Abstract
Purpose
To analyze the feasibility of unilateral and bilateral translaminar screw placement in Koran population, and compare the acceptance rate using previously reported data in American population.
Materials and Methods
The translaminar lengths, thickness, heights, and sagittal-diagonal measurements were performed. The feasibility analysis was performed using unilateral and bilateral 3.5 mm cervical screw placement on the CT scans within 0.5 mm of safety margin. We also performed radiographic analysis of the morphometric dimensions and the feasibility of unilateral and bilateral translaminar screw placement at C3-C7.
Results
Korean population had similar or significantly shorter translaminar lengths and thickness (lengths and thickness in C7 among males; lengths in C6-C7 and thickness in C4 among females) than American population, but had similar or significantly longer translaminar heights and sagittal-diagonal measurements (heights in C3-C7 and sagittal-diagonal measurements in C3-C6 among males; heights in C7 and sagittal-diagonal measurements in C3-C7 among females). Unilaterally, translaminar screw acceptance rates in C3-C7 were similar between Korean and American male population, but the rates in C4-C6 were significantly smaller between Korean and American female population. Bilaterally, translaminar screw acceptance rates in C3 and C5-C6 were significantly larger between Korean and American male population, but the rates in C3-C7 were similar between Korean and American female population.
Conclusion
The feasibility of unilateral and bilateral translaminar screw placement is different depending on different ethnics. Subaxial cervical unilateral translaminar screw placement among Korean male population and bilateral placement at C4-C7 among Korean female population are more acceptable than American population.
Posterior cervical screw fixation has been broadly used to correct cervical spine instability and spinal deformity, as it has been reported to induce high fusion rates and obviates the need for rigid external mobilization.1,2 Instability of the cervical spine necessitating surgical intervention may be treated with a variety of techniques including posterior wiring, transarticular screws, lateral mass screws and translaminar screws. Lateral mass screws are relatively safe and easy to insert, but lateral mass screw fixation reportedly faces problems of screw loosening or avulsion.3,4,5,6,7 Thus, screw fixation into the cervical pedicle has been proposed as an alternative to overcome these limitations; however, their use in the cervical spine can be technically difficult and potentially harmful to the relatively small cervical pedicles and delicate surrounding structures.1,8,9 Additionally, some authors have recommended the use of a navigation system or laminoforaminotomy technique to aid in cervical pedicle screw placement, but this leads to a longer surgery and more time in the operating room.10,11,12
Recently, translaminar screws have seen greater use as a potentially safer alternative to traditional fusion constructs for fixation of the cervical spine.1,10,12 Translaminar screw placement is simple, and is not limited by the position of the vertebral artery in the transverse foramen, and thereby, may be more applicable to a wider number of patients.13 Although a previous study of an American population reported a 100% unilateral translaminar acceptance rate and a high bilateral acceptance rate at vertebral level C7, limited unilateral acceptance rates were recorded at C4 and C5, where bilateral screws were unable to be placed at all.1 However, the morphology of the subaxial cervical spine can differ among ethnic groups.9 Here, for the first time, the present study describes the feasibility of unilateral and bilateral translaminar screw placement in a Korean population, comparing the acceptance rates thereof with that previously reported for an American population.
Morphometric analyses were performed on the subaxial vertebral lamina of 50 randomly chosen Korean patients (25 males and 25 females) who underwent cervical spine computed tomography (CT) scan, utilizing the same methods described by Alvin, et al.1 in a previous study. Morphometric analysis was completed using the picture archiving and communication system (GE Electronic, NY, USA) at Yonsei University Severance Hospital.
Measurements (length, thickness, height and sagittal-diagonal measurement) were taken in millimeters in the axial, coronal and sagittal planes as described by Alvin, et al.1 All CT scans had resolutions of less than 1 mm. In the axial plane, translaminar length measurements were taken from the junction of the lateral mass and lamina to the contralateral outer cortex of the spinous process (Fig. 1A). Thickness was defined as the greatest maximum measurement spanning from the ventromedial to dorsolateral sides of the central portion of the lamina bilaterally (Fig. 1B). In the coronal plane, laminar height was measured as the maximal height between the spinous process and the base of the pedicle (Fig. 1C). The sagittal-diagonal measurement was made from the most rostral point of the lamina to the most caudal portion of the lamina of the same vertebrae in the sagittal plane (Fig. 1D).
In this study, we assessed the feasibility of translaminar placement of 3.5 mm in diameter screws for correction of cervical spine instability. Probable translaminar screw placement failure was expected for subjects with a thickness and height of less than 4 mm,12,14 and/or a screw length of less than 7 mm (not entering the lamina).15 In addition, a sagittal-diagonal measurement of less than 10 mm was considered indicative of probable bilateral translaminar screw placement failure.
The results are expressed as a mean±standard deviation. Student's t-test was used to assess morphometric analyses between genders, coefficient of determination (R2) to assess the relationship between body height and lamina size, and an independent Student's (σ12=σ22) t-test was conducted to assess statistical differences between a Korean and American population using Microsoft Excel software for Windows (Microsoft Corporation, Redmond, WA, USA). p-values less than 0.050 were considered significant.
In this study, 50 randomized (25 men, 25 women) cervical spine radiographs of a Korean cohort were evaluated and compared to 50 (25 men, 25 women) cervical spine radiographs of an American cohort assessed in a previous study by Alvin, et al.1 For the American cohort, the mean age of the male patients was 54.0±12.1 years (range: 31-75 yr) and the mean age of the female patients was 49.2±15.2 years (range: 22-80 yr). The mean age of the Korean male patients was 49.6±12.5 years (range: 27-72 yr) and the mean age of the Korean female patients was 54.9±16.3 years (range: 21-74 yr). Age was not significantly different between the American and Korean cohorts according to gender (p-value=0.212 in males and 0.207 in females). Although we could not compare body height in the American population, the mean body heights of the Korean male and female patients were 166.0±4.0 cm and 157.0±5.0 cm, respectively. The relationship between body height and lamina size is illustrated as scattered plot in Fig. 2. All the cervical spine measurements of translamina length, thickness, height, and sagittal diagonal were evenly distributed without linear relation to own's body height (all R2 between body height and lamina size <0.100).
Table 1 lists the mean morphometric measurements at each vertebral level (C3-C7) for the Korean men and women. In this group, laminar parameters tended to decrease when moving from C3 to C5 and increase from C6 to C7. Additionally, males tended to have similar or larger laminar values than those of females. Translaminar length did not significantly differ between the genders at levels C3-C5 and C7. At level C5, men had significantly longer translaminar lengths than women (p=0.001). Laminar thickness differed significantly between the genders at levels C3-C5; men exhibited greater laminar thickness than women. At C6-C7, however, laminar thickness did not significantly differ between the genders. Laminar height did not statistically differ between men and women at any of the vertebral levels measured. Men exhibited larger lamina heights at levels C3-C4 than women; however, no gender differences were recorded for laminar height at levels C5-C7. At all vertebral levels measured, except for C7, men had similar or significantly greater laminar sagittal-diagonal measurements than women. Overall, 2000 discrete morphometric measurements were made. The correlation coefficient of two successive intraobserver measurements for morphometric measurements at vertebral levels C3, C4, C5, C6, and C7 was 0.83.
Fig. 3 provides the mean morphometric measurements at each vertebral level (C3-C7) for the Korean and American populations according to gender. The Korean population tended to have relatively smaller laminar lengths and thicknesses than the American population, whereas the Korean population exhibited relatively larger laminar heights and sagittal-diagonal measurements than the American population. Korean males had significantly smaller laminar lengths and thicknesses in C7, but significantly larger laminar heights (C3-C7) and sagittal-diagonal measurements (C3-C7) than the American males. Korean females had significantly smaller laminar lengths at C6-C7 and thicknesses at C4, but had significantly larger laminar heights at C7 and sagittal-diagonal measurements at C3-C7 than American females.
Table 2 lists the unilateral and bilateral translaminar acceptance rates at each vertebral level for men and women of both the Korean and American cohorts. Notably, there were no differences in the unilateral acceptance rate between Korean and American men; however, the bilateral acceptance rate for men at levels C3 and C5-C6 was significantly different. Additionally, there were no significant differences in the bilateral acceptance rate between Korean and American women; however, the unilateral acceptance rate was significantly different between the two at levels C4-C6. The Korean population demonstrated a higher likelihood of successful translaminar screw placement than the American population, especially bilateral placement in men and unilateral placement in women.
Several constructs have been developed to provide fixation throughout the subaxial spine. Among these, pedicle screws are the most biomechanically stable, but their use in the cervical spine carries a high risk of neurovascular complications.15,16,17,18 Although easier and safer to insert, lateral mass screws are known to exhibit lower pullout strengths.19 In contrast, translaminar screws pose no risk of injury to neurovascular structures as translaminar screws remain in the posterior element.7 Another important advantage of translaminar screw fixation is that the use of a fluoroscope or navigation system is not necessary; the screw can be placed under direct vision of the outer cortex of the lamina and all relevant structures.12 Therefore, in instances where a pedicle screw may fail, placement of translaminar screws seems to be a biomechanically sound salvage technique.20,21
Translaminar screw placement requires extensive feasibility and safety assessment before it can be accepted as standard practice as a new spinal procedure, particularly involving instrumentation. Previous cadaveric, clinical and radiological studies have provided important morphometric data, which can be used to assess the feasibility of translaminar screw placement. In the anatomical calculation study of the subaxial cervical spine (cadaveric study) showed that men had greater subaxial laminar measurements compare to women, and the smallest height and the smallest laminar thickness of all vertebrae was C4 and C5.22 Additionally, a case series of the feasibility of subaxial cervical translaminar screw placement demonstrated successful application of translaminar screw fixation with limited adverse outcomes, and it concluded that translaminar fixation is a simple technique not limited by the positioning of vascular structures, and provides high stability to the subaxial cervical spine.13
Most of the literature on adult translaminar anatomy and feasibility focused on C2, C7 and the upper thoracic vertebral levels, with limited mention of the subaxial cervical spine.2,4,8,9,10,12,20,21,23 Morphometric analysis of the subaxial cervical spine has been conducted in only few studies. Yusof and Shamsi24 studied the average transverse lamina diameter of the cervical spine in a Malaysian population to evaluate the feasibility and safety of lamina screw fixation. In this report, the mean transverse inner diameters of the lamina at C2, C3, C4, C5, C6, and C7 were 3.4, 2.0, 1.7, 1.9, 2.3, and 3.4 mm, respectively, while the mean transverse outer diameters of the lamina at C2, C3, C4, C5, C6, and C7 were 5.6, 3.5, 3.1, 3.1, 3.9, and 5.8 mm, respectively. They concluded that translaminar fixation using a 3.5 screw should be attempted with caution in Asian population. Alvin, et al.1 calculated the spatial anatomical environment for translaminar screws at C3-C7, and determined the feasibility of translaminar screw placement at C3-C7 for clinical applicability using CT images and BrainLAB software in an American population. In their study, subaxial cervical unilateral translaminar screw placement was found to be potentially safe and effective technique for use at all vertebral levels; moreover, cervical translaminar screw placement was also reported as a potentially safe and effective technique for bilateral placement at C7, but not at C3-C6.
There are a few differences, however, between the studies of Yusof and Shamsi24 and Alvin, et al.1 Although different methods were used to determine the specific anatomical dimensions of the adult subaxial cervical vertebra laminar and to analyze the feasibility of translaminar screw placement, one reported that unilateral translaminar screw placement is a potentially safe and effective technique for use at all vertebral levels,1 while the other reported that translaminar fixation should be attempted with caution.24 This discrepancy could have derived from differences in ethnicity. Unfortunately, however, there is a lack of data from morphologic analyses of the subaxial cervical spine according to different ethnicities. In the present study, we analyzed the feasibility of unilateral and bilateral translaminar screw placement in Korean population, utilizing the same methods used to determine the specific anatomical dimensions of adult subaxial cervical lamina by Alvin, et al.,1 in order to compare the acceptance rate thereof between Koreans and Americans.
In this study, Korean males tended to have similar or larger laminar values than those of Korean females, as shown in Table 1. Also, laminar parameters tended to decrease when moving from C3 to C5 and increase from C6 to C7. This tendency in cervical spine measurement for the Korean population was not different from the tendency reported in a previous study of Asians and Americans.1,11,24 Notwithstanding, the mean morphometric measurements at each vertebral level (C3-C7) for the Korean and American cohorts showed some differences according to gender, as summarized in Fig. 3. The Korean population tended to have relatively smaller laminar lengths and thicknesses than the American population, while the Korean population exhibited relatively larger laminar heights and sagittal-diagonal measurements than the American population. This result was similar to previous morphometric results for the lumbar spinal canal in Koreans, which was shown to be significantly narrower than those in Caucasian and African populations.25 This difference may influence the differences in the unilateral and bilateral translaminar acceptance rates among Koreans and Americans. In the present study, Koreans demonstrated a higher likelihood of successful translaminar screw placement than the American population, especially bilateral placement in men and unilateral placement in women.
A few limitations warrant further consideration when interpreting the results of this comparison study. Our study population comprised 50 patients and may not have been large enough to generalize the results to the greater population. But, this recent study provided the useful laminar anatomy and its morphometric variations among the subaxial cervical vertebrae. The successful and safe translaminar screw fixation needed the minimum thickness of 4.0 mm or more in the axis, so, we considered the screw placement as a potential success for those with a thickness of more than 4.0 mm.1,3,4,9,14 Moreover, Alvin, et al.1 used an imaginary translaminar screw on BrainLAB software to determine success, and the acceptability of screw placement could be affected by this difference. However, Alvin, et al.1 also commented that their anatomical and feasibility results indicated that, within the subaxial cervical spine, translaminar screws of 3.5 mm in diameter could achieve sufficient purchase rates in lamina with a thickness of 4.0 mm or greater. Therefore, the screw acceptance rate may not be that different. Nevertheless, despite these limitations and although more research is needed, the present study is valuable in that it is the first to report differences in cervical anatomy according to ethnicity.
In conclusion, the feasibility of unilateral and bilateral translaminar screw placement differed according to ethnicity. Performing subaxial cervical unilateral translaminar screw placement in Korean males and bilateral placement at C4-C7 in Korean females was shown to be more feasible than performing the same procedures in Americans.
Figures and Tables
Fig. 1
Morphometric measurement on cervical computed tomography: A, translaminar length was measured from the junction of the lateral mass and lamina to the contralateral outer cortex of the spinous process; B, laminar thickness was measured as the greatest maximum thickness spanning from the ventromedial to the dorsolateral sides of the central portion of the lamina bilaterally; C, laminar height was recorded as the maximal height between the spinous process and the base of the pedicle in the coronal plane; and D, the sagittal-diagonal measurement was made from the most rostral point of the lamina to the most caudal portion of the lamina.

Fig. 2
Scatter plot between body height and translaminar length, thickness, height, and sagittal diagonal in cervical spine showed no linear relationship (all R2<0.100).

Fig. 3
Comparison of morphometric measurements between a Korean and American population. The results reported by Alvin, et al.1 are annotated as "Cleveland," while the results of the current study are indicated as "Korea". *p<0.050.
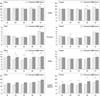
Table 1
Morphometric Analysis of C3-C7 Vertebral Laminar

Table 2
Comparison of Translaminar 3.5 mm Screw Acceptance Rate with 0.5 mm Safety Margin

ACKNOWLEDGEMENTS
This research was supported by the Basic Science Research Program through the National Research foundation of Korea (NRF) funded by the Ministry of Education, Science, and Technology (KRF-2011-0010067) research.
References
1. Alvin MD, Abdullah KG, Steinmetz MP, Lubelski D, Nowacki AS, Benzel EC, et al. Translaminar screw fixation in the subaxial cervical spine: quantitative laminar analysis and feasibility of unilateral and bilateral translaminar virtual screw placement. Spine (Phila Pa 1976). 2012; 37:E745–E751.
2. Wright NM. Posterior C2 fixation using bilateral, crossing C2 laminar screws: case series and technical note. J Spinal Disord Tech. 2004; 17:158–162.
3. Cassinelli EH, Lee M, Skalak A, Ahn NU, Wright NM. Anatomic considerations for the placement of C2 laminar screws. Spine (Phila Pa 1976). 2006; 31:2767–2771.

4. Jea A, Sheth RN, Vanni S, Green BA, Levi AD. Modification of Wright's technique for placement of bilateral crossing C2 translaminar screws: technical note. Spine J. 2008; 8:656–660.

5. Kretzer RM, Chaput C, Sciubba DM, Garonzik IM, Jallo GI, McAfee PC, et al. A computed tomography-based feasibility study of translaminar screw fixation in the upper thoracic spine. J Neurosurg Spine. 2010; 12:286–292.

6. Kretzer RM, Chaput C, Sciubba DM, Garonzik IM, Jallo GI, McAfee PC, et al. Surgical management of two- versus three-column injuries of the cervicothoracic junction: biomechanical comparison of translaminar screw and pedicle screw fixation using a cadaveric model. Spine (Phila Pa 1976). 2010; 35:E948–E954.
7. Kretzer RM, Sciubba DM, Bagley CA, Wolinsky JP, Gokaslan ZL, Garonzik IM. Translaminar screw fixation in the upper thoracic spine. J Neurosurg Spine. 2006; 5:527–533.

8. Leonard JR, Wright NM. Pediatric atlantoaxial fixation with bilateral, crossing C-2 translaminar screws. Technical note. J Neurosurg. 2006; 104:1 Suppl. 59–63.

9. Ma XY, Yin QS, Wu ZH, Xia H, Riew KD, Liu JF. C2 anatomy and dimensions relative to translaminar screw placement in an Asian population. Spine (Phila Pa 1976). 2010; 35:704–708.

10. Chamoun RB, Relyea KM, Johnson KK, Whitehead WE, Curry DJ, Luerssen TG, et al. Use of axial and subaxial translaminar screw fixation in the management of upper cervical spinal instability in a series of 7 children. Neurosurgery. 2009; 64:734–739.

11. Chern JJ, Chamoun RB, Whitehead WE, Curry DJ, Luerssen TG, Jea A. Computed tomography morphometric analysis for axial and subaxial translaminar screw placement in the pediatric cervical spine. J Neurosurg Pediatr. 2009; 3:121–128.

12. Wang MY. Cervical crossing laminar screws: early clinical results and complications. Neurosurgery. 2007; 61:5 Suppl 2. 311–315.

13. Hong JT, Sung JH, Son BC, Lee SW, Park CK. Significance of laminar screw fixation in the subaxial cervical spine. Spine (Phila Pa 1976). 2008; 33:1739–1743.

14. Suk SI, Lee JH, Yoon KS, Kim WJ. The diameter and changes of the vertebral pedicles after screw insertion. J Korean Soc Spine Surg. 1995; 2:168–176.
15. Bozkus H, Ames CP, Chamberlain RH, Nottmeier EW, Sonntag VK, Papadopoulos SM, et al. Biomechanical analysis of rigid stabilization techniques for three-column injury in the lower cervical spine. Spine (Phila Pa 1976). 2005; 30:915–922.

16. Papagelopoulos PJ, Currier BL, Neale PG, Hokari Y, Berglund LJ, Larson DR, et al. Biomechanical evaluation of posterior screw fixation in cadaveric cervical spines. Clin Orthop Relat Res. 2003; 13–24.

17. Shin EK, Panjabi MM, Chen NC, Wang JL. The anatomic variability of human cervical pedicles: considerations for transpedicular screw fixation in the middle and lower cervical spine. Eur Spine J. 2000; 9:61–66.

18. Xu R, Ebraheim NA, Tang G, Stanescu S. Location of the vertebral artery in the cervicothoracic junction. Am J Orthop (Belle Mead NJ). 2000; 29:453–456.
19. Jones EL, Heller JG, Silcox DH, Hutton WC. Cervical pedicle screws versus lateral mass screws Anatomic feasibility and biomechanical comparison. Spine (Phila Pa 1976). 1997; 22:977–982.
20. Jang SH, Hong JT, Kim IS, Yeo IS, Son BC, Lee SW. C7 posterior fixation using intralaminar screws: early clinical and radiographic outcome. J Korean Neurosurg Soc. 2010; 48:129–133.

21. Jang WY, Kim IS, Lee HJ, Sung JH, Lee SW, Hong JT. A computed tomography-based anatomic comparison of three different types of c7 posterior fixation techniques: pedicle, intralaminar, and lateral mass screws. J Korean Neurosurg Soc. 2011; 50:166–172.

22. Xu R, Burgar A, Ebraheim NA, Yeasting RA. The quantitative anatomy of the laminas of the spine. Spine (Phila Pa 1976). 1999; 24:107–113.

23. Hong JT, Yi JS, Kim JT, Ji C, Ryu KS, Park CK. Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation--review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. World Neurosurg. 2010; 73:112–118.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download