Methicillin-resistant Staphylococcus aureus (MRSA) is one of the most important pathogen in nosocomial infections. MRSA is mainly treated with antibiotics of the glycopeptide family, such as vancomycin or teicoplanin; however, the minimum inhibitory concentration of MRSA has recently been increased.1 The emerging resistance has led to focus on antibiotics from alternative classes.
Arbekacin has been shown to be effective against MRSA and to exert a longer post-antibiotic effect than that observed with vancomycin.23 Recently, we compared the effectiveness of arbekacin with vancomycin.45 However, there have been no studies to compare the effectiveness of arbekacin with teicoplanin.
This study was conducted as a retrospective case-control study including patients admitted to the hospital from January 1st, 2009 to December 31st, 2010 who received arbekacin (100 mg q 12 hrs, IV) or teicoplanin (400 mg loading, 200 mg q 24 hrs, IV) for treatment of infection caused by MRSA. The MRSA was identified from active pus (arbekacin group vs. vancomycin group, 51 vs. 45), blood (7 vs. 10), sputum (10 vs. 12), and others (3 vs. 4). The arbekacin group and teicoplanin group infected by MRSA was selected by age and gender, matched by propensity score method.
Nephrotoxicity was defined as at least a 50% reduction in glomerular filtration rate using the abbreviated modified diet in renal disease equation.6 Hepatotoxicity was defined as an elevation in aspartate aminotransferase/alanine aminotransferase levels more than two times baseline values during treatment.7
Leukocytopenia was defined as a continuous decrease lower than 4.8×103/µL in the number of white blood cells found in complete blood cell counts during treatment.8 Drug fever was defined as a disorder characterized by fever coinciding with the administration of a drug and disappearing after discontinuation of the drug.
The efficacy was analyzed as bacteriological efficacy response (BER) and clinical efficacy response (CER), and the improvements and failures were classified according to a published study.9 Categorical variables were compared utilizing the McNemar's test, and continuous variables were compared using the Wilcoxon singed rank test. Stata 11.0 software (Stata Corporation, College Station, TX, USA) was used to conduct all analyses, and p-values less than 0.05 were considered statistically significant. This study protocol was approved and performed according to the guidelines of the Institutional Review Board (IRB) of Chonbuk National University Hospital (IRB number 2015-04-038).
During the study period, a total of 235 patients received arbekacin (108) or teicoplanin (127) for treatment of MRSA infections. These patients were matched by age and gender and classified into the arbekacin group (71) and teicoplanin group (71). Therefore, a total of 142 patients with MRSA infections were enrolled in this study. The mean age of the arbekacin group was 56.3±15.4 (14–78) years, and that of the teicoplanin group was 57.6±15.4 (16–78) years (p=0.003). The majority of these patients had skin and soft tissue infections (arbekacin group 60.6% vs. teicoplanin group 63.4%), and clinical statuses (arbekacin group vs. teicoplanin group; pneumonia 14.1% vs. 16.9%, otitis media 11.3% vs. 0%, sepsis 9.8% vs. 14.1%, and others 4.2% vs. 5.6%) were similar between the two groups (p=0.262).
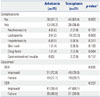
Complications during the medication period were more commonly recorded in the teicoplanin group (36.6%, 26/71) than in the arbekacin group (18.3%, 13/71) (p=0.003) (Table 1). The BER of the arbekacin and teicoplanin groups were 72.9% (51/70) and 70.3% (45/64), respectively: The BER of the arbekacin group was 2.6% higher than that of the teicoplanin group, but this difference was not significant (p=0.835). The CER of the arbekacin group (59.4%, 41/69) was lower than that of the teicoplanin group (69.1%, 47/68), however, this difference was not statistically significant (p=0.257). These results were very similar to our previous arbekacin/vancomycin studies which showed that arbekacin had similar bacteriological and clinical efficacy and excellence in safety in comparison to vancomycin for treating patients with MRSA infection.510
Although BER and CER were not significantly different between the two groups (arbekacin vs. teicoplanin), we nevertheless observed fewer adverse reactions in the arbekacin group than in the teicoplanin group. These results suggest that arbekacin is a good alternative drug to teicoplanin or vancomycin for treatment of MRSA infection.
Figures and Tables
Table 1
Safety and Outcomes in Patients Receiving Arbekacin or Vancomycin
ACKNOWLEDGEMENTS
This study was supported by research funds from Chonbuk National University in 2015 and also by Fund of Biomedical Research Institute, Chonbuk National University Hospital, Jeonju, Korea.
References
1. Miller CE, Batra R, Cooper BS, Patel AK, Klein J, Otter JA, et al. An association between bacterial genotype combined with a high-vancomycin minimum inhibitory concentration and risk of endocarditis in methicillin-resistant Staphylococcus aureus bloodstream infection. Clin Infect Dis. 2012; 54:591–600.

2. Ida T, Okamoto R, Shimauchi C, Okubo T, Kuga A, Inoue M. Identification of aminoglycoside-modifying enzymes by susceptibility testing: epidemiology of methicillin-resistant Staphylococcus aureus in Japan. J Clin Microbiol. 2001; 39:3115–3121.

3. Watanabe T, Ohashi K, Matsui K, Kubota T. Comparative studies of the bactericidal, morphological and post-antibiotic effects of arbekacin and vancomycin against methicillin-resistant Staphylococcus aureus. J Antimicrob Chemother. 1997; 39:471–476.

4. Hwang JH, Lee JH, Moon MK, Kim JS, Won KS, Lee CS. The usefulness of arbekacin compared to vancomycin. Eur J Clin Microbiol Infect Dis. 2012; 31:1663–1666.

5. Hwang JH, Lee JH, Moon MK, Kim JS, Won KS, Lee CS. The efficacy and safety of arbekacin and vancomycin for the treatment in skin and soft tissue MRSA infection: preliminary study. Infect Chemother. 2013; 45:62–68.

6. Manjunath G, Sarnak MJ, Levey AS. Prediction equations to estimate glomerular filtration rate: an update. Curr Opin Nephrol Hypertens. 2001; 10:785–792.

8. Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997; 40:1725.

9. Kim TH, Choo EJ, Lee MS, Kim NJ, Woo JH, Ryu J, et al. Clinical efficacy and safety with arbekacin for methicillin-resistant Staphylococcus aureus (MRSA) infections. Korean J Med. 2003; 65:239–244.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download