Abstract
Intraductal carcinoma of the prostate (IDC-P) is characterized by prostatic carcinoma involving ducts and/or acini. The presence of IDC-P is usually associated with a high-grade Gleason score, large tumor volume, and adverse prognostic parameters, including extraprostatic extension and seminal vesicle invasion. When present, IDC-P is associated with worse outcomes, regardless of treatment status. IDC-P is included in a broader diagnostic category of atypical cribriform lesions of the prostate gland. This category of lesions also includes high-grade prostatic intraepithelial neoplasia (HGPIN), urothelial carcinoma involving prostatic ducts or acini, and prostatic ductal adenocarcinoma, amongst other intraductal proliferations. Differentiating between these entities is important as they have differing therapeutic and prognostic implications for patients, although differential diagnosis thereof is not always straightforward. The present review discusses IDC-P in regards to its morphological characteristics, molecular features, and clinical outcomes. Given the current state of knowledge, the presence of IDC-P should be evaluated and documented correctly in both radical prostatectomy and needle biopsy specimens, and the clinical implications thereof should be taken into consideration during treatment and follow up.
Intraductal carcinoma of the prostate (IDC-P) is a malignant lesion characterized by an expansile proliferation of malignant prostatic secretory epithelial cells within prostatic ducts and acini, and demonstrates significant architectural and cytological atypia.1 The presence of IDC-P in a specimen is frequently associated with large tumor volume, advanced disease stage, high Gleason score, and increased risk of recurrence.2 The diagnostic criteria and clinical significance of this entity continue to evolve as more studies are undertaken, and advances in the understanding of its' pathogenesis are supported by immunohistochemical and genetic markers.
With increasingly frequent recognition of IDC-P, the differential diagnosis of atypical medium sized and large cribriform lesions on prostate core needle biopsies has become more challenging. The differential diagnosis for this group of lesions includes several entities, with differing therapeutic and prognostic implications. High-grade prostatic intraepithelial neoplasia (HGPIN) is considered a preneoplastic lesion; its presence does not require definitive treatment, and when present exclusively in an extended core biopsy, does not warrant another biopsy.3 Meanwhile, IDC-P, when present in a core needle biopsy, requires a prompt rebiopsy or definitive treatment.2 Atypical intraductal proliferations are borderline lesions that exhibit atypical features greater than those seen in HGPIN, but not entirely fulfilling the diagnostic criteria for IDC-P.4 Other entities included in the list of differential diagnoses for IDC-P include high-grade, invasive prostatic acinar adenocarcinoma, prostatic ductal adenocarcinoma, and urothelial carcinoma involving prostatic ducts. The morphological features, diagnostic criteria, and molecular characteristics of IDC-P and the distinction of this category of lesions from the aforementioned entities are discussed herein. Correctly diagnosing IDC-P is not only important for pathologists, but also for other members of the clinical team, including urologists and medical and radiation oncologists.
The term IDC-P has been employed interchangeably over the years to refer to prostatic ductal adenocarcinoma, prostatic acinar adenocarcinoma, and extension of urothelial carcinoma into prostatic ducts and acini.5 IDC-P was previously used to refer to carcinoma cells extending into prostatic ducts and acini, in which the subtype of tumor cells included neoplastic prostate epithelium, as well as urothelial and squamous carcinoma cells.15 This was in contrast to the initial description proposed by Kovi, et al.6 in 1985, wherein prostate carcinoma cells are reported to involve pre-existing prostate ducts and acini. It was suggested that prostate carcinoma cells could also involve or extend into benign prostatic ducts, owing to the observation that features now recognized as IDC-P were present in a significant subset (almost 50% of cases) included in the study. McNeal, et al.7 also documented that some cases of prostate carcinoma demonstrating a cribriform growth pattern have a higher Gleason score than their counterparts with non-cribriform morphology, and also exhibit features consistent with an IDC-P component. IDC-P lesions were included under the uniform diagnostic category of HGPIN when Bostwick and Brawer8 introduced this concept. Therefore, a diagnosis of IDC-P was not rendered frequently, as these proliferations were included in the diagnostic category of HGPIN. However, as pathogenesis of this ductal proliferation has become better understood, IDC-P is used to refer to prostatic adenocarcinoma that extends into and proliferates within preexisting prostatic ducts. IDC-P can exhibit a variety of growth patterns, including loose or dense cribriform, solid, micropapillary, and rarely, flat architecture. The cells exhibit cuboidal or columnar cytological features with significant nuclear enlargement.4 Several similar diagnostic criteria schemes for the morphologic diagnosis of IDC-P have been proposed:910 the major diagnostic criteria for IDC-P include 1) solid or dense cribriform architecture (defined as atypical cells spanning greater than 50% of the glandular lumina), 2) marked nuclear atypia or pleomorphism with nucleomegaly (≥six times normal), and 3) non-focal comedonecrosis.9 The presence of any of these criteria is considered diagnostic for IDC-P in conjunction with the presence of medium to large sized ducts or glands with at least partial preservation of an identifiable basal cell layer.
Minor criteria for IDC-P that are often present and helpful but not diagnostic include 1) involvement of greater than six glands and/or ≥1 mm size, 2) atypical glands that are irregular or branching at right angles, 3) increased mitotic activity with frequently identified mitotic figures, and 4) two distinct cell populations comprising of an outer layer of pleomorphic, mitotically active cells and a central component of cuboidal, monomorphic cells without mitotic activity.491011 In IDC-P with two morphologically distinct cell populations, the outer layer of pleomorphic cells does not stain strongly with prostate-specific antigen (PSA), whereas the inner monomorphic cells demonstrate strong PSA positivity.12 Immunohistochemistry (IHC) is also considered helpful in establishing a diagnosis of IDC-P in terms of confirming the presence of at least an incomplete or partial basal cell layer around the atypical glands. Morphologic patterns and cytologic features required for diagnosis of IDC-P are represented in Fig. 1.
IDC-P is associated with aggressive prostatic adenocarcinoma and its presence in both core needle biopsy and radical prostatectomy specimens is associated with adverse prognosis. IDC-P is not usually identified in prostate core biopsies, and this finding is supported by a recently published study with a significant cohort of more than 100 consecutive prostate biopsies, wherein an overall incidence of 2.8% of IDC-P was reported. The incidence of IDC-P with simultaneously identified foci of invasive adenocarcinoma in a core needle biopsy ranges from 10% to 22%.131415 The presence of isolated IDC-P without accompanying invasive adenocarcinoma is extremely rare, occurring in less than 0.3% of core needle biopsies.2915
Several published studies have shown that the presence of IDC-P correlates with higher Gleason scores, larger tumor volume, increased risk of extraprostatic extension, seminal vesicle invasion, and pelvic lymph node metastases identified upon subsequent radical prostatectomies.6101116171819 In a recent study published by Van der Kwast, et al.,13 the authors reported that the presence of IDC-P in prostate biopsies correlated with early biochemical failure and metastatic disease following radiation treatment in patients with intermediate or high-risk prostate cancer. The presence of IDC-P in radical prostatectomy specimens correlates with decreased progression-free survival and an increase in the incidence of biochemical recurrence following radical prostatectomy. In a similar vein, O'Brien, et al.20 suggested in their study that the predictive accuracy of existing nomograms to predict PSA recurrence after radical prostatectomy may be enhanced upon inclusion of novel pathologic parameters, including IDC-P on prostate biopsies. The presence of IDC-P is associated with a comparatively poor prognosis, following stratification for Gleason score.21
IDC-P represents late-stage progression of prostatic adenocarcinoma in the majority of cases with intraductal extension of high-stage, advanced cancer and this theory has been supported by molecular studies.4 The majority of IDC-P cases show cytoplasmic loss of phosphatase and tensin homolog gene (PTEN, 61–84% cases) as opposed to no loss of PTEN staining in HGPIN. 22 Additionally, a greater frequency of loss of heterozygosity (LOH) of up to 60% is reported in IDC-P cases, compared to no loss in Gleason pattern 3 prostate acinar adenocarcinoma and rare loss in HGPIN cases. However, PTEN loss is reported in one-third of cases with LOH in Gleason pattern 4 prostatic acinar adenocarcinoma.17 LOH of p53 or Rb genes is more frequently seen in IDC-P in 60% and 81% cases, respectively, than HGPIN, which shows LOH of p53 and Rb genes in 30% and 53%, respectively.23 TMPRSS2:ERG gene fusion, which is the most common recurrent chromosomal alteration seen in prostatic adenocarcinoma and identified in approximately 50% of cases, is present in greater than two-thirds of cases of IDC-P and absent in HGPIN.222425 This finding has been confirmed by using both break-apart probes in a fluorescent in situ hybridization (FISH) assay as well as by employing IHC for ERG protein, which shows ERG positivity in a significantly large number of cases of IDC-P (30–58%) in comparison to HGPIN (0–18%).222627
The recognition of IDC-P in a specimen is understood to represent a late-stage occurrence in cases with high-grade, high-stage prostate adenocarcinoma. However IDC-P may represent a precursor lesion to invasive carcinoma in a small subset of cases, representing a point of growth between HGPIN and invasive carcinoma. These precursor type IDC-Ps may represent an entity in the spectrum of neoplastic changes from HGPIN to invasive cancer or possibly an entity in a separate de novo pathway. Miyai, et al.28 reported a cohort of 14 cases of precursor-type IDC-P out of a total of 155 cases with IDC-P. Rare reports of IDC-P occurring without the concomitant presence of invasive carcinoma or in the presence of only Gleason score 6 cancer documented on prostatectomy have been published. In this small cohort, outcomes were seemingly better with a decreased incidence of biochemical recurrence; however, these cases had a relatively limited follow-up.929
It is, therefore, important to consider two scenarios when evaluating IDC-P: whether it is seen in association with invasive prostate carcinoma or not. The former group focuses on prognostic factors used mainly to predict outcome, and can be applied to both radical prostatectomy samples and needle biopsies. The latter is focused on impacting decisions for subsequent therapy, and can only be applied in the setting of core needle biopsies. These differences should be considered whenever IDC-P is reported.
Distinguishing HGPIN from IDC-P is significant from a clinical viewpoint, and can be challenging in some cases. A greater degree of architectural and cytological atypia is seen in association with IDC-P, although both IDC-P and HGPIN demonstrate cytologically atypical cells within prostatic ducts and acini. The outlines of prostatic ducts and glands with HGPIN are usually smooth with rounded contours, in contrast to irregular outlines with branching in IDC-P. The prostatic glands are usually similar in size to adjacent, benign glands in HGPIN, and cells lack marked nuclear atypia with nuclear size, measuring 2 to 3 times that of adjacent benign nuclei (Fig. 2A). The mitotic activity is not significantly increased in HGPIN with only occasional mitotic figures identified. The cells in HGPIN are more uniform as opposed to pleomorphic cells seen in IDC-P. Both IDC-P and HGPIN may exhibit micropapillary, flat, or loose cribriform growth patterns, although solid nests and dense cribriform architecture are more frequently seen in IDC-P.3031 Only very focal comedonecrosis may be rarely identified in HGPIN, and non-focal comedonecrosis is almost always seen in association with IDC-P. Using the above-described criteria for the diagnosis of IDC-P, HGPIN can usually be readily distinguished from IDC-P. IDC-P may occasionally demonstrate a spectrum of features that include low-grade cytology with uniform nuclei and small, regularly contoured glands. It may occasionally prove to be a challenging task to distinguish between HGPIN and IDC-P on core needle biopsies.4 Both HGPIN and IDC-P exhibit similar IHC phenotypes, including overexpression of α-methylacyl coenzyme A racemase (AMACR) and patchy positivity for basal cell markers. In such circumstances, IHC staining for PTEN and ERG may be helpful in distinguishing between these two entities, as loss of PTEN expression and ERG overexpression are seen in IDC-P, whereas retained PTEN expression and absence of ERG overexpression are usually seen in HGPIN.22 Sometimes the lesion of interest is very focal or exhibits overlapping features between IDC-P and HGPIN, precluding a definitive interpretation, and a diagnosis of atypical intraductal proliferation or atypical cribriform lesion (ACL) may be rendered in these difficult cases.32 Table 1 highlights the morphologic and immunohistochemical features that distinguish HGPIN from IDC-P.
HGPIN without concomitant invasive prostatic adenocarcinoma is diagnosed more frequently, with an incidence of up to 8% in core needle biopsies. The risk of invasive adenocarcinoma on a repeat core needle biopsy following a diagnosis of isolated HGPIN in extended core biopsies is 20–25%. This is similar to the risk of invasive adenocarcinoma on a repeat biopsy following a benign diagnosis. It is not mandatory to require a repeat biopsy following a diagnosis of isolated HGPIN on an extended core biopsy, thus making the distinction between HGPIN and IDC-P signficant.3
An atypical intraductal proliferation is seen microscopically as a lesion spanning the lumen of prostatic ducts or glands, and demonstrating the presence of cells with cytological atypia that exceeds the cytoarchitectural features of HGPIN but is not sufficient to meet the threshold for a definitive diagnosis of IDC-P (Fig. 2B).33032 The term is employed for diagnostic clarification for borderline lesions in which neither HGPIN nor IDC-P can be definitively diagnosed and does not represent a definitive entity.
Morphologically, the following criteria have been put forth for diagnosing atypical intraductal proliferations by Morais, et al.:26 1) loose cribriform architecture with greater atypia than expected to be seen in HGPIN, yet lacking significant pleomorphism or necrosis to qualify for IDC-P; 2) cytological atypia with significant pleomorphism but not meeting criteria required for IDC-P (≥six times adjacent benign nuclei), or 3) dense cribriform or solid proliferation of cells with cytological atypia in incompletely sampled large ducts on the edge of biopsy specimens. In their study, 60 patients with atypical intraductal proliferations were included and a repeat biopsy was performed in 35 cases along with prostatectomy in one case. Invasive prostatic adenocarcinoma (15 cases) or IDC-P (3 cases) were identified on repeat biopsies in approximately 50% cases. In the cohort where invasive adenocarcinoma was seen on repeat biopsies, about half of the cases (n=7) were assigned a Gleason score of 7 or higher. As the likelihood of finding high-grade (Gleason score ≥7) is significantly greater in the lesions diagnosed as atypical intraductal proliferation, an immediate repeat biopsy is therefore recommended in these cases.25 Cytoplasmic loss of PTEN or ERG expression was also frequently associated with atypical intraductal proliferation (52% and 27%, respectively) in this same study. Out of the 11 cases exhibiting PTEN loss, seven cases had follow-up biopsies with a diagnosis of either invasive prostatic adenocarcinoma or IDC-P. This rate of subsequent carcinoma is significantly higher than that associated with atypical small acinar proliferation, but only slightly higher than that seen in PTEN-intact, atypical intraductal proliferation (50%).
In another study by Miyai, et al.,32 IDC-P, atypical intraductal proliferation or ACL, and HGPIN were recorded in 155, 22, and 436 cases, respectively, in a series of 901 radical prostatectomies. Patients with IDC-P showed more aggressive pathologic features when compared to HGPIN. Invasive cancers in patients with ACL had higher Gleason score, larger tumor volume, and more advanced pT stage than those with HGPIN. Cases with atypical intraductal proliferation showed a higher risk of biochemical recurrence than those with HGPIN and a lower risk than those with IDC-P based on log-rank tests (p=0.0045 and 0.0069, respectively). A recommendation from this study was that atypical intraductal proliferations should be distinguished from HGPIN, as these lesions mandate active clinical surveillance with repeat biopsy within 3 months.
Invasive acinar adenocarcinoma with cribriform or solid architectural patterns (Gleason patterns 4 and/or 5) may resemble IDC-P, and warrants distinction for further management. The absence of basal cells around the ductal or glandular units serves to distinguish invasive high-grade acinar adenocarcinoma of prostate from IDC-P. Although IHC staining for basal cells distinguishes IDC-P from invasive acinar adenocarcinoma and is very helpful in this regard, it is not always performed owing to similar clinical management of both these types of lesions.
Prostatic ductal adenocarcinoma is an aggressive form of adenocarcinoma of the prostate, representing less than 1% of prostatic adenocarcinoma cases, and is usually seen in association with high-grade prostatic acinar adenocarcinoma.43334 It may arise from both large-sized periurethral or peripheral prostatic ducts, and is associated with hematuria and/or obstructive urinary symptoms.333435 This malignancy also presents as an exophytic, papillary mass protruding into the urethral lumen in continuity with periurethral ducts. Microscopically, it demonstrates pseudostratified tall, columnar cell morphology. Other frequently encountered features that help in establishing the diagnosis include the presence of papillary architecture with fibrovascular cores or a cribriform growth pattern with large sized, back-to-back glandular elements with intraglandular bridging and narrow slit-like lumina akin to a Mullerian "endometrioid" pattern (Fig. 2C).2 TMPRSS2:ERG gene fusions are reported to occur in prostatic ductal adenocarcinoma albeit with a lesser frequency. 3
This entity may also cause diagnostic confusion with IDC-P when the cribriforming architecture is prominent and the malignant glands have relatively round contours. Morphologic clues to a diagnosis of prostatic ductal adenocarcinoma include the presence of true fibrovascular cores that are lacking in IDC-P and the presence of pseudostratified, columnar cells, in contrast to cuboidal cells lining the cribriform nests in IDC-P.
IHC staining is also helpful as it demonstrates a lack of staining for basal cell markers in prostatic ductal adenocarcinoma. A pitfall to consider is that basal cells may be seen underlying the pseudostratified, columnar cells in cases of prostatic ductal adenocarcinoma; however, this likely represents intraductal spread of prostatic ductal adenocarcinoma.36 Establishing a diagnosis of prostatic ductal adenocarcinoma is clinically relevant since it is considered to represent high-grade (Gleason score 8 or higher) cancer.37383940 It is associated with adverse pathologic parameters, including a greater incidence of extraprostatic extension and seminal vesicle invasion apart from lower biochemical-free survival subsequent to radical prostatectomy.3341424344
Prostatic intraepithelial neoplasia-like (PIN-like) adenocarcinoma of prostate, which is a variant of prostatic ductal adenocarcinoma, is also included in the differential diagnosis of IDC-P and prostatic ductal adenocarcinoma as it demonstrates a pattern of medium to large sized dilated glands lined by pseudostratified, columnar epithelial cells.45 This tumor does not behave as aggressively as the aforementioned classic type of prostatic ductal adenocarcinoma. Cytologically, PIN-like prostatic ductal adenocarcinoma is composed of uniformly elongated, monomorphic nuclei without prominent nucleoli, and lacks the cytological pleomorphism seen in IDC-P.4546 Distinguishing features from IDC-P include the absence of cribriform and solid growth patterns. IHC for basal markers is significantly helpful in this aspect since it will show lack of basal cells in PIN-like prostatic ductal adenocarcinoma.
Urothelial carcinoma involving prostatic ducts can also mimic IDC-P by growing into and distending prostatic ducts and acini. It can also demonstrate foci of comedonecrosis further confounding the differential with IDC-P. The often countered papillary growth pattern of urothelial carcinoma may be absent, although divergent squamous differentiation, when present, may be of assistance in distinguishing urothelial carcinoma from IDC-P. Mitotic activity is also frequently elevated in urothelial carcinoma cases, serving as a useful feature (Fig. 2D). IHC staining is immensely helpful in distinguishing urothelial carcinoma from IDC-P, as urothelial carcinoma cells are negative for various prostatic lineage markers, including PSA, NKX3.1, prostate-specific membrane antigen, P501S (prostein), and prostate-specific acid phosphatase. Urothelial carcinoma involving prostatic ducts is positive for expression of urothelial markers, including uroplakin 2 or 3, GATA3, high molecular weight cytokeratin 34βE12, and p63.4 Additionally, basal cell markers show the presence of basal cells surrounding the glandular units in cases of urothelial carcinoma extending into prostatic ducts and acini. Identification of urothelial carcinoma involving prostatic ducts is also important as cystoprostatectomy with or without accompanying chemotherapy is the treatment of choice in such cases.
IDC-P should be reported in both core needle biopsies and radical prostatectomy specimens when it is seen in association with invasive adenocarcinoma or as isolated IDC-P without concomitant invasive carcinoma. Assigning a Gleason grade to IDC-P is not recommended.415
In biopsy specimens, IDC-P should be included in overall volume (percentage) of tumor involvement in a core with conconcomitant invasive carcinoma. The application of IHC staining in IDC-P is dependent on the grade and type of concomitant invasive carcinoma. When IDC-P is seen in association with high-grade invasive prostatic adenocarcinoma (Gleason score 8–10), it should be documented as a morphologic finding, although IHC staining for basal cell markers to establish a diagnosis of IDC-P is not necessary in such cases.
IHC for basal markers (p63, CK5/6 and high molecular weight cytokeratin) is performed in the setting of IDC-P where there is a need to distinguish IDC-P from invasive carcinoma for quantification of tumor volume or the presence of IDC-P potentially affects the Gleason score. When IDC-P is seen in isolation without concomitant invasive carcinoma, it must be mentioned that IDC-P is often associated with high-grade, high-stage invasive prostate adenocarcinoma, and an immediate repeat biopsy is warranted for such cases. Tables 2 and 3 highlight recommendations for reporting and management strategies in cases of IDC-P and atypical intraductal proliferations.
The decision to proceed with definitive treatment or an immediate rebiopsy in rare instances of IDC-P associated with low-grade (Gleason score 6) cancer should be weighed in a multidisciplinary setting on an individual basis. If the volume of IDC-P is extremely focal or an ACL is diagnosed, a repeat biopsy within 3 months may be recommended. On the other hand, if several biopsy cores are involved by IDC-P with high-grade cytoarchitectural features, then definitive treatment may be recommended.
IDC-P is frequently encountered in association with high-grade and high-stage, invasive prostatic adenocarcinoma, and mandates definitive treatment. It is important to recognize and report these lesions if they are identified in both core needle biopsies and radical prostatectomy specimens, thereby providing the clinical team with an opportunity to consider the presence of this lesion when planning patient care. A crucial distinction in the differential diagnosis is separation of IDC-P from HGPIN, owing to the vastly differing therapeutic and prognostic implications. Thus, IDC-P lies on the malignant end of a spectrum with HGPIN on the preneoplastic, benign end; whereas atypical intraductal proliferation or ACL represents a borderline/intermediate category. IDC-P may be identified in a series of different biopsy and prostatectomy scenarios, and application of the proposed diagnostic criteria and reporting patterns, coupled with immunohistochemical staining, if required, are recommended for outlining further management strategies. Additional studies are required in this area to establish more uniform guidelines and to investigate other possible robust immunohistochemical or molecular markers that may aid in establishing an unequivocal diagnosis of IDC-P.
Figures and Tables
Fig. 1
(A) IDC-P with a cribriform growth pattern associated with invasive adenocarcinoma of prostate, Gleason score 4+3=7. Note the presence of a darkly outlined layer of basal cells around the circumference of the involved duct. (B) IDC-P with a densely solid growth pattern associated with invasive high-grade adenocarcinoma of prostate (Gleason score 8) in a prostatectomy specimen. (C) A core biopsy of prostate showing IDC-P with a prominent cribriform growth pattern spanning the entire lumen of the prostatic ducts, measuring >2 mm. (D) High-grade cytologic features of lesional cells in IDC-P with significantly enlarged nuclei exhibiting marked pleomorphism and focal comedonecrosis (right side). (E) Nonfocal comedonecrosis associated with IDC-P. Note the high-grade cytologic features with uniform significantly enlarged nuclei and prominent nucleoli. (F) IDC-P with cribriform growth pattern present at the edge of a core needle prostate biopsy specimen. Thus focus may be interpreted as an atypical cribriform lesion or atypical intraductal proliferation in the absence of unequivocal foci of IDC-P elsewhere in the specimen. IDC-P, intraductal carcinoma of the prostate.
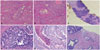
Fig. 2
Entities comprising the list of differential diagnoses for IDC-P. (A) HGPIN with cribriform growth pattern lacking the high-grade cytologic atypia and complex architecture of IDC-P. The nuclei are not as significantly enlarged as seen in IDC-P. (B) Atypical intraductal proliferation or atypical cribriform lesion. Although this atypical proliferation demonstrates architectural complexity greater than that encountered with HGPIN, it does not display the high-grade cytological features and solid or dense cribriform proliferation seen frequently in IDC-P. (C) Ductal adenocarcinoma of prostate can also demonstrate areas of cribriform growth, however, presence of true fibrovascular cores in the papillary areas and pseudostratified tall, columnar nuclei serve to distinguish this entity from IDC-P. Most importantly there are no identifiable basal cells in this entity. (D) Urothelial carcinoma can also extend along prostatic ducts and acini mimicking IDC-P. The presence of tumor cells with a 'squamoid' appearance is a helpful feature that assists in making a distinction from IDC-P apart from IHC stains which are diagnostic in these cases. IDC-P, intraductal carcinoma of the prostate; HGPIN, high grade prostatic intraepithelial neoplasm; IHC, immunohistochemistry.
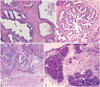
Table 1
Morphological and IHC Features of IDC-P and HGPIN

Table 2
Reporting Recommendations for IDC-P in Different Scenarios

Table 3
Recommendations for Therapy in Patients with IDC-P

References
1. Rhamy RK, Buchanan RD, Spalding MJ. Intraductal carcinoma of the prostate gland. J Urol. 1973; 109:457–460.

2. Robinson BD, Epstein JI. Intraductal carcinoma of the prostate without invasive carcinoma on needle biopsy: emphasis on radical prostatectomy findings. J Urol. 2010; 184:1328–1333.

3. Epstein JI, Netto GJ. Biopsy Interpretation of the Prostate. 5th ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins;2015.
5. Catalona WJ, Kadmon D, Martin SA. Surgical considerations in treatment of intraductal carcinoma of the prostate. J Urol. 1978; 120:259–261.

6. Kovi J, Jackson MA, Heshmat MY. Ductal spread in prostatic carcinoma. Cancer. 1985; 56:1566–1573.

7. McNeal JE, Reese JH, Redwine EA, Freiha FS, Stamey TA. Cribriform adenocarcinoma of the prostate. Cancer. 1986; 58:1714–1719.

8. Bostwick DG, Brawer MK. Prostatic intra-epithelial neoplasia and early invasion in prostate cancer. Cancer. 1987; 59:788–794.

9. Guo CC, Epstein JI. Intraductal carcinoma of the prostate on needle biopsy: histologic features and clinical significance. Mod Pathol. 2006; 19:1528–1535.

10. Cohen RJ, Wheeler TM, Bonkhoff H, Rubin MA. A proposal on the identification, histologic reporting, and implications of intraductal prostatic carcinoma. Arch Pathol Lab Med. 2007; 131:1103–1109.

11. Shah RB, Magi-Galluzzi C, Han B, Zhou M. Atypical cribriform lesions of the prostate: relationship to prostatic carcinoma and implication for diagnosis in prostate biopsies. Am J Surg Pathol. 2010; 34:470–477.

12. Cohen RJ, McNeal JE, Baillie T. Patterns of differentiation and proliferation in intraductal carcinoma of the prostate: significance for cancer progression. Prostate. 2000; 43:11–19.

13. Van der Kwast T, Al Daoud N, Collette L, Sykes J, Thoms J, Milosevic M, et al. Biopsy diagnosis of intraductal carcinoma is prognostic in intermediate and high risk prostate cancer patients treated by radiotherapy. Eur J Cancer. 2012; 48:1318–1325.

14. Cohen RJ, Chan WC, Edgar SG, Robinson E, Dodd N, Hoscek S, et al. Prediction of pathological stage and clinical outcome in prostate cancer: an improved pre-operative model incorporating biopsy-determined intraductal carcinoma. Br J Urol. 1998; 81:413–418.

15. Watts K, Li J, Magi-Galluzzi C, Zhou M. Incidence and clinicopathological characteristics of intraductal carcinoma detected in prostate biopsies: a prospective cohort study. Histopathology. 2013; 63:574–579.

16. Rubin MA, de La Taille A, Bagiella E, Olsson CA, O'Toole KM. Cribriform carcinoma of the prostate and cribriform prostatic intraepithelial neoplasia: incidence and clinical implications. Am J Surg Pathol. 1998; 22:840–848.

17. Dawkins HJ, Sellner LN, Turbett GR, Thompson CA, Redmond SL, McNeal JE, et al. Distinction between intraductal carcinoma of the prostate (IDC-P), high-grade dysplasia (PIN), and invasive prostatic adenocarcinoma, using molecular markers of cancer progression. Prostate. 2000; 44:265–270.

18. McNeal JE, Yemoto CE. Spread of adenocarcinoma within prostatic ducts and acini. Morphologic and clinical correlations. Am J Surg Pathol. 1996; 20:802–814.
19. Wilcox G, Soh S, Chakraborty S, Scardino PT, Wheeler TM. Patterns of high-grade prostatic intraepithelial neoplasia associated with clinically aggressive prostate cancer. Hum Pathol. 1998; 29:1119–1123.

20. O'Brien BA, Cohen RJ, Wheeler TM, Moorin RE. A post-radical-prostatectomy nomogram incorporating new pathological variables and interaction terms for improved prognosis. BJU Int. 2011; 107:389–395.
21. Kimura K, Tsuzuki T, Kato M, Saito AM, Sassa N, Ishida R, et al. Prognostic value of intraductal carcinoma of the prostate in radical prostatectomy specimens. Prostate. 2014; 74:680–687.

22. Lotan TL, Gumuskaya B, Rahimi H, Hicks JL, Iwata T, Robinson BD, et al. Cytoplasmic PTEN protein loss distinguishes intraductal carcinoma of the prostate from high-grade prostatic intraepithelial neoplasia. Mod Pathol. 2013; 26:587–603.

23. Bettendorf O, Schmidt H, Staebler A, Grobholz R, Heinecke A, Boecker W, et al. Chromosomal imbalances, loss of heterozygosity, and immunohistochemical expression of TP53, RB1, and PTEN in intraductal cancer, intraepithelial neoplasia, and invasive adenocarcinoma of the prostate. Genes Chromosomes Cancer. 2008; 47:565–572.

24. Tomlins SA, Rhodes DR, Perner S, Dhanasekaran SM, Mehra R, Sun XW, et al. Recurrent fusion of TMPRSS2 and ETS transcription factor genes in prostate cancer. Science. 2005; 310:644–648.

25. Han B, Suleman K, Wang L, Siddiqui J, Sercia L, Magi-Galluzzi C, et al. ETS gene aberrations in atypical cribriform lesions of the prostate: Implications for the distinction between intraductal carcinoma of the prostate and cribriform high-grade prostatic intraepithelial neoplasia. Am J Surg Pathol. 2010; 34:478–485.
26. Morais CL, Han JS, Gordetsky J, Nagar MS, Anderson AE, Lee S, et al. Utility of PTEN and ERG immunostaining for distinguishing high-grade PIN from intraductal carcinoma of the prostate on needle biopsy. Am J Surg Pathol. 2015; 39:169–178.

27. Tomlins SA, Palanisamy N, Siddiqui J, Chinnaiyan AM, Kunju LP. Antibody-based detection of ERG rearrangements in prostate core biopsies, including diagnostically challenging cases: ERG staining in prostate core biopsies. Arch Pathol Lab Med. 2012; 136:935–946.

28. Miyai K, Divatia MK, Shen SS, Miles BJ, Ayala AG, Ro JY. Heterogeneous clinicopathological features of intraductal carcinoma of the prostate: a comparison between "precursor-like" and "regular type" lesions. Int J Clin Exp Pathol. 2014; 7:2518–2526.
29. Khani F, Epstein JI. Prostate biopsy specimens with Gleason 3+3=6 and intraductal carcinoma: radical prostatectomy findings and clinical outcomes. Am J Surg Pathol. 2015; 39:1383–1389.
30. Bostwick DG, Amin MB, Dundore P, Marsh W, Schultz DS. Architectural patterns of high-grade prostatic intraepithelial neoplasia. Hum Pathol. 1993; 24:298–310.

31. Amin MB, Schultz DS, Zarbo RJ. Analysis of cribriform morphology in prostatic neoplasia using antibody to high-molecular-weight cytokeratins. Arch Pathol Lab Med. 1994; 118:260–264.
32. Miyai K, Divatia MK, Shen SS, Miles BJ, Ayala AG, Ro JY. Clinicopathological analysis of intraductal proliferative lesions of prostate: intraductal carcinoma of prostate, high-grade prostatic intraepithelial neoplasia, and atypical cribriform lesion. Hum Pathol. 2014; 45:1572–1581.

33. Seipel AH, Wiklund F, Wiklund NP, Egevad L. Histopathological features of ductal adenocarcinoma of the prostate in 1,051 radical prostatectomy specimens. Virchows Arch. 2013; 462:429–436.

34. Samaratunga H, Duffy D, Yaxley J, Delahunt B. Any proportion of ductal adenocarcinoma in radical prostatectomy specimens predicts extraprostatic extension. Hum Pathol. 2010; 41:281–285.

35. Aydin H, Zhang J, Samaratunga H, Tan N, Magi-Galluzzi C, Klein E, et al. Ductal adenocarcinoma of the prostate diagnosed on transurethral biopsy or resection is not always indicative of aggressive disease: implications for clinical management. BJU Int. 2010; 105:476–480.

36. Herawi M, Epstein JI. Immunohistochemical antibody cocktail staining (p63/HMWCK/AMACR) of ductal adenocarcinoma and Gleason pattern 4 cribriform and noncribriform acinar adenocarcinomas of the prostate. Am J Surg Pathol. 2007; 31:889–894.

37. Christensen WN, Steinberg G, Walsh PC, Epstein JI. Prostatic duct adenocarcinoma. Findings at radical prostatectomy. Cancer. 1991; 67:2118–2124.

38. Ro JY, Ayala AG, Wishnow KI, Ordóñez NG. Prostatic duct adenocarcinoma with endometrioid features: immunohistochemical and electron microscopic study. Semin Diagn Pathol. 1988; 5:301–311.
39. Bostwick DG, Kindrachuk RW, Rouse RV. Prostatic adenocarcinoma with endometrioid features. Clinical, pathologic, and ultrastructural findings. Am J Surg Pathol. 1985; 9:595–609.
40. Epstein JI, Woodruff JM. Adenocarcinoma of the prostate with endometrioid features. A light microscopic and immunohistochemical study of ten cases. Cancer. 1986; 57:111–119.

41. Brinker DA, Potter SR, Epstein JI. Ductal adenocarcinoma of the prostate diagnosed on needle biopsy: correlation with clinical and radical prostatectomy findings and progression. Am J Surg Pathol. 1999; 23:1471–1479.
42. Morgan TM, Welty CJ, Vakar-Lopez F, Lin DW, Wright JL. Ductal adenocarcinoma of the prostate: increased mortality risk and decreased serum prostate specific antigen. J Urol. 2010; 184:2303–2307.

43. Amin A, Epstein JI. Pathologic stage of prostatic ductal adenocarcinoma at radical prostatectomy: effect of percentage of the ductal component and associated grade of acinar adenocarcinoma. Am J Surg Pathol. 2011; 35:615–619.

44. Meeks JJ, Zhao LC, Cashy J, Kundu S. Incidence and outcomes of ductal carcinoma of the prostate in the USA: analysis of data from the Surveillance, Epidemiology, and End Results program. BJU Int. 2012; 109:831–834.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download