Abstract
Purpose
The expression of nerve growth factor-β (NGF-β) is related to cardiac nerve sprouting and sympathetic hyper innervation. We investigated the changes of plasma levels of NGF-β and the relationship to follow-up heart rate variability (HRV) after radiofrequency catheter ablation (RFCA) of atrial fibrillation (AF).
Materials and Methods
This study included 147 patients with AF (117 men, 55.8±11.5 years, 106 paroxysmal AF) who underwent RFCA. The plasma levels of NGF-β were quantified using double sandwich enzyme linked immunosorbent assay method before (NGF-βpre) and 1 hour after RFCA (NGF-βpost-1hr). HRV at pre-procedure (HRVpre), 3 months (HRVpost-3mo), and 1 year post-procedure (HRVpost-1yr) were analyzed and compared with plasma levels of NGF-β.
Results
1) The plasma levels of NGF-β significantly increased after RFCA (20.05±11.09 pg/mL vs. 29.60±19.43 pg/mL, p<0.001). The patients who did not show increased NGF-βpost-1hr were older (p=0.023) and had greater left atrial volume index (p=0.028) than those with increased NGF-βpost-1hr. 2) In patients with NGF-βpre >18 pg/mL, low frequency components (LF)/high-frequency components (HF) (p=0.003) and the number of atrial premature contractions (APCs, p=0.045) in HRVpost-3mo were significantly higher than those with ≤18 pg/mL. 3) The LF/HF at HRVpost-3mo was linearly associated with the NGF-βpre (B=4.240, 95% CI 1.114-7.336, p=0.008) and the NGF-βpost-1hr (B=7.617, 95% CI 2.106-13.127, p=0.007). 4) Both NGF-βpre (OR=1.159, 95% CI 1.045-1.286, p=0.005) and NGF-βpost-1hr (OR=1.098, 95% CI 1.030-1.170, p=0.004) were independent predictors for the increase of LF/HF at HRVpost-3mo.
Previous studies have demonstrated that myocardial injuries, such as myocardial infarction or radiofrequency catheter ablation (RFCA), lead to cardiac nerve sprouting and sympathetic hyper innervation in animal models.1234 Such cardiac nerve sprouting and cardiac sympathetic hyper innervation have been documented to be related to sudden cardiac death56 or atrial fibrillation (AF).7 The nerve regeneration is triggered by the expression of nerve growth factor-β (NGF-β) gene in the non-neuronal cells around the injury site, consequently raising plasma levels of NGF-β.8 Therefore, the increase of the plasma level of NGF-β may indicate active nerve sprouting and generation. However, the relationship between the plasma level of NGF-β and cardiac autonomic nerve activity or arrhythmia in human heart has not yet been evaluated. Heart rate variability (HRV) is a measurement of the cyclic variation of the time intervals between consecutive normal heart beats, and has been widely used to assess cardiac autonomic activity, and may be considered as a marker of sympathetic and parasympathetic influence on the modulation of heart rate (HR). Therefore, HRV is one of the integral components of autonomic nervous system assessment.9 Extensive but titrated atrial tissue damage during catheter ablation of AF was known to increase trans-cardiac NGF concentration in patients with AF.10 However, it has not been elucidated whether the plasma level of NGF increases after RFCA and it may reflect post-procedural cardiac autonomic activity in patients who underwent AF catheter ablation. Therefore, we hypothesized that RFCA for AF changes the plasma concentration of NGF-β, which is associated with 3rd month HRV or frequency of arrhythmias. We also tested the feasibility of double sandwich enzyme linked immunosorbent assay (ELISA) technique for detection of the minimal change of NGF-β in the peripheral blood of patients with AF.
The study protocol adhered to the Declaration of Helsinki and was approved by the Institutional Review Board of Yonsei University Health System. All patients provided written informed consent. This study initially included consecutive 229 patients with AF who underwent RFCA guided by computed tomography (CT) merged 3D NavX electroanatomical map. Exclusion criteria were as follows: 1) permanent AF refractory to the electrical cardioversion, 2) left atrial (LA) anterior posterior dimension >55 mm measured on echocardiogram, 3) uncontrolled thyroid disease, 4) aortic aneurysm or dissection, 5) intracardiac thrombi detected by transesophageal echocardiography, 6) significant rheumatic valvular disease, or 7) previous AF ablation or maze surgery. Among 229 patients, 82 patients were excluded because one of HRV data (pre-RFCA, post-RFCA 3rd months, and post-RFCA 1 year) was not available due to frequent AF or other arrhythmias. We did not include the patients with cardiac implantable electronic device in this study. Finally, 147 patients with acceptable 3 times of HRV data were included for data analysis. The baseline characteristics of the patients are summarized in Table 1. All patients maintained optimal anticoagulation (target international normalized ratio 2.0-3.0) before the procedure and antiarrhythmic drugs (AADs) were discontinued for at least five half-lives of each drug and for at least 4 weeks especially in amiodarone. We examined all patients with 3D-spiral CT (64 Channel, Light Speed Volume CT, Philips, Brilliance 63, the Netherlands) in order to visually define the anatomy of LA.
Intracardiac electrograms were recorded using a Prucka CardioLab™ Electrophysiology system (General Electric Health Care System Inc., Milwaukee, WI, USA). Double trans-septal punctures were performed and multi-view pulmonary venograms were obtained. After obtaining trans-septal access, systemic anticoagulation was achieved with intravenous heparin to maintain an activated clotting time of 350-400 sec. We generated 3D-spiral CT merged 3D electroanatomical mapping (NavX system, St. Jude Medical Inc., Minneapolis, MN, USA). We generated a LA 3D voltage map by obtaining contact bipolar electrograms from 350-500 points of the LA endocardium during high right atrial pacing (pacing cycle length: 500 ms) using a multi-polar ring catheter (Lasso, Johnson & Johnson Inc., Diamond Bar, CA, USA). The bipolar electrograms were filtered from 32 to 300 Hz. Color-coded voltage maps were generated by recording bipolar electrograms and measuring peak-to-peak voltage. The percentage of color-coded areas of voltage maps was analyzed by customized software (Image Pro software 6.0, Media Cybernetics Inc., Silver Spring, MD, USA), referenced to the color scale bars, and utilized for the calculation of the mean and regional endocardial voltages.11
We used an open irrigated-tip catheter (Celsius, Johnson & Johnson Inc., Diamond Bar, CA, USA; irrigation flow rate 20 to 30 mL/min; 30 W; 47℃) to deliver RF energy for ablation (Stockert generator, Biosense Webster Inc., Diamond Bar, CA, USA). Patients with both PAF and PeAF initially underwent circumferential pulmonary vein isolation (CPVI) and cavotricuspid isthmus block. Following CPVI in PeAF patients, we generated an LA roof line, a posterior inferior line, and an LA anterior line, and confirmed bidirectional blocks by differential pacing.12 Depending on the operator's decision, additional ablations for superior vena cava, non-PV foci or complex fractionated electrogram were conducted. If AF persisted beyond the aforementioned ablation protocols for PAF or PeAF, we stopped the procedure after internal cardioversion. The end point of our procedure was the point of no immediate recurrence of AF after cardioversion with isoproterenol infusion (5 µg/min). If there were non-PV foci under isoproterenol infusion, we ablated them all.
Patients were asked to visit the outpatient clinic 1 week, 1 month, 3 months, 6 months, and 12 months after RFCA. AADs were stopped in all patients after procedure, but AAD was prescribed for patients with AF recurrence or highly symptomatic ECG-documented frequent atrial premature beats. Warfarin was maintained for at least 2 months after RFCA. The Holter monitoring (24 hr or 48 hr) were evaluated at pre-RFCA and 3, 6, 12, 18, and 24 months after RFCA following the HRS/EHRA/ECAS Expert Consensus Statement guidelines.13 Patients were also advised to call a clinician or visit the outpatient clinic if they experienced symptoms suggestive of an arrhythmia and Holter (24- or 48-h) or event recorder was performed to document ECG in those symptomatic patients. Patients with any documented AF episode lasting longer than 30 sec after the 3-month follow-up were deemed as having clinical recurrence and AADs were prescribed.
All patients had analyzable HRV data in Holter monitoring taken at 3 different periods (pre-RFCA, post-RFCA 3rd month, and post-RFCA 1 year) by utilizing a GE Marquette MARS 8000 Holter analyzer (GE Medical System, Milwaukee, WI, USA). We excluded the patients whose HRV was not analyzable due to sinus node dysfunction, high number of AF or other arrhythmia episodes. Premature ventricular contractions (PVCs), atrial premature contractions (APCs), and electrical artifacts were also excluded from the analysis. Only high-quality recordings were considered for analysis. All recordings were converted to a digitized format and reviewed by an experienced operator. HRV parameters were obtained and used as an indicator of autonomic activity according to the guidelines previously published.14 The mean HR, time-domain HRV parameters [mean RR interval (mean NN interval), the standard deviation of NN intervals (SDNN), the standard deviation of 5-minute means of NN intervals (SDANN), the root-mean square of differences between successive NN intervals (rMSSD), the proportion of adjacent NN intervals differing by >50 ms (%) (pNN50)], frequency domain parameters [very-low-frequency components (<0.04 Hz), low frequency components (LF; 0.04-0.15 Hz), high-frequency components (HF; 0.15-0.40 Hz), and the ratio of LF/HF] were analyzed, respectively. The HF and rMSSD served as an indicator of parasym-pathetic nervous activity, and the LF and LF/HF ratio reflected sympathetic nervous activity.
Continuous data were expressed as mean±SD and normality tests were performed for each variable to determine whether or not a data set was well-modeled by normal distribution. The baseline characteristics of the two groups were compared using the Student t-test for continuous variables and the chi-square test and Fisher's exact test for categorical variables. We analyzed HRV parameters in Holter monitoring according to the plasma levels of NGF-β before and after RFCA. Baseline characteristics and clinical variables associated with RFCA were also compared according to the plasma levels of NGF-β. Continuous variables were divided and assessed using the median value as the cut-off points. Statistical significance was established at a value of p<0.05. Statistical analysis was performed by SPSS version 20.0 (SPSS Inc., Chicago, IL, USA).
The plasma levels of NGF-β significantly increased 1 hour after RFCA (20.1±11.1 pg/mL vs. 29.6±19.4 pg/mL, p<0.001) (Fig. 1A). There was a significant correlation between the plasma levels of pre-procedural NGF-β and post-procedural NGF-β (R=0.773, p<0.001) (Fig. 1B). Table 1 summarized the baseline characteristics of included patients, and there was no significant difference between the patients with NGF-βpre >18 pg/mL (n=73) and those with ≤18 pg/mL (n=74) based on the median plasma level of NGF-β. When we compared the patients who had an increased plasma NGF-βpost-1hr (n=127) and those did not (n=20), the group with no increase of NGF-βpost-1hr showed older age (p=0.023), lower body mass index (p=0.048), and greater LA volume index (p=0.028) (Table 1). However, higher plasma levels of NGF-β were not related to longer duration of total ablation time. In Post AF ablation, mean heart rate and LF was higher than before ablation. In contrast, rMSSD was higher in pre AF albation (Fig. 1C, D, and E).
Fig. 2 summarized the changes of mean HR and HRV at pre-RFCA (HRVpre), post-RFCA 3 months (HRVpost-3mo), and post-RFCA 1 year (HRVpost-1yr), depending on median plasma levels of NGF-βpre and NGF-βpost-1hr. After catheter ablation of AF, mean HRs were increased at Holterpost-3mo (68.9±12.3 bpm to 72.4±10.3 bpm, p=0.010) and at Holterpost-1yr (71.9±10.1 bpm, p=0.023). The rMSSD (27.1±22.9 ms to 20.6±15.8 ms, p=0.009 and 20.7±14.8 ms, p=0.010), LF (16.4±19.3 Hz to 10.6±11.4 Hz, p=0.003 and 11.3±10.9 Hz, p=0.010) were reduced at HRVpost-3mo and HRVpost-1yr, respectively. We compared HRV parameters depending on the plasma level of NGF-βpre and NGF-βpost-1hr using the median values as a cut-off (Table 2). Compared to the patients with NGF-βpre ≤18 pg/mL, NGF-βpre >18 pg/mL group showed higher LF/HF ratio (p=0.003) and higher number of APCs (p=0.045) in HRVpost-3mo (Fig. 2E and F). LF/HF ratio was also higher in high NGF-βpost-1hr group than in low NGF-βpost-1hr group (p=0.042). Because both sympathetic (represented by LF) and parasympathetic (represented by rMSSD) activities were reduced after AF catheter ablation, we might not have found significant change of LF/HF ratio in the whole population (Fig. 2).
In the uni- and multi-variate linear regression analyses, both NGF-βpre (B=4.240, 95% CI 1.114-7.336, p=0.008) and NGF-βpost-1hr (B=7.617, 95% CI 2.106-13.127, p=0.007) were linearly associated with LF/HF ratio at HRVpost-3mo (Table 3). Both the plasma levels of NGF-βpre (OR=1.159, 95% CI 1.045-1.286, p=0.005) and NGF-βpost-1hr (OR=1.098, 95% CI 1.030-1.170, p=0.004) were independently associated with the increase of LF/HF at HRVpost-3mo (Table 4). However, AF recurrence or ventricular arrhythmic events did not vary depending on the plasma levels of NGF-β.
The present study demonstrated that catheter ablation of AF increases the plasma level of NGF-β significantly, and NGF-β was closely associated with high sympathetic nerve activity estimated by HRV and high number of APCs in Holter performed 3 months after the procedure. However, plasma level of NGF-β was not increased after RFCA in patients with old age and advanced LA remodeling. We also documented the feasibility of double sandwich ELISA technique for detection of the minimal change of NGF-β in the peripheral blood of patients with AF.
Following a peripheral nerve injury, a complex and finely regulated sequence of events lead to neurilemma cell proliferation and axonal regeneration.15 Nerve regeneration is triggered by re-expression of NGF or other neurotrophic factors in the non-neuronal cells around the site of injury.8 NGF and other neurotrophic factors that are derived from myocardial injuries are transported retrograde to the stellate ganglion, which triggers cardiac nerve sprouting in canine models.16 Acute myocardial infarction causes an immediate (within 30 minutes) increase of transcardiac NGF concentration, whereas mRNA of NGF in the damaged myocardium begins to increase 3 days after myocardial infarction and peaks 1 week later.16 NGF over-expression is associated with myocardial hyper innervation and atrial fibrosis,17 and heterogeneous increases in atrial sympathetic innervation contribute to the generation and maintenance of AF by exerting significant effects on automaticity, refractoriness, and conduction velocity.181920 In this study, elevated NGF level was found to be associated with high sympathetic tone and high frequency of APCs after RFCA.
RFCA is a kind of necrotic cardiac injury and induces cardiac nerve sprouting, which has been known to be related to the rises of the level of NGF.416 Kangavari, et al.10 demonstrated that RFCA induces over-expression of NGF mRNA, resulting in increased plasma level of NGF. Although study population and detection methods were different, the current study found consistent elevation of plasma level of NGF-β after RFCA, but, it was not the case in patients with old age, low body mass index, and high LA volume index. We applied the double sandwich ELISA method to enhance detection sensitivity to pg/mL level, and our results of plasma NGF-β level were consistent with other previous reports.212223 Because AF catheter ablation itself has the effects of cardiac autonomic denervation,24 the change of post-ablation HRV cannot be the result of increased plasma level of NGF-β alone. However, the current study found that plasma level of NGF-β was clearly associated with the change of autonomic nerve activity at HRVpost-3mo and HRVpost-1yr.
HRV relies on the principle that the pattern of beat-to-beat control of the sinoatrial node provides a reflection of cardiac autonomic nerve activity.14 Among multiple parameters in HRV, HF components are thought to primarily reflect vagal tone, whereas high LF/HF ratio has been assumed as the index of high sympathetic activity that is known to be pro-arrhythmic and higher frequency of PVCs or APCs.1425 The present study showed that patients with a higher plasma level of NGF-β had a higher LF/HF ratio and a trend of more frequent APCs in Holter monitoring at 3 months after ablation. Although NGF provokes both sympathetic and parasympathetic nerve regeneration, it was associated only with an increased sympathetic nerve activity, but not with an increased parasympathetic nerve activity in this study. This finding may be due to the fact that RFCA destroyed parasympathetic postganglionic cells that are located at or very close to the ablation sites. On the other hand, since sympathetic postganglionic cells are located in the stellate ganglia far from the ablation site, ablation-induced sympathetic nerve axonal damage might recover three months after RFCA. It has been reported that a rapid HR after AF catheter ablation predicts a low recurrence rate of AF.26 Although it might be associated with an appropriate vagal denervation, a high plasma level of NGF-β and an increased post-procedure LF/HF ratio in patients who have less remodeled atrium might contribute to a rapid HR and low recurrence after RFCA.
The present study has several limitations. The patients included in this study were a highly selected group referred for RFCA, and the number of patients was also limited. We excluded patients with LA >55 mm. HRV analysis requires normal sinus rhythm with normal cardiac function, therefore, we excluded patients whose Holter could not be analyzed for HRV. We did not evaluate the long-term change in plasma level of NGF-β after AF ablation. Although we could not find statistical difference of clinical recurrence rate depending on the plasma levels of NGF-β in this small sample size and short follow-up period study, we found the differences in the LF/HF at HRVpost-3mo. Recently, we reported that LF/HF at HRVpost-3mois an independent factor predicting clinical recurrence of AF after RFCA.27 We also found higher LF/HF ratio in HRVpost-3moand higher number of APCs in patients with NGF-βpre>18 pg/mL than those with ≤18 pg/mL, but we do not have direct evidence for the mechanism or causal-results relationship. Further study with a large population may be warranted. We chose post-procedure 1 hour to evaluate the plasma level of NGF-βpost-1hr, but it might not be enough time to show increased plasma level of NGF-β after RFCA. Because we used irrigated tip ablation catheter, irrigated fluid volume might affect the plasma concentration of NGF-β.
In conclusion, AF catheter ablation increases plasma level of NGF-β, and high plasma levels of pre- or post-RFCA NGF-β were associated with high sympathetic nerve activity and the presence of high number of APCs in post-RFCA 3 month Holter. Double sandwich ELISA technique was feasible and acceptable for the detection of the minimal change of NGF-β in the peripheral blood of the patients with AF.
Figures and Tables
 | Fig. 1(A) Plasma levels of NGF-β before and after AF ablation. (B) Correlation between pre- and post-ablation NGF-βs. (C) Mean heart rate in pre AF ablation, post 3 month AF ablation, and post 1 year AF ablation. (D) rMSSD in pre AF ablation, post 3 month AF ablation, and post 1 year AF ablation. (E) LF in pre AF ablation, post 3 month AF ablation, and post 1 year AF ablation. NGF-β, nerve growth factor-β; RFCA, radiofrequency catheter ablation; LF, low frequency components. |
 | Fig. 2Changes of mean heart rate and HRV after catheter ablation of AF. We compared the change of Mean heart rate (A), rMSSD (B), LF (C), HF (D), LF/HF ratio (E), and number of APCs (F) defending on the NGF-βpre plasma level. HRV, heart rate variability; AF, atrial fibrillation; HF, high-frequency components; LF, low frequency components; APCs, atrial premature contractions; NGF-β, nerve growth factor-β. |
Table 1
Patient Characteristics and Comparisons Based on the Median Value of NGF-βpre and Whether Increase of NGF-βpost-1hr

Table 2
Comparisons of HRVpre, HRVpost-3mo, and HRVpost-1yr Depending on the Median Value of NGF-βpre and NGF-βpost-1hr Median Value

Table 3
Uni- and Multivariate Linear Regression Analyses for Pre-NGF-β, Post-NGF-β1hr, and the Increase of NGF-β1hr
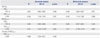
Table 4
Uni- and Multivariate Logistic Regression Analyses for Increase of LF/HF Ratio in HRVpost-3mo Compared with HRVpre

ACKNOWLEDGEMENTS
This work was supported by a grant (A085136 and A120478) from the Korea Health 21 R&D Project, Ministry of Health and Welfare and a grant (7-2013-0362 and 2012027176) from the Basic Science Research Program run by the National Research Foundation of Korea (NRF) which is funded by the Ministry of Science, ICT & Future Planning (MSIP).
References
1. Vracko R, Thorning D, Frederickson RG. Fate of nerve fibers in necrotic, healing, and healed rat myocardium. Lab Invest. 1990; 63:490–501.
2. Nori SL, Gaudino M, Alessandrini F, Bronzetti E, Santarelli P. Immunohistochemical evidence for sympathetic denervation and reinnervation after necrotic injury in rat myocardium. Cell Mol Biol (Noisy-le-grand). 1995; 41:799–807.
3. Cao JM, Fishbein MC, Han JB, Lai WW, Lai AC, Wu TJ, et al. Relationship between regional cardiac hyperinnervation and ventricular arrhythmia. Circulation. 2000; 101:1960–1969.

4. Okuyama Y, Pak HN, Miyauchi Y, Liu YB, Chou CC, Hayashi H, et al. Nerve sprouting induced by radiofrequency catheter ablation in dogs. Heart Rhythm. 2004; 1:712–717.

5. Cao JM, Chen LS, KenKnight BH, Ohara T, Lee MH, Tsai J, et al. Nerve sprouting and sudden cardiac death. Circ Res. 2000; 86:816–821.

6. Chen PS, Chen LS, Cao JM, Sharifi B, Karagueuzian HS, Fishbein MC. Sympathetic nerve sprouting, electrical remodeling and the mechanisms of sudden cardiac death. Cardiovasc Res. 2001; 50:409–416.

7. Chen PS, Tan AY. Autonomic nerve activity and atrial fibrillation. Heart Rhythm. 2007; 4:3 Suppl. S61–S64.

8. Levi-Montalcini R. Growth cntrol of nerve cells by a protein factor and its antiserum: discovery of this factor may provide new leads to understanding of some neurogenetic processes. Science. 1964; 143:105–110.

9. Cygankiewicz I, Zareba W, de Luna AB. Prognostic value of Holter monitoring in congestive heart failure. Cardiol J. 2008; 15:313–323.
10. Kangavari S, Oh YS, Zhou S, Youn HJ, Lee MY, Jung WS, et al. Radiofrequency catheter ablation and nerve growth factor concentration in humans. Heart Rhythm. 2006; 3:1150–1155.

11. Park JH, Pak HN, Choi EJ, Jang JK, Kim SK, Choi DH, et al. The relationship between endocardial voltage and regional volume in electroanatomical remodeled left atria in patients with atrial fibrillation: comparison of three-dimensional computed tomographic images and voltage mapping. J Cardiovasc Electrophysiol. 2009; 20:1349–1356.

12. Pak HN. Large circular ring catheter ablation versus anatomically guided ablation of atrial fibrillation: back to the future for successful catheter ablation of atrial fibrillation? Korean Circ J. 2011; 41:431–433.

13. Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010; 3:32–38.

14. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation. 1996; 93:1043–1065.
16. Zhou S, Chen LS, Miyauchi Y, Miyauchi M, Kar S, Kangavari S, et al. Mechanisms of cardiac nerve sprouting after myocardial infarction in dogs. Circ Res. 2004; 95:76–83.

17. Kiriazis H, Du XJ, Feng X, Hotchkin E, Marshall T, Finch S, et al. Preserved left ventricular structure and function in mice with cardiac sympathetic hyperinnervation. Am J Physiol Heart Circ Physiol. 2005; 289:H1359–H1365.

18. Chang CM, Wu TJ, Zhou S, Doshi RN, Lee MH, Ohara T, et al. Nerve sprouting and sympathetic hyperinnervation in a canine model of atrial fibrillation produced by prolonged right atrial pacing. Circulation. 2001; 103:22–25.

19. Jayachandran JV, Sih HJ, Winkle W, Zipes DP, Hutchins GD, Olgin JE. Atrial fibrillation produced by prolonged rapid atrial pacing is associated with heterogeneous changes in atrial sympathetic innervation. Circulation. 2000; 101:1185–1191.

20. Olgin JE, Sih HJ, Hanish S, Jayachandran JV, Wu J, Zheng QH, et al. Heterogeneous atrial denervation creates substrate for sustained atrial fibrillation. Circulation. 1998; 98:2608–2614.

21. Lee BC, Choi IG, Kim YK, Ham BJ, Yang BH, Roh S, et al. Relation between plasma brain-derived neurotrophic factor and nerve growth factor in the male patients with alcohol dependence. Alcohol. 2009; 43:265–269.

22. Titanji K, Nilsson A, Mörch C, Samuelsson A, Sönnerborg A, Grutzmeier S, et al. Low frequency of plasma nerve-growth factor detection is associated with death of memory B lymphocytes in HIV-1 infection. Clin Exp Immunol. 2003; 132:297–303.

23. Aloe L, Bracci-Laudiero L, Alleva E, Lambiase A, Micera A, Tirassa P. Emotional stress induced by parachute jumping enhances blood nerve growth factor levels and the distribution of nerve growth factor receptors in lymphocytes. Proc Natl Acad Sci U S A. 1994; 91:10440–10444.

24. Mesas CE, Pappone C, Lang CC, Gugliotta F, Tomita T, Vicedomini G, et al. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: electroanatomic characterization and treatment. J Am Coll Cardiol. 2004; 44:1071–1079.

25. Podrid PJ, Fuchs T, Candinas R. Role of the sympathetic nervous system in the genesis of ventricular arrhythmia. Circulation. 1990; 82:2 Suppl. I103–I113.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download