Abstract
Purpose
The aim of the study was to investigate and analyze bilateral incidence and morphology of complete discoid lateral meniscus (DLM) with possible relation to tears and symptoms in knee joints.
Materials and Methods
Thirty-eight consecutive patients with symptomatic or already-torn complete DLM on magnetic resonance imaging in a unilateral knee underwent diagnostic arthroscopy on both knee joints upon agreement. The presence and shape of complete DLM as well as presence and pattern of tear were recorded accordingly.
Results
In total, 89.5% (34 of 38 patients) showed bilateral complete DLM, and 84.2% yielded bilateralism with identical shape. Cape-slab was the most frequent shape, comprising 68.8% of patients with identically-shaped bilateral DLM overall. Tear patterns were more frequent, in the order of longitudinal, simple horizontal, radial, and degenerative; however, the morphological shape of complete DLM was not significantly related to tear incidence or pattern. Meniscus tears and knee symptoms occurred in the contralateral knee with incidences of 32.4% and 26.5% in patients with bilateral complete DLM, respectively.
Discoid meniscus is the most common variant of the meniscus, with reported incidences
ranging from 0.4% to 17% for the lateral side and 0.06% to 0.3% for the medial side.1,2,3,4,5,6,7 Discoid meniscus is prone to mechanical or shear stress due to its thick and less vascular structure and its underlying loose peripheral attachment,6,8,9,10,11,12 all of which may necessitate surgical management. Consequently, more insights on the condition, particularly regarding the contralateral knee, would seem to be of clinical importance, especially among Asians, who are known to be more frequently affected by the discoid condition.1,13,14
Historically, overall bilateral occurrence of the condition has been reported in up to 20% of cases for the lateral side.4,9,13,15,16,17,18 Rao and Sripathi Rao9 concluded that the possibility of bilaterality should be suspected in discoid lateral meniscus (DLM), after observing 12 bilateral cases out of 177 arthroscopies for DLM. Bilaterality of discoid meniscus also seems to be more frequent among Asian people. In a Japanese cadaveric study, bilateral DLM was shown in 30.1% (84 out of 279 cadavers), and bilateral DLM with identical shape (either complete or incomplete) was shown in 27.6% of the cases (77 out of 279 cadavers).19 Evaluation with magnetic resonance imaging (MRI) of the contralateral knee has also shown discoid meniscus in 97% of patients with symptomatic DLM, even with an identical discoid shape in 88%.20 A recent prospective study involving arthroscopic evaluation of both knee joints showed bilateral DLM in 79% of 52 consecutive patients with symptomatic unilateral DLM, with bilateral DLM of the same type in 65%.21
Although several studies have been performed on the incidence and bilaterality of DLM, there are still limited numbers of studies on the contralateral knee status in patients with already-known DLM in a unilateral knee. To date, the generally accepted consensus on the management of DLM is to withhold treatment until knee symptoms or tears occur; however, with such management, a non- or minimally-symptomatic contralateral knee is easily ignored without further evaluation in patients diagnosed with DLM in a unilateral knee. Thus, the pre-existing literature on DLM seems rather insufficient as a solid reference to guide knee surgeons in explaining to such patients the potential contralateral knee status in terms of morphological details of discoid meniscus and the rate of accompanying symptoms or tears. Furthermore, the relationship between the structural morphology of DLM and related tears and symptoms has not yet been elucidated. Menisci are mobile structures used not only in the anteroposterior direction but also in axial rotation, along with the femoral condyle. A discoid meniscus can be caught between the femur and the tibia and overly dragged due to its intrinsic thickness and typical shape, both of which may contribute to symptoms.22,23,24,25 One previous study showed a seven-layer-based collagenous orientation of complete-type DLM.26 The collagen fibrils in the anterior and posterior zones are arranged in a radial direction suited for anchoring the meniscus to the tibia, whereas those in the lateral middle zone appeared parallel to the periphery, resisting hoop stresses.26 The medial middle zone was irregular in terms of collagen fibril arrangement.26 Based on the three-dimensional collagenous fibril texture of the discoid lateral meniscus, we hypothesized that the structural morphology of the discoid meniscus might be related to tear patterns or knee symptoms. We also hypothesized that the discoid meniscus itself may not be related to symptoms, although tearing necessarily accompanies symptoms. Thus, the purpose of this study was to investigate and analyze the bilateral incidence and morphology of complete DLM and its possible relation to tear patterns and symptoms in knee joints.
The retrospective study cohort included 38 consecutive patients who underwent arthroscopic surgery on one knee with complete DLM due to tearing or concurrent symptoms and who voluntarily expressed their desire to undergo diagnostic arthroscopy on the contralateral knee simultaneously in the period between January 2002 and December 2008. The definition of "complete" DLM was based on the Watanabe classification as having full coverage of the lateral tibial plateau. When patients with symptomatic unilateral knee symptoms were diagnosed with complete DLM by MRI at the outpatient clinic, we usually explained the possibility of DLM bilaterality, as the bilateral incidence of DLM is known to be much higher among the Asian population. Given that costly MRI expenses for the evaluation of knee pain are not reimbursed by the National Health Insurance System, some patients were willing to be evaluated for the presence of any abnormalities on the contralateral knee without having to pay for an additional high-priced MRI. In fact, some eagerly asked for arthroscopic evaluation on both knee joints simultaneously in one stage, as they did not want to pay extra money for MRI evaluation and additionally wanted to be free from any potential pathology in the contralateral knee in the future. Thus, only those who underwent arthroscopic surgery on one knee and voluntarily wanted to receive diagnostic arthroscopy simultaneously on the contralateral knee were included in the study. The authors affirm that contralateral diagnostic arthroscopy was not performed in any of the patients for any purpose other than patients' voluntary requests.
The patients consisted of 15 males and 23 females with a mean age of 30.6±13.4 years (ranging from 10-54 years). Knee symptoms and signs included subjective pain, popping or snapping, locking, giving way, and objective decreased knee motion. At the time of initial presentation, 36 out of 38 patients (94.7%) complained of subjective knee symptoms in the affected knee, and the other two referred patients had asymptomatic yet surgically-indicated torn DLM, which was confirmed by MRI preoperatively. During arthroscopic evaluation of each knee joint, the presence and shape of complete DLM as well as the presence of any tears and their patterns-if observed-were recorded accordingly. In order to describe the shape of complete DLM during arthroscopy, each case of complete DLM was classified into either a "cape" or "bay" shape in the axial plane and into either a "slab" or "wedge" shape in the coronal plane27 based on the medial edge of the meniscus (Fig. 1). The tear patterns of DLM were also classified into simple horizontal, complicated horizontal, longitudinal, radial, degenerative, and complex tears accordingly.28 In cases of symptomatic complete DLM or asymptomatic DLM presenting a definite tear, meniscoplasty (saucerization) or partial meniscectomy was performed. For asymptomatic cases with no definite tear, no further surgical management was performed.
All data were analyzed with the SPSS statistical package (SPSS 17.0, Chicago, IL, USA). For continuous variables such as age, a t-test was used for comparison between the two groups. For non-continuous variables, either a chi-square test or Fisher's exact test was performed. The level of significance was set at p<0.05.
The study protocol was approved by the Institutional Review Board (IRB) of our institution (AJIRB-MED-MDB-13-250). Informed consent was confirmed by the IRB. The study protocol followed was in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000.
On arthroscopic evaluation of both knee joints, all 38 patients showed complete DLM in the initially-presented knee, and of these patients, 34 (89.5%) had complete DLM in the contralateral knee. When each complete DLM in the initially presented knee was classified according to its shape, cape (in axial), bay (in axial), slab (in coronal), and wedge (in coronal) shapes were observed in 32 (84.2%), 6 (15.8%), 28 (73.7%), and 10 (26.3%) knees, respectively. When axial and coronal shapes were considered simultaneously, cape-slab, cape-wedge, bay-slab, and bay-wedge shapes were shown in 25 (65.8%), seven (18.4%), three (7.9%), and three (7.9%) knees, respectively, with cape-slab being the most frequent shape among them (Table 1). Among 38 initially-presented knees with complete DLM, 26 knees (68.4%) presented with notable tearing. The tear patterns included six simple horizontal (15.8%), 12 longitudinal (31.6%), five radial (13.2%), and three degenerative (7.9%) tears (Table 1).
When the shape of complete DLM in the initially-presented knee was classified according to its tear pattern, there were no significant differences of tear patterns among the different shapes of complete DLM overall (Table 2); neither were there significant differences of tear incidences in coronal (p=0.235) or axial (p=0.920) planes. However, the shape of complete DLM did show sex-based predilection, with females presenting a cape shape more frequently in the axial plane (p=0.027). However, no sex-based difference of coronal shape was noted (p=0.473) (Table 3).
When the two knees of 34 patients with bilateral complete DLM were compared with each other, 94.1% (32 of 34 knees) showed complete DLM with an identical shape in the contralateral knee. Cape-slab in the axial-coronal plane was the most frequent shape of identical bilateral complete DLM, comprising 68.8% of the shapes overall. In patients with bilateral complete DLM, the incidence of meniscus tearing in the contralateral knee was as high as 32.4% (11 of 34 knees) yet still significantly low compared to the tear incidence (67.6%) of the initially-presented knee (p=0.004). The observed tear patterns in the contralateral knee were longitudinal, simple horizontal, radial, and degenerative tears, in the same order of frequency as in the initially-presented knee. Knee symptoms in the contralateral knees, which patients initially did not complain of at the very first visit, were also present in 26.5% of the patients (9 of 34 knees) at the time of operation (Table 4).
Our results showed that the bilateral incidence of complete DLM in Korean knees was 89.5% and the incidence of identical shapes in patients with bilateral complete DLM was 94.1%. In other words, when a patient initially presents with complete DLM in one knee, the chance of morphologically-identical DLM in the contralateral knee is as high as 84.2%, which seems to be greater than previously-reported incidences. In another recent study in which both knee joints were evaluated arthroscopically in patients with symptomatic
DLM, the bilateral incidence was 79%, and 65% of patients had the same DLM types, although this incidence included both complete and incomplete types.21
The reason why we analyzed only the complete type in this study was to provide solid evidence of bilateral incidence to patients who presented with unambiguous complete DLM on preoperative MRI evaluation (assuming that sometimes the incomplete type may be overlooked on MRI evaluation). Bae, et al.21 reported that among 31 patients with symptomatic complete DLM in a knee joint, 19 (61.3%) showed complete type, four were incomplete type, seven were normal, and one showed ring type on contralateral knee evaluation. The greater bilateral incidence observed seems to be more in accord with a study of patients arthroscopically diagnosed with complete unilateral DLM, by Ahn, et al.,20 in which 26 out of 29 (89.6%) also showed the complete type in the contralateral knee on MRI evaluation; however, his study included only young male Asians. Unequivocally, the bilateral incidence of DLM in Asians appears to be much greater than historically-reported incidences studied from non-Asian countries.13,15,16,17,18 We also observed concurrent tears (32.4%) and symptoms (26.5%) in the contralateral knees of patients with bilateral complete DLM who initially presented with complete DLM only in a unilateral knee joint and complained of no symptoms at the very first visit. Thus, it seems plausible to propose that, even if patients complain of no symptoms in the contralateral knee at the initial visit, there is still a potential in the contralateral knee for accompanying tears or eventual symptoms and a higher incidence of the same pathology, at least in patients with previously-confirmed complete DLM in a unilateral knee joint.
Another hypothesis in this study was that the shape of DLM may be related to the tear pattern or knee symptom. We originally anticipated that the more bulky and thick complete discoid meniscus, such as the slab type, could be easily caught between the tibiofemoral condyles, resulting in horizontal tearing due to shear stress, whereas the rather slender complete discoid meniscus, such as the wedge type, would endure less shear stress and present with other meniscus tearing patterns more frequently. Also, as demonstrated in a previous study, longitudinal tearing might be quite frequent in collagen fibrils of the lateral middle zone, which run parallel to the periphery.26 As expected, longitudinal tearing was the most frequent tear pattern overall, and in comparing slab and wedge types in the coronal plane, horizontal tearing was observed only in the slab type (slab: 28.6%; wedge: 0%). However, the morphological shape of complete DLM was not statistically related to the tear pattern or tear incidence overall. Bin, et al.28 analyzed the relationship between the tear pattern and the type of DLM and observed that all simple horizontal tears were observed in the complete type, and complicated horizontal tearing was found significantly more often in the complete type, whereas all radial, degenerative, and complex tears were observed in the incomplete type. No differences were observed in longitudinal tears between the two types.28 Klingele, et al.10 also reported that peripheral rim instability was significantly more common in the complete type than in the incomplete type due to a greater chance of mechanical stress on the thick discoid meniscus. We also demonstrated that longitudinal tearing (which mainly occurs in the periphery) was a frequent tear pattern in complete DLM, and the incidence of longitudinal tearing was 47.6% and 50.0% in the "relatively bulky" slab and cape types, respectively.
Limitations in this study should be addressed. First, the number of patients enrolled in this study was rather small. However, considering that the observed incidence of DLM ranged from 0.4% to 17% overall, 38 consecutive patients seem to be enough to show clinical significance. Second, our study results may be applicable to only Asian patients and may be limited in generalization of characteristics of complete DLM due to racial differences in the incidence of discoid pathology. However, the significantly high incidence of bilaterality and greater chances of accompanying tears and symptoms may encourage the physician to suspect any pathology requiring treatment and consider MRI evaluation on the contralateral knee more actively in Korean patients who definitively show complete DLM in a unilateral knee in preoperative MRI. It is also important to note that while all patients in this study group initially complained of a problem in only a unilateral knee at the very first visit, 26.5% of those with bilateral complete DLM later complained of some kind of discomfort or strange feelings in the contralateral knee after they were informed of the presence of discoid pathology in the affected knee and of the possibility of concurrent pathology in the contralateral knee joint. Based on our experience in a real outpatient practice, physicians need to note that most patients with discoid pathology usually complain of knee symptoms only in a unilateral knee initially and not in both knee joints, making it possible to overlook the presence of symptomatic discoid pathology requiring appropriate treatment at the time of presentation. Thus, more attention should be paid to the contralateral side when consulting with patients with MRI-confirmed unilateral DLM. It is of great importance that patients with symptomatic discoid lateral meniscus in one knee should be well informed of the characteristics of discoid pathology and should be evaluated again on the presence of any symptom on the contralateral knee. Physicians should also sufficiently warn patients to consider visiting again if they feel any discomfort, pain, or any mechanical symptom in the contralateral knee; in such circumstances, MRI evaluation on the contralateral knee may be necessary again. In this perspective, our study may play a role as a solid reference regarding the necessity for more active MRI evaluation of contralateral knee status when consulting with these patients in the outpatient clinic.
In conclusion, we arthroscopically evaluated both knee joints of 38 consecutive patients who presented with symptomatic or already-torn complete DLM in a unilateral knee and observed bilaterality in 89.5% and identically-shaped bilaterality in 84.2%. Cape-slab was the most common shape, and tears and symptoms were also present in the contralateral knee in 32.4% and 26.5% of the patients with bilateral complete DLM, respectively. Based on these findings, more aggressive warning on the presence of discoid pathology and more active evaluation of contralateral knee status should be considered during outpatient clinic consultation with patients with symptomatic complete DLM in a unilateral knee.
Figures and Tables
 | Fig. 1Classification of the shape of complete discoid lateral meniscus based on the arthroscopic morphology of the medial edge. In axial plane, (A) cape or (B) bay shape. In coronal plane, (C) slab or (D) wedge shape. |
Table 1
Characteristics of Initially-Presented Knees with Complete DLM (38 Knees)

Table 2
Morphology of Complete DLM in Initially-Presented Knees According to Tear Pattern
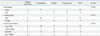
Table 3
Morphology of Complete DLM in Initially-Presented Knees According to Sex
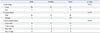
Table 4
Comparison of Characteristics between Initially-Presented Knees and Contralateral Knees in Patients with Bilateral Complete DLM (34 Patients)

DLM, discoid lateral meniscus.
*One patient was asymptomatic at initial presentation yet already had surgically-indicated torn DLM that was confirmed by preoperative MRI.
†The number of patients who later admitted to having some discomfort after being informed of the possibility of discoid pathology in the contralateral knee. It should be noted that all patients in the study presented with a problem only in a unilateral knee at initial presentation.
ACKNOWLEDGEMENTS
This research was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI14C0692).
References
2. Greis PE, Bardana DD, Holmstrom MC, Burks RT. Meniscal injury: I. Basic science and evaluation. J Am Acad Orthop Surg. 2002; 10:168–176.

3. Choi CH, Cho SH, Kim JH, Chung HK. Prevalence of lateral discoid meniscus. J Korean Orthop Assoc. 2002; 37:353–356.

4. Ikeuchi H. Arthroscopic treatment of the discoid lateral meniscus. Technique and long-term results. Clin Orthop Relat Res. 1982; 19–28.

5. Dickason JM, Del Pizzo W, Blazina ME, Fox JM, Friedman MJ, Snyder SJ. A series of ten discoid medial menisci. Clin Orthop Relat Res. 1982; 75–79.

6. Nathan PA, Cole SC. Discoid meniscus. A clinical and pathologic study. Clin Orthop Relat Res. 1969; 64:107–113.
8. Ahn JY, Kim TH, Jung BS, Ha SH, Lee BS, Chung JW, et al. Clinical Results and Prognostic Factors of Arthroscopic Surgeries for Discoid Lateral Menisci Tear: Analysis of 179 Cases with Minimum 2 Years Follow-up. Knee Surg Relat Res. 2012; 24:108–112.

9. Rao SK, Sripathi Rao P. Clinical, radiologic and arthroscopic assessment and treatment of bilateral discoid lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2007; 15:597–601.

10. Klingele KE, Kocher MS, Hresko MT, Gerbino P, Micheli LJ. Discoid lateral meniscus: prevalence of peripheral rim instability. J Pediatr Orthop. 2004; 24:79–82.
11. Rosenberg TD, Paulos LE, Parker RD, Harner CD, Gurley WD. Discoid lateral meniscus: case report of arthroscopic attachment of a symptomatic Wrisberg-ligament type. Arthroscopy. 1987; 3:277–282.

12. Clark CR, Ogden JA. Development of the menisci of the human knee joint. Morphological changes and their potential role in childhood meniscal injury. J Bone Joint Surg Am. 1983; 65:538–547.

13. Dickhaut SC, DeLee JC. The discoid lateral-meniscus syndrome. J Bone Joint Surg Am. 1982; 64:1068–1073.

14. Jordan MR. Lateral Meniscal Variants: Evaluation and Treatment. J Am Acad Orthop Surg. 1996; 4:191–200.

15. Aichroth PM, Patel DV, Marx CL. Congenital discoid lateral meniscus in children. A follow-up study and evolution of management. J Bone Joint Surg Br. 1991; 73:932–936.

16. Bellier G, Dupont JY, Larrain M, Caudron C, Carlioz H. Lateral discoid menisci in children. Arthroscopy. 1989; 5:52–56.

17. Hart ES, Kalra KP, Grottkau BE, Albright M, Shannon EG. Discoid lateral meniscus in children. Orthop Nurs. 2008; 27:174–179.

18. Pellacci F, Montanari G, Prosperi P, Galli G, Celli V. Lateral discoid meniscus: treatment and results. Arthroscopy. 1992; 8:526–530.

19. Kato Y, Oshida M, Aizawa S, Saito A, Ryu J. Discoid lateral menisci in Japanese cadaver knees. Mod Rheumatol. 2004; 14:154–159.

20. Ahn JH, Lee SH, Yoo JC, Lee HJ, Lee JS. Bilateral discoid lateral meniscus in knees: evaluation of the contralateral knee in patients with symptomatic discoid lateral meniscus. Arthroscopy. 2010; 26:1348–1356.

21. Bae JH, Lim HC, Hwang DH, Song JK, Byun JS, Nha KW. Incidence of bilateral discoid lateral meniscus in an Asian population: an arthroscopic assessment of contralateral knees. Arthroscopy. 2012; 28:936–941.

22. Hayashi LK, Yamaga H, Ida K, Miura T. Arthroscopic meniscectomy for discoid lateral meniscus in children. J Bone Joint Surg Am. 1988; 70:1495–1500.

23. Herwig J, Egner E, Buddecke E. Chemical changes of human knee joint menisci in various stages of degeneration. Ann Rheum Dis. 1984; 43:635–640.

24. Kim SJ, Kim DW, Min BH. Discoid lateral meniscus associated with anomalous insertion of the medial meniscus. Clin Orthop Relat Res. 1995; 234–237.

25. Rohren EM, Kosarek FJ, Helms CA. Discoid lateral meniscus and the frequency of meniscal tears. Skeletal Radiol. 2001; 30:316–320.

26. Cui JH, Min BH. Collagenous fibril texture of the discoid lateral meniscus. Arthroscopy. 2007; 23:635–641.

27. Stark JE, Siegel MJ, Weinberger E, Shaw DW. Discoid menisci in children: MR features. J Comput Assist Tomogr. 1995; 19:608–611.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download