level of <10 g/dL. In all cases, a p-value of <0.05 was considered to be statistically significant.
Demographic, clinical, and biochemical data are shown in Table 1. The mean age was 40.7±11.4 years, and 262 patients (63.9%) were male. The mean serum 25(OH)D3 concentration was 11.1±6.4 ng/mL, while the mean 25(OH)D3 level was 6.5±1.8 ng/mL in group 1 and 17.2±5.6 ng/mL in group 2. There were no differences in age, dialysis modality, season at the time of RTx, and comorbidities between the two groups. However, the following factors were significantly different between the two groups. Group 2 had a higher proportion of men than group 1 (69.9%; p=0.003). The proportion of patients who met the criteria for anemia (60.2%; p<0.001) and ESA use (53.8%; p=0.013) was significantly higher in group 1. Moreover, the monthly ESA dose was significantly higher in group 1 (20656.2±17627.7; p=0.003).
As seen in Table 1, serum phosphate, calcium, and albumin concentrations were significantly lower in group 1 than in group 2. In contrast, there were no significant differences in serum levels of iPTH, serum iron, TIBC, TSAT, ferritin, ALP, eGFR, and hs-CRP.
On univariate linear regression analysis, Hb concentration was found to be significantly correlated with serum 25(OH)D3 level (β=0.292; p<0.001), age (β=0.147; p=0.003), ESA dose (β=-0.177; p<0.001), and log iPTH (β=-0.102; p=0.039). The associations between Hb concentration and serum 25(OH)D3 level (β=0.263; p<0.001), age (β=0.122; p=0.010), and ESA dose (β=-0.069; p=0.005) remained significant on multivariate linear regression analysis (Table 2). Serum 25(OH)D3 concentration was also significantly associated with ESA resistance, assessed by the ESA dose/Hb index, on both univariate analysis (β=-0.176; p<0.001) and multivariate analysis (β=-0.047; p<0.001) (Table 3).
Pearson's correlation analysis revealed a significant correlation between 25(OH)D3 and Hb levels (r=0.292; p<0.001). Hb level also significantly correlated with albumin (r=0.267; p<0.001) and calcium levels (r=0.309; p=0.040).
Pearson's correlation analysis revealed a significant negative correlation between ESA dose/Hb index and 25(OH)D3 level (r=-0.176; p<0.001). ESA dose/Hb level also negatively correlated with Hb (r=-0.329; p<0.001), albumin (r=-0.172; p<0.001), and calcium levels (r=-0.099; p=0.046).
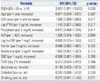
Logistic regression analysis revealed that patients in group 1 had a significantly higher risk for developing anemia than group 2 patients, even after adjusting for age, ESA dose, log iPTH, phosphate, ALP, log hs-CRP, ferritin, serum iron, TIBC, TSAT levels, sex, diabetes, and smoking [OR=3.857; 95% confidence interval (CI)=1.091–13.632; p=0.036] (Table 4).
Previous studies have demonstrated the association of serum vitamin D and Hb levels in patients with CKD who do not require dialysis;819 however, the impact of vitamin D deficiency on anemia has not been extensively explored in patients with ESRD.
In this study, we demonstrated that patients with 25(OH)D3 levels <10 ng/dL had a higher risk of developing anemia than patients with 25(OH)D3 levels ≥10 ng/dL. This association remained significant even after adjusting for potentially important risk factors for anemia. These findings are of great clinical significance, as anemia is very common in CKD patients and is associated with negative clinical outcomes.202122 The NKF-KDOQI guidelines (2012) recommended 10 g/dL as the lowest Hb level in CKD patients.18 Hb levels <10 g/dL can increase the need for transfusion and the risks of cardiovascular complications and mortality in CKD patients.2324 Several factors or medical comorbidities have been identified as risk factors for anemia. Based on our data, we suggest that vitamin D deficiency, a modifiable condition, could be an additional risk factor for anemia in ESRD patients.
Several potential mechanisms could explain the association between vitamin D deficiency and anemia in ESRD patients. Several studies have found that vitamin D exerts a direct stimulatory action on erythroid precursor cells in CKD patients. The burst-forming unit-erythroid (BFU-E) assay revealed that combined low doses of erythropoietin and vitamin D significantly increased proliferation of mononuclear cells isolated from the peripheral blood of patients with CKD compared to low-dose erythropoietin alone.25 Moreover, BFU-E proliferation was further potentiated by high-dose vitamin D,26 although this was not observed with cells isolated from healthy subjects. Taken together, these findings suggest that vitamin D has a direct effect on erythroid precursor proliferation in CKD patients yet not in patients with normal renal function.
In addition, there is growing evidence that inflammatory cytokines influence erythropoiesis in CKD patients.27 Moreover, vitamin D deficiency was associated with secondary hyperparathyroidism, which is known to induce bone marrow fibrosis and suppress erythropoiesis in CKD patients.28 Taken together, vitamin D seems to be involved in erythropoiesis in multiple ways in CKD patients, including directly stimulating the proliferation of erythropoietic cells, improving iron availability by inhibiting inflammatory cytokines and hepcidin production, and suppressing parathyroid hormone concentrations.
In this study, vitamin D deficiency was found to be an independent risk factor for anemia in patients with ESRD, which is in agreement with the results of most previous studies of patients with early CKD and patients undergoing hemodialysis. Although no significant differences in serum hs-CRP and iPTH levels were found with respect to vitamin D deficiency, the concentrations of both were lower in patients with vitamin D deficiency. Furthermore, Pearson's correlation analysis revealed no relationships between Hb levels and serum hs-CRP, iPTH, or iron levels. Based on these findings, it seems likely that the weak association between inflammation, hyperparathyroidism, and iron profiles with anemia in the present study was the result of our patients being relatively healthy and stable with minimal inflammation, acceptably controlled secondary hyperparathyroidism, and a good nutritional status.
This study had several limitations. First, the number of patients was relatively small. Second, as the study subjects were all Korean patients with ESRD, the associations of vitamin D with anemia and erythropoietin resistance may not be generalizable to other populations. Finally, serum vitamin D concentrations were measured only once at the time of RTx; therefore, it was difficult to conclusively determine whether the changes in serum vitamin D levels had any influence on the changes in Hb concentrations and erythropoietin resistance.
In conclusion, vitamin D deficiency was prevalent in patients with ESRD undergoing RTx and was found to be independently associated with anemia and erythropoietin resistance. Further studies will be needed to verify the association of vitamin D deficiency with anemia and erythropoietin resistance by evaluating the effect of vitamin D replacement in patients with ESRD.
Figures and Tables
Table 1
Baseline Characteristics of Patients According to 25(OH)D3 Levels

25(OH)D3, 25-hydroxyvitamin D; Hb, hemoglobin; RTx, renal transplantation; IV, intravenous; ESA, erythrocyte stimulating agent; iPTH, intact parathyroid hormone; TIBC, total iron binding capacity; TSAT, transferrin saturation; ALP, alkaline phosphatase; eGFR, estimated glomerular filtration rate; hs-CRP, high-sensitivity C-reactive protein.
Results are expressed as mean±standard deviation, median±interquartile range, or n (%).
Table 2
Associations between Hb and Clinical/Biochemical Parameters
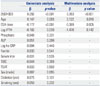
Table 3
Associations between ESA Dose/Hb Index and Clinical/Biochemical Parameters
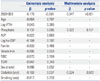
Table 4
Risk Factors for Developing Anemia (Hb <10 g/dL)
References
1. Astor BC, Muntner P, Levin A, Eustace JA, Coresh J. Association of kidney function with anemia: the Third National Health and Nutrition Examination Survey (1988-1994). Arch Intern Med. 2002; 162:1401–1408.
2. Golbahar J, Altayab D, Carreon E, Darwish A. Association of vitamin D deficiency and hyperparathyroidism with anemia: a crosssectional study. J Blood Med. 2013; 4:123–128.

4. Wojcicki JM. Hyperphosphatemia is associated with anemia in adults without chronic kidney disease: results from the National Health and Nutrition Examination Survey (NHANES): 2005-2010. BMC Nephrol. 2013; 14:178.

5. Shimizu Y, Nakazato M, Sekita T, Kadota K, Sato S, Arima K, et al. Association between alkaline phosphatase and anemia in rural Japanese men: The Nagasaki Islands study. Acta Medica Nagasakiensia. 2014; 58:125–130.
6. Icardi A, Paoletti E, De Nicola L, Mazzaferro S, Russo R, Cozzolino M. Renal anaemia and EPO hyporesponsiveness associated with vitamin D deficiency: the potential role of inflammation. Nephrol Dial Transplant. 2013; 28:1672–1679.

7. Besarab A, Coyne DW. Iron supplementation to treat anemia in patients with chronic kidney disease. Nat Rev Nephrol. 2010; 6:699–710.

8. Patel NM, Gutiérrez OM, Andress DL, Coyne DW, Levin A, Wolf M. Vitamin D deficiency and anemia in early chronic kidney disease. Kidney Int. 2010; 77:715–720.

9. Kendrick J, Targher G, Smits G, Chonchol M. 25-Hydroxyvitamin D deficiency and inflammation and their association with hemoglobin levels in chronic kidney disease. Am J Nephrol. 2009; 30:64–72.

10. Yoo EH, Cho HJ. Prevalence of 25-hydroxyvitamin D deficiency in Korean patients with anemia. J Clin Lab Anal. 2015; 29:129–134.

11. Hollis BW, Kamerud JQ, Selvaag SR, Lorenz JD, Napoli JL. Determination of vitamin D status by radioimmunoassay with an 125I-labeled tracer. Clin Chem. 1993; 39:529–533.

13. Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006; 81:353–373.

14. Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006; 84:18–28.

15. Thomas MK, Lloyd-Jones DM, Thadhani RI, Shaw AC, Deraska DJ, Kitch BT, et al. Hypovitaminosis D in medical inpatients. N Engl J Med. 1998; 338:777–783.

16. Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998; 351:805–806.

17. Moorthi RN, Kandula P, Moe SM. Optimal vitamin D, calcitriol, and vitamin D analog replacement in chronic kidney disease: to D or not to D: that is the question. Curr Opin Nephrol Hypertens. 2011; 20:354–359.

18. Coyne DW. The KDOQI US commentary on KDIGO anemia guideline and quality of life. Am J Kidney Dis. 2014; 63:540.

19. Cană-Ruiu D, Moţa E, Istrate N, Văduva C, Trican E. Renal anemia - risk factor for chronic kidney disease. Curr Health Sci J. 2013; 39:214–217.
20. Hörl WH. Anaemia management and mortality risk in chronic kidney disease. Nat Rev Nephrol. 2013; 9:291–301.

21. Cases-Amenós A, Martínez-Castelao A, Fort-Ros J, Bonal-Bastons J, Ruiz MP, Vallés-Prats M, et al. Prevalence of anaemia and its clinical management in patients with stages 3-5 chronic kidney disease not on dialysis in Catalonia: MICENAS I study. Nefrologia. 2014; 34:189–198.
22. Chang JM, Chen SC, Huang JC, Su HM, Chen HC. Anemia and left ventricular hypertrophy with renal function decline and cardiovascular events in chronic kidney disease. Am J Med Sci. 2014; 347:183–189.

23. Tirmenstajn-Jankovic B, Dimkovic N, Perunicic-Pekovic G, Radojicic Z, Bastac D, Zikic S, et al. Anemia is independently associated with NT-proBNP levels in asymptomatic predialysis patients with chronic kidney disease. Hippokratia. 2013; 17:307–312.
24. Hung SC, Kuo KL, Tarng DC, Hsu CC, Wu MS, Huang TP. Anaemia management in patients with chronic kidney disease: Taiwan practice guidelines. Nephrology (Carlton). 2014; 19:735–739.

25. Aucella F, Scalzulli RP, Gatta G, Vigilante M, Carella AM, Stallone C. Calcitriol increases burst-forming unit-erythroid proliferation in chronic renal failure. A synergistic effect with r-HuEpo. Nephron Clin Pract. 2003; 95:c121–c127.
26. Aucella F, Gatta G, Vigilante M, Scalzulli RP, Mantuano S, Carotenuto M, et al. [Calcitriol increases burst forming unit-erythroid (BFU-E) in vitro proliferation in chronic uremia. Synergic effect with DNA recombinant erythropoietin (rHu-Epo)]. Minerva Urol Nefrol. 2001; 53:1–5.
27. Zughaier SM, Alvarez JA, Sloan JH, Konrad RJ, Tangpricha V. The role of vitamin D in regulating the iron-hepcidin-ferroportin axis in monocytes. J Clin Transl Endocrinol. 2014; 1:19–25.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download