Abstract
Purpose
To investigate the prevalence of paralytic ileus after spinal operation in the supine or prone operative position and to determine the efficacy of prophylactic gastrointestinal motility medications in preventing symptomatic paralytic ileus after a spinal operation.
Materials and Methods
All patients received spinal surgery in the supine or prone operative position. The study period was divided into two phases: first, to analyze the prevalence of radiographic and symptomatic paralytic ileus after a spinal operation, and second, to determine the therapeutic effects of prophylactic gastrointestinal motility medications (postoperative intravenous injection of scopolamine butylbromide and metoclopramide hydrochloride) on symptomatic paralytic ileus after a spinal operation.
Results
Basic demographic data were not different. In the first phase of this study, 27 patients (32.9%) with radiographic paralytic ileus and 11 patients (13.4%) with symptomatic paralytic ileus were observed. Radiographic paralytic ileus was more often noted in patients who underwent an operation in the prone position (p=0.044); whereas the occurrence of symptomatic paralytic ileus was not different between the supine and prone positioned patients (p=0.385). In the second phase, prophylactic medications were shown to be ineffective in preventing symptomatic paralytic ileus after spinal surgery [symptomatic paralytic ileus was observed in 11.1% (4/36) with prophylactic medication and 16.7% (5/30) with a placebo, p=0.513].
With any surgery, one faces the risk of complications. When surgery is performed near the spine and spinal cord, these complications can be very serious. Thankfully, however, the chance that any of these complications will occur during spinal surgery is generally very small. Possible complications after spinal surgery have been categorized by different authors as major or minor complications1 and early or late complications.2 Postoperative ileus is a common complication of many surgical procedures.345 Particularly, ileus is a common complication of spinal surgery, affecting 5% to 12% of all spinal surgery patients,26789 and is more frequently observed in surgeries that take a transperitoneal approach, such as anterior lumbar interbody fusion.1011 Often, ileus is secondary to acute colonic pseudo-obstruction,35 however, the actual prevalence of ileus and the efficacy of medication to prevent ileus is not yet well known. Here, we attempted to analyze the prevalence of paralytic ileus after spinal operation in the supine or prone operative position and to determine the efficacy of prophylactic gastrointestinal motility medications in preventing symptomatic paralytic ileus after a spinal operation as a prospective clinical trial.
This is a prospective controlled study. All patients in this study, received general anesthesia for spinal surgery in the supine or prone operative position at a single university hospital from March 2012 to November 2012. The cases with preoperative ileus in imaging studies and with preoperative prokinetic drug usage were excluded in this study. Additionally, all patients received a patient controlled analgesia after the spinal operation. This study was divided into two phases. The first phase was designed to analyze the prevalence of radiographic and symptomatic paralytic ileus after spinal operation in either the supine or prone operative position, while the second phase was designed to determine the therapeutic effects of prophylactic gastrointestinal motility medications on symptomatic paralytic ileus after a spinal operation. If symptomatic paralytic ileus was observed in a patient, the patient controlled analgesia [main regimen with 100 mL mixture of normal saline and fentanyl (patient's weight×24 microliter) or alternative regimen with 100 mL mixture with ketorolac (patient's weight×3 mg)] was discontinued when the patient disagreed the use of opioid, and proper medication for paralytic ileus was administered.
The first phase of this study was conducted from March to July 2012, and included a total of 82 patients. Among the patients, there were 24 cases spinal surgery in the supine position and 58 instances of spinal surgery in the prone position. All spinal operations, according to operative position, as well as the number of cases, are summarized in Table 1. Spinal surgery in the supine position comprised seven cases of cervical artificial disc replacement and 17 cases of cervical anterior discectomy with interbody fusion. Meanwhile, spinal surgery in the prone position comprised 8 cervical spine surgeries with a posterior approach, 9 thoracic spine surgeries with a posterior approach and 41 lumbar spine surgeries with a posterior approach. All patients underwent simple abdomen radiographs in the supine and erect position within 36 hours after a spine operation. All radiographs were analyzed by a single radiologist on the presence of radiographic paralytic ileus. Radiographic paralytic ileus was defined as an accumulation in the bowel within both the small and large bowels (Fig. 1). Symptomatic paralytic ileus was defined as the presence of gastrointestinal symptoms or signs, such as anorexia, nausea, vomiting, epigastric colicky pain, and projectile diarrhea, associated with radiographic findings of paralytic ileus within 3 days after spinal surgery.
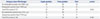
The second phase of this study was conducted from June to November 2012 and included a total of 66 patients (Table 2). Subjects were divided randomly into either the experimental group treated with prophylactic gastrointestinal motility medications or the control group treated with placebo in the nursing ward where the patients received postoperative care. In total, 36 subjects were included in the experimental group, and 30 subjects in the control group. The prophylactic gastrointestinal motility medications were chosen after consultation with a physician at the Department of Internal Medicine. Postoperatively back immediately to the ward, patients in the experimental group were administered an intravenous injection of scopolamine butylbromide (Buscopan Inj®, 20 mg/vial, Handok Pharmaceuticals Co., Seoul, Korea) every 8 hours, as well as an intravenous injection of metoclopramide hydrochloride (Macperan®,10 mg/vial, Dong Wha Pharm Co., Seoul, Korea) every 12 hours for 3 days. Patients in the control group were administered an intravenous injection of normal saline according to the same time schedule as that for the experimental group. The occurrence of postoperative paralytic ileus was considered for instances of symptomatic paralytic ileus only, which was defined as the presence of gastrointestinal symptoms or signs associated with radiographic findings of paralytic ileus within 3 days after spinal surgery.
Statistical analysis was performed using Microsoft Excel 2007. We conducted chi-square tests to compare the prevalences of radiographic or symptomatic paralytic ileus according to the operative position as well as the prophylactic effects of gastrointestinal motility medications in preventing symptomatic paralytic ileus. All p-values<0.05 were considered statistically significant.
Basic demographic data of the patients included in the first and second phases of the present study are shown in Table 1 and 2. No statistical differences in gender and age were observed between the subgroups, except for a larger proportion of males in the first phase of the study. The mean dosages of patient controlled analgesia were observed; 1761.0±265.0 microliters in supine position and 1757.8±266.0 microliters in prone position (p=0.960), while 1803.3±317.8 microliters in prophylactic group and 1717.2±148.0 in non-prophylactic group (p=0.259).
In the first phase of this study, 27 patients (32.9%) with radiographic paralytic ileus and 11 patients (13.4%) with symptomatic paralytic ileus were observed (overlapped symptomatic and radiographic ileus was 7 patients). As shown in Table 3, a statistically significant increase in the number of patients with radiographic paralytic ileus was observed among patients who underwent spinal surgery in the prone position (p=0.044); however, there was no significant difference in the number of patients with symptomatic paralytic ileus (p=0.385). In the second phase of the study, prophylactic medications were shown to be ineffective in preventing symptomatic paralytic ileus, as symptomatic paralytic ileus was recorded in 11.1% (4/36) of the patients treated with prophylactic medication and 16.7% (5/30) treated with a placebo (p=0.513) (Table 4). All patients during the observational periods were relieved from the paralytic ileus after close observation and proper medication.
Ileus is a common postoperative complication noted by spinal surgeons. Although paralytic ileus is considered an early and minor complication after spinal surgery,211 it could affect one's quality of life during postoperative rehabilitation.12 Indeed, patients may consider paralytic ileus a major complication, although most physicians likely would not.1 Paralytic ileus often appears as a secondary to acute colonic pseudo-obstruction, and its occurrence is thought to be even more common than what was once believed.13 Delay in the diagnosis of paralytic ileus can result in serious complications and even death. According to a previous study, the risk for spontaneous perforation is 3%, with an attendant mortality rate of 50%.14 Generally, most patients respond to conservative management and the problem resolves within 3 days, nevertheless, this prolongs hospital stay, and increases costs.
Although often benign, ileus secondary to acute colonic pseudo-obstruction, also known as Ogilvie syndrome, can have serious consequences. Recognition of the presenting features of acute colonic pseudo-obstruction is important for ensuring prompt initiation of treatment in order to hasten recovery and reduce the morbidity and mortality rates associated with this condition. Only four cases of Ogilvie syndrome after lumbar disk surgery have been reported in the literature.7 The most common presenting symptoms of Ogilvie syndrome are abdominal distension, pain, nausea, and vomiting.1 Plain abdominal radiography is the most useful diagnostic test for confirmation of Ogilvie syndrome, and a cecal diameter greater than 9 cm with an absence of distal obstruction should raise concern for the presence of Ogilvie syndrome. Increasing age, immobility, and use of patient-controlled anesthesia are known to be risk factors of Ogilvie syndrome in patients undergoing orthopedic procedures.13
Some authors have previously reported an incidence of 5-6% for paralytic ileus after posterolateral spinal fusion26 and an incidence as great as 12% after combined anterior and posterior spinal fusion.815 In the present study, we observed an incidence of 32.9% (27/82) for radiographic paralytic ileus and 13.4% (11/82) for symptomatic paralytic ileus, which are higher than those of other reports,2678915 but could be explained by differences in the definition of ileus. Most studies defined ileus as no improvement therein after 3 days of conservative management, but we broadly defined paralytic ileus as an accumulation in the bowel (radiographic paralytic ileus) or the presence of gastrointestinal symptoms or signs, such as anorexia, nausea, vomiting, epigastric colicky pain, and projectile diarrhea, associated with radiographic findings of paralytic ileus within 3 days after spinal surgery (i.e., symptomatic paralytic ileus). Our results indicated that silent paralytic ileus occurs more frequently after spinal operation than previously thought and that proper management thereof is needed to ensure proper recovery after surgery.
In this study, we also determined the effectiveness of prophylactic gastrointestinal motility medications in preventing symptomatic paralytic ileus after a spinal operation. The prophylactic gastrointestinal motility medications used in this study were butylscopolamine and metoclopramide hydrochloride. These prophylactic medications were chosen based on the advice of a physician at the Department of Internal Medicine, and have been reported to show good results in paralytic ileus.1617 Scopolamine, another belladonna alkaloid, can be used as an antispasmodic to reduce activity of the gastrointestinal tract.18 Blockade of muscarinic receptors has dramatic effects on motility and some of the secretory functions of the gut, and motility of gastrointestinal smooth muscle is affected from the stomach to the colon.19 Therefore, gastric emptying time is prolonged, and intestinal transit time is lengthened. Indeed, intestinal paralysis induced by antimuscarinic drugs is temporary; local mechanism within the enteric nervous system usually reestablishes at least some peristalsis after anti-muscarinic drug therapy.19 Metoclopramide is promoted as more selective motility stimulants and a potent dopamine antagonist.20 This drug apparently releases acetylcholine from cholinergic neurons in the enteric nervous system's myenteric plexus, and they also sensitize intestinal smooth muscle cells to the action of acetylcholine.20 In clinical applications, metoclopramide produces significant symptomatic relief that is useful for the patients with facilitating small bowel intubation, gastric motor failure-particularly diabetic gastroparesis, or other disorder of gastric emptying.20 In the present study, however the prophylactic medications were shown to be ineffective in preventing symptomatic paralytic ileus, as symptomatic paralytic ileus was noted in 11.1% (4/36) of the patients treated with prophylactic medication and in 16.7% (5/30) of those treated with a placebo (p=0.513). This dissatisfactory result was quite different from the favorable outcomes noted in other disease entities, and it could be due to different treatment regimen.16172021 The clinical series about the colonic pseudo-obstruction treatment among patients after spine surgery was carried out with different regimens of gastrointestinal motility medications such as neostigmine. In this series, neostigmine was a successful treatment in patients with acute colonic pseudo-obstruction in whom conservative management failed. Therefore, a more well-designed study comparing other prophylactic medications for paralytic ileus could show better efficacy in it's prevention.
There are a few limitations to this study that warrant consideration. First of all, the sample size was small to prevent potential type I errors. Indeed, the choice of supine versus prone procedure was not randomized and the mode of operations were different. Therefore, the attributing ileus to procedural position alone can be problematic. Lastly, as data on other prophylactic gastrointestinal motility medications such as neostigmine have been shown to demonstrate clinical prophylactic results different from the results of the present study, readers should be cautious in generalizing the efficacy of the prophylactic motility medications used in this study. A well-designed longitudinal prospective study with a larger number of younger subjects, as well as an equal number of males to females, is needed to overcome these limitations.
In summary, spinal surgery in the prone position was shown to increase the likelihood of radiographic paralytic ileus occurrence, but not symptomatic paralytic ileus. Unfortunately, the prophylactic motility medications used in this study to prevent symptomatic paralytic ileus after spine surgery were shown to be ineffective.
Figures and Tables
Table 1
Demographic Data of the Study's First Phase, Designed to Analyze the Prevalence of Radiographic and Symptomatic Paralytic Ileus after Spinal Operation
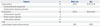
Table 2
Demographic Data of the Study's Second Phase for Determining the Effectiveness of Prophylactic Gastrointestinal Motility Medications in Preventing Symptomatic Paralytic Ileus after a Spinal Operation

Table 3
Radiographic and Symptomatic Paralytic Ileus after Spinal Operation in the Supine or Prone Position
References
1. Ratliff JK, Lebude B, Albert T, Anene-Maidoh T, Anderson G, Dagostino P, et al. Complications in spinal surgery: comparative survey of spine surgeons and patients who underwent spinal surgery. J Neurosurg Spine. 2009; 10:578–584.

2. Cho KJ, Suk SI, Park SR, Kim JH, Kim SS, Choi WK, et al. Complications in posterior fusion and instrumentation for degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2007; 32:2232–2237.
3. Althausen PL, Gupta MC, Benson DR, Jones DA. The use of neostigmine to treat postoperative ileus in orthopedic spinal patients. J Spinal Disord. 2001; 14:541–545.

4. Breusch SJ, Lavender CP. Acute pseudo-obstruction of the colon following left-sided total hip replacement: an analysis of five patients. Int J Clin Pract. 1997; 51:327–329.
5. elMaraghy AW, Schemitsch EH, Burnstein MJ, Waddell JP. Ogilvie's syndrome after lower extremity arthroplasty. Can J Surg. 1999; 42:133–137.
6. Bell DF, Moseley CF, Koreska J. Unit rod segmental spinal instrumentation in the management of patients with progressive neuromuscular spinal deformity. Spine (Phila Pa 1976). 1989; 14:1301–1307.
7. Caner H, Bavbek M, Albayrak A, Altinörs TC. Ogilvie's syndrome as a rare complication of lumbar disc surgery. Can J Neurol Sci. 2000; 27:77–78.
8. Faciszewski T, Winter RB, Lonstein JE, Denis F, Johnson L. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine (Phila Pa 1976). 1995; 20:1592–1599.

9. Hannon JK, Faircloth WB, Lane DR, Ronderos JF, Snow LL, Weinstein LS, et al. Comparison of insufflation vs. retractional technique for laparoscopic-assisted intervertebral fusion of the lumbar spine. Surg Endosc. 2000; 14:300–304.

10. Kang BU, Choi WC, Lee SH, Jeon SH, Park JD, Maeng DH, et al. An analysis of general surgery-related complications in a series of 412 minilaparotomic anterior lumbosacral procedures. J Neurosurg Spine. 2009; 10:60–65.
11. Scaduto AA, Gamradt SC, Yu WD, Huang J, Delamarter RB, Wang JC. Perioperative complications of threaded cylindrical lumbar interbody fusion devices: anterior versus posterior approach. J Spinal Disord Tech. 2003; 16:502–507.

12. Benacker SA. Managing quality on an orthopedic service: ileus in the lumbar spinal fusion patient. J Healthc Qual. 1993; 15:17–20.

13. Clarke HD, Berry DJ, Larson DR. Acute pseudo-obstruction of the colon as a postoperative complication of hip arthroplasty. J Bone Joint Surg Am. 1997; 79:1642–1647.
14. Rex DK. Colonoscopy and acute colonic pseudo-obstruction. Gastrointest Endosc Clin N Am. 1997; 7:499–508.
15. Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999; 341:137–141.
16. Chan DC, Liu YC, Chen CJ, Yu JC, Chu HC, Chen FC, et al. Preventing prolonged post-operative ileus in gastric cancer patients undergoing gastrectomy and intra-peritoneal chemotherapy. World J Gastroenterol. 2005; 11:4776–4781.

18. Mycek MJ, Harvey RA, Champe PC. Lippincott's Illustrated Reviews: Pharmacology. 2nd ed. Philadelphia: Lippincott, Williams & Wilkins;2000.
19. Pappano AJ. Cholinoceptor-blocking drugs. In : Katzung BG, editor. Basic & clinical pharmacology. 8th ed. Philadelphia: Lange Medical Books/McGraw-Hill;2001. p. 107–119.
20. Altman DF. Drugs used in gastrointestinal diseases. In : Katzung BG, editor. Basic & clinical pharmacology. 8th ed. Philadelphia: Lange Medical Books/McGraw-Hill;2001. p. 1064–1076.
21. Holte K, Kehlet H. Postoperative ileus: progress towards effective management. Drugs. 2002; 62:2603–2615.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download