Abstract
Purpose
Although several studies have reported the morphological and electrical characteristics in patients with hypertrophic cardiomyopathy (HCM), comparison between asymmetric and apical HCM has not been investigated in a reasonably sized cohort.
Materials and Methods
Echocardiography and electrocardiography were quantitatively analyzed in patients with HCM in a Korean tertiary referral center.
Results
Of 864 patients (mean age 55.4±14.2 years, 68.9% men), 255 (29.5%) patients had apical HCM, 553 (64.0%) patients asymmetric HCM, and 56 (6.4%) patients mixed type HCM. In echocardiographic evaluations, about three quarters of patients (75.8%) had left atrial enlargement. Left ventricular (LV) dilatations and systolic dysfunction were observed in 6.1% and 2.4%, respectively. QRS widening, PR prolongation, and pathologic Q wave are frequent in patients with asymmetric HCM, while LV strain is frequent in patient with apical HCM. The prevalence of J-point elevations (9.4% in inferior, 2.2% in lateral leads) were substantially higher than that in general population. Giant negative T wave was observed in 15.0% of total patients (32.2% in apical, 6.2% in asymmetric, 25% in mixed type). There was no significant correlation between the thickness of the apical wall and the amplitude of T wave inversion (r=-0.005, p=0.71).
The evaluation for hypertrophic cardiomyopathy (HCM) relies principally on echocardiography and electrocardiography. Historically, the evolution of echocardiography has demonstrated the important morphological characteristics such as asymmetric pattern, systolic anterior motion of the mitral valve, obstructive form, and apical involvement.1234 Therefore, echocardiography is considered as the gold standard for identifying the clinical phenotype of HCM.5 The electrocardiography also provides substantial information of HCM including mimic myocardial ischemia or infarction, and thereby creates diagnostic confusion.6789 However, most data were produced a long time ago and on the basis of relatively small population before the establishment of diagnostic consensus for HCM.1011 In addition, most data is about asymmetric HCM, while there are limited data on the apical HCM which was introduced later and was a relatively rare form in Western country.561213 We, therefore, investigated the morphological and electrical characteristics in a large Korean cohort, and they were compared among three HCM groups (asymmetric, apical, and mixed). It should be noted that we had already reported long-term survival between the two types of HCM.14
Our study enrolled patients with HCM who underwent echocardiography at a large tertiary referral center in Korea, between March 1996 and November 2005. We excluded 93 patients that had no electrocardiogram or otherwise unreadable traces. Thus, a total of 864 patients were enrolled. The diagnosis of HCM was based on the presence of a hypertrophied left ventricle in the absence of other diseases capable of producing the degree of observed hypertrophy. The patients were divided into three types (apical, asymmetric, and mixed) as an involved myocardium. The diagnostic criteria for apical HCM included demonstration of asymmetric left ventricular (LV) hypertrophy, confined predominantly to the LV apex with an apical wall thickness ≥15 mm and a ratio of maximal apical to posterior wall thickness ≥1.5, based on two-dimensional echocardiography.15 Asymmetric HCM was diagnosed in case of a septal-to-posterior (or posterior-to septal) wall thickness ratio of equal to or greater than 1.3.21617 Mixed type HCM was defined when a patient had a coexistent apical and asymmetric HCM. The 12-lead electrocardiograms for each of the eligible patients were obtained at the time of the initial evaluation for HCM. All electrocardiograms were retrospectively analyzed. The electrocardiographic parameters included heart rate, PR duration, corrected QRS duration, the presence of atrial fibrillation, the presence of pathologic Q wave, the presence of LV strain, the amplitude of T wave inversion in V4-6, and the amplitude of J-point elevation. LV strain was defined as ST-T segment vector shifted in direction opposite to the mean QRS complex.1819 Early repolarization patterns were stratified according to the degree of J-point elevation (<0.1 mV, 0.1-0.2 mV, or >0.2 mV) that was either notched or slurred in at least two consecutive anterior (V1-3), lateral (V4-6, I, aVL), or inferior (II, III, aVF) leads. A prolonged corrected QT interval was defined as at least 440 msec for men and at least 460 msec for women. A pathologic Q wave was defined as at least 25% or more of the height of the partner R wave and greater than 40 msec in width in at least two consecutive leads. The presence of atrial fibrillation was decided with the electrocardiography at the time of diagnosis of HCM. The electrocardiogram findings were compared among the three different HCM groups.
Categorical variables are presented as raw numbers and percentages, and were compared with the chi-square test or Fisher's exact test. Continuous variables are presented as mean±standard deviation and were compared by Kruskal Wallis test. A probability value <0.05 was considered statistically significant. SPSS for Windows (12.0, SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. This study was approved by the Institutional Review Board at Asan Medical Center, Seoul, Korea.
Baseline demographic and echocardiographic findings are summarized in Table 1, according to the type of HCM. Of 864 patients, 255 patients had apical HCM, 553 patients had asymmetric HCM, and 56 patients had mixed type HCM. The mean age was 55.4±14.2 years (from 12 to 92), and the patient with apical HCM was likely to be young compared to those with asymmetric HCM. The majority of patients were men. The proportion of patients with apical HCM increased in elder patients compared with stationary proportion of the patient with asymmetric and mixed type HCM (Fig. 1). Beta blocker was prescribed in about a half of patients, while 42.4% of patients had no medication. The patients with verapamil were 16.1%.
30.4% of patients with asymmetric HCM had resting LV outflow tract obstruction. About three quarters of patients (75.8%) had left atrial enlargement, defined as equal to or more than 40 mm of anterior-posterior diameter. LV dilatations, considered as more than 55 mm of LV internal diameter in diastole, were observed in 6.1% of total patients. It was more frequent in patients with apical HCM (12.2% in apical HCM, 3.1% in asymmetric HCM, and 8.9% in mixed type HCM, p<0.001, by Kruskal Wallis test). The prevalence of LV dilatation was increased with age (6.1% in total). Mean ejection fraction was within normal range, and LV systolic dysfunction, defined as equal to or less than 50%, was observed in 2.4% of patients. There were no difference of incidence according to the type of HCM. Deceleration time in patient with asymmetric HCM was longer than those with apical HCM. Prolonged deceleration time, considered as more than 220 msec, were prevalent in patient with asymmetric HCM (41.5% in total, 29.5% in apical HCM, 48.0% in asymmetric HCM, and 33.3% in mixed type HCM, p<0.001, by Kruskal Wallis test).
Electrocardiographic findings are summarized in Table 2. Patients with asymmetric HCM were likely to have long PR interval and long QRS duration. Wide QRS (17.7% vs. 4.7%, p<0.001) and PR prolongation (14.8% vs. 6.8%, p=0.003) were more prevalent in patients with asymmetric HCM compared to those with apical HCM. The prevalence of atrial fibrillation at the diagnosis was 8.1% (11.0% in apical HCM, 7.1% in asymmetric HCM, p=0.17), and it increased in elder patients.
Early repolarization, considered as more than 0.1 mV of J-point elevation, was found in 32.3% of anterior leads, 9.5% of inferior leads, and 2.2% of lateral leads. Significant J-point elevations, defined as more than 0.2 mV, were found in 12.7% (anterior leads), 2.9% (inferior leads), and 0.8% (lateral leads) of patients.
Patients with apical HCM were likely to have LV strain and deep negative T wave (Figs. 2 and 3). Giant negative T wave, defined as a negative T wave with depth ≥1 mV, was observed in 15.0% of total patients (32.2% in apical HCM, 6.2% in asymmetric HCM, 25% in mixed type HCM). In patients with apical HCM, there was no significant correlation between the thickness of the apical wall and the amplitude of T wave inversion (r=-0.005, p=0.71) (Fig. 4). Abnormal findings of electrocardiography were included the pattern of LV strain, longer than 480 msec of corrected QT interval, longer than 120 msec of PR interval, the presence of atrial fibrillation, the presence of LV strain, and more than 0.2 mV of the elevation of J-point. Their frequencies of abnormal findings according to the type of HCM are shown in Fig. 2. LV strain and QT prolongation were frequently observed in patients with HCM (68.9% and 52.5%, respectively).
In 864 Korean cohort of patients with HCM, significant electrical as well as morphological abnormalities were found. The major findings on electrical abnormalities were as follows; 1) more than half of patients had a repolarization abnormality presenting LV strain and QT prolongation, 2) giant negative T wave were observed in 15.0% of total patients, mostly patients with apical HCM, 3) the prevalence of wide QRS and PR prolongation were not infrequent, especially in patients with asymmetric HCM.
Echocardiographic evaluation revealed that the prevalence of apical HCM was increased with age until seventh decade, and substantial portion of patients had left atrial enlargement (75.8%) and deceleration time prolongation (41.5%), suggesting diastolic dysfunction.
HCM is a complex and relatively common genetic cardiac disorder.20 Although the majority of patients are asymptomatic, that is allowed to delayed diagnosis, some present with severe symptoms and some may even die suddenly because of fatal ventricular arrhythmia. LV obstruction by asymmetrical septal hypertrophy is the first discovered and a very specific finding in HCM.2122 Therefore, most morphological and electrical observations for HCM have been based on the population with these findings.679112324 However, the evolution of echocardiography demonstrated heterogeneous clinical phenotypes such as non-obstruction form and apical hypertrophy,14 and established the diagnosis of HCM.51125 However, there is a little data about morphological and electrical characteristics since the consensus for diagnosis and management of HCM were established. Especially, the differences of asymmetric HCM and apical HCM are hardly known.
In the demographic results, the patients with apical HCM were likely to be old compared to those with asymmetric HCM, and their prevalence was increased with age (Fig. 1). It is quite possible that almost all patients with apical HCM had no obstruction of the LV outflow tract and relatively benign prognosis. Although it was possible to be under-diagnosed in women of such a tertiary referral population, the majority of patients were men, in consistance with previous reports, especially in patients with apical HCM.1526 In the echocardiographic results, substantial portion of patients were likely to have diastolic dysfunction, and it was consistent with previous data.2728 In other word, systolic dysfunction suggesting burned out phase was rare at the time of diagnosis.1729 With age, the prevalence of LV dilatation was increased, while those of LV obstruction was decreased. Although these findings were derived from cross-sectional observation, it was supported by the previous reports for progressive LV remodeling in patients with HCM.293031
There are some uncertainties over medical treatment of the patients with HCM. While 40% of patients had no medication and near half of patients were prescribed beta blocker in our routine practice, it was highly dependent on individual situations such as symptom, compliance, and physician's discretion, which are not described in the present study. It is one of the limitations of the present study. However, the initiation and maintenance of pharmacologic treatment are largely subjected to patient's compliance and physician's discretion. Symptom and response for medication are highly variable in terms of magnitude and duration of benefit. Therefore, it is difficult to objectively categorize patient's symptom and medication.
Various electrocardiographic abnormalities were found in our study. They included LV strain, QT prolongation, QRS prolongation, PR prolongation, atrial fibrillation, and J point elevation more than 0.2 mV in anterior leads, and pathologic Q wave.
More than half of patients showed repolarization abnormality like LV strain (68.9%) and QT prolongation (52.5%). Reversal of the sequence of depolarization secondary to severe and localized LV hypertrophy was considered as mechanism of LV strain.32 LV strain was defined as ST-T segment vector shifted in direction opposite to the mean QRS complex in the present study, and it is similar to T wave inversion in other studies. It was reported that T wave inversion in the lateral leads is seen commonly in HCM. In the asymptomatic young athletes with HCM, 62% exhibited T wave inversion.33 Similarly, in HCM patients with a positive genetic test, 54% demonstrate T wave inversion.34 Our study confirmed that T wave inversion was common in patients with HCM and demonstrated that its prevalence was different as the type of HCM. Giant negative T wave was considered as classic electrocardiographic finding of HCM. However, it seemed not to be sensitive parameter of HCM, since only 14.8% of our patients showed giant negative T wave. No significant relationship between apical wall thickness and the degree of T wave inversion was found in the present study, in agreement with previous report.35
Recently, early repolarization has received attention for association with sudden cardiac death.36 Quantitative analysis showed that significant J wave elevation, more than 2 mV, was more frequently observed in patients with HCM (2.9% in inferior leads, 0.8% in lateral leads) than that previously reported in general population (0.3% in inferior leads, 0.3% in lateral leads).36 Clinical significance of repolarization abnormality in patients with HCM should be clarified in further longitudinal study. The prevalence of atrial fibrillation in our population was 8.1% (11.0% in apical, 7.1% in asymmetric, 5.4% in mixed type, mean age 55.4 years), much higher than that in Eastern general populations including Korean (0.7%, mean age 54.6 years),37 Japanese (1.6%, mean age 72.1 years),38 Hong Kong (1.3%, mean age 71 years)39 as well as in Western general population (0.95%, mean age 71 years).40 And it is comparable with that in Western HCM population (5% at the time of diagnosis, mean age 55 years).41 Atrial fibrillation in patients with HCM was challenging and associated with substantial risk for mortality and morbidity.41 In our results, only persistent atrial fibrillation might be detected, indicating an another limitation of our study: the prevalence of atrial fibrillation could be higher, about three times in a previous study, if paroxysmal atrial fibrillation was included.41
Our results had several limitations. First, we could not evaluate genetic analysis or magnetic resonance imaging for diagnostic test. Second, this study was based on the database of a tertiary referral center, and a community-based study is warranted to avoid referral bias.
This large Korean cohort of HCM including apical type demonstrated that repolarization abnormalities including early repolarization and QT prolongation as well as LV strain were significantly observed. T wave inversion was not appropriate for screening of HCM and not correlated with apical wall thickness.
Figures and Tables
 | Fig. 1Proportion of hypertrophic cardiomyopathy type relative to patient's age. In contrast to asymmetric hypertrophy, the proportion of patients with apical hypertrophy increased with age. |
 | Fig. 2Electrocardiographic abnormalities according to the type of hypertrophy. *Advanced electrical abnormalities such as QT prolongation, QRS widening, PR prolongation, and pathologic Q wave were more prevalent in patients with asymmetric hypertrophy. LV, left ventricle; QTc, corrected QT duration ≥480 msec; QRS, QRS duration ≥120 msec; PR, PR interval ≥200 msec; Q wave, pathologic Q wave; anterior J, J point in anterior leads ≥0.1 mV; inferior J, J point in inferior leads ≥0.1 mV; lateral J, J point in lateral leads ≥0.1 mV; AF, atrial fibrillation. |
 | Fig. 3The amplitude T wave inversion according to the type of hypertrophic cardiomyopathy. HCM, hypertrophic cardiomyopathy. |
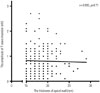 | Fig. 4Correlation between apical wall thickness and the amplitude of T wave inversion in patients with apical hypertrophy. No significant correlation was observed. |
Table 1
Demographic and Echocardiographic Characteristics

HCM, hypertrophic cardiomyopathy; LVOT, left ventricular outflow tract; IVSd, interventricular septum end diastole; IVSs, interventricular septum end systole; LVPWs, left ventricular posterior wall end systole; LVPWd, left ventricular posterior wall end diastole; LVIDs, left ventricular internal diameter end systole; LVIDd, left ventricular internal diameter end diastole.
Table 2
Electrocardiographic Findings

ACKNOWLEDGEMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A100909).
References
1. Abbasi AS, MacAlpin RN, Eber LM, Pearce ML. Echocardiographic diagnosis of idiopathic hypertrophic cardiomyopathy without outflow obstruction. Circulation. 1972; 46:897–904.

2. Henry WL, Clark CE, Epstein SE. Asymmetric septal hypertrophy. Echocardiographic identification of the pathognomonic anatomic abnormality of IHSS. Circulation. 1973; 47:225–233.
3. Pridie RB, Oakley C. Mitral valve movement in hypertrophic obstructive cardiomyopathy. Br Heart J. 1969; 31:390.
4. Sakamoto T, Tei C, Murayama M, Ichiyasu H, Hada Y. Giant T wave inversion as a manifestation of asymmetrical apical hypertrophy (AAH) of the left ventricle. Echocardiographic and ultrasono-cardiotomographic study. Jpn Heart J. 1976; 17:611–629.

5. Klues HG, Schiffers A, Maron BJ. Phenotypic spectrum and patterns of left ventricular hypertrophy in hypertrophic cardiomyopathy: morphologic observations and significance as assessed by two-dimensional echocardiography in 600 patients. J Am Coll Cardiol. 1995; 26:1699–1708.

6. Maron BJ, Wolfson JK, Ciró E, Spirito P. Relation of electrocardiographic abnormalities and patterns of left ventricular hypertrophy identified by 2-dimensional echocardiography in patients with hypertrophic cardiomyopathy. Am J Cardiol. 1983; 51:189–194.

7. Savage DD, Seides SF, Clark CE, Henry WL, Maron BJ, Robinson FC, et al. Electrocardiographic findings in patients with obstructive and nonobstructive hypertrophic cardiomyopathy. Circulation. 1978; 58(3 Pt 1):402–408.

8. Prescott R, Quinn JS, Littmann D. Electrocardiographic changes in hypertrophic subaortic stenosis which simulate myocardial infarction. Am Heart J. 1963; 66:42–48.

9. Cosio FG, Moro C, Alonso M, de la Calzada CS, Liovet A. The Q waves hypertrophic cardiomyopathy: an electrophysiologic study. N Engl J Med. 1980; 302:96–99.
10. Maron BJ, Maron MS, Wigle ED, Braunwald E. The 50-year history, controversy, and clinical implications of left ventricular outflow tract obstruction in hypertrophic cardiomyopathy from idiopathic hypertrophic subaortic stenosis to hypertrophic cardiomyopathy: from idiopathic hypertrophic subaortic stenosis to hypertrophic cardiomyopathy. J Am Coll Cardiol. 2009; 54:191–200.

11. Maron BJ, McKenna WJ, Danielson GK, Kappenberger LJ, Kuhn HJ, Seidman CE, et al. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol. 2003; 42:1687–1713.

12. Yamaguchi H, Ishimura T, Nishiyama S, Nagasaki F, Nakanishi S, Takatsu F, et al. Hypertrophic nonobstructive cardiomyopathy with giant negative T waves (apical hypertrophy): ventriculographic and echocardiographic features in 30 patients. Am J Cardiol. 1979; 44:401–412.

13. Chikamori T, Doi YL, Akizawa M, Yonezawa Y, Ozawa T, McKenna WJ. Comparison of clinical, morphological, and prognostic features in hypertrophic cardiomyopathy between Japanese and western patients. Clin Cardiol. 1992; 15:833–837.

14. Kim SH, Kim SO, Han S, Hwang KW, Lee CW, Nam GB, et al. Long-term comparison of apical versus asymmetric hypertrophic cardiomyopathy. Int Heart J. 2013; 54:207–211.

15. Eriksson MJ, Sonnenberg B, Woo A, Rakowski P, Parker TG, Wigle ED, et al. Long-term outcome in patients with apical hypertrophic cardiomyopathy. J Am Coll Cardiol. 2002; 39:638–645.

16. Otto CM. The practice of clinical echocardiography. 2nd ed. Philadelphia: W.B. Saunders;2002. p. 589.
17. Feigenbaum H, Armstrong WF, Ryan T. Feigenbaum's echocardiography. 6th ed. Philadelphia: Lippincott Williams & Wilkins;2005. p. 545.
18. Romhilt DW, Bove KE, Norris RJ, Conyers E, Conradi S, Rowlands DT, et al. A critical appraisal of the electrocardiographic criteria for the diagnosis of left ventricular hypertrophy. Circulation. 1969; 40:185–195.

19. Wagner GS, Marriott HJL. Marriott's practical electrocardiography. 10th ed. Philadelphia: Lippincott Williams & Wilkins;2001. p. 90–93.
20. Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults. Echocardiographic analysis of 4111 subjects in the CARDIA Study. Coronary Artery Risk Development in (Young) Adults. Circulation. 1995; 92:785–789.

21. Brock R. Functional obstruction of the left ventricle; acquired aortic subvalvar stenosis. Guys Hosp Rep. 1957; 106:221–238.
23. Braunwald E, Lambrew CT, Rockoff SD, Ross J Jr, Morrow AG. Idiopathic hypertrophic subaortic stenosis. I. A description of the disease based upon an analysis of 64 patients. Circulation. 1964; 30:Suppl 4. 3–119.

24. Maron BJ, Bonow RO, Cannon RO 3rd, Leon MB, Epstein SE. Hypertrophic cardiomyopathy. Interrelations of clinical manifestations, pathophysiology, and therapy (2). N Engl J Med. 1987; 316:844–852.
25. Maron BJ. Hypertrophic cardiomyopathy: a systematic review. JAMA. 2002; 287:1308–1320.
26. Louie EK, Maron BJ. Apical hypertrophic cardiomyopathy: clinical and two-dimensional echocardiographic assessment. Ann Intern Med. 1987; 106:663–670.

27. Ho CY, Sweitzer NK, McDonough B, Maron BJ, Casey SA, Seidman JG, et al. Assessment of diastolic function with Doppler tissue imaging to predict genotype in preclinical hypertrophic cardiomyopathy. Circulation. 2002; 105:2992–2997.

28. Maron BJ, Spirito P, Green KJ, Wesley YE, Bonow RO, Arce J. Noninvasive assessment of left ventricular diastolic function by pulsed Doppler echocardiography in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol. 1987; 10:733–742.

29. Maron BJ, Spirito P. Implications of left ventricular remodeling in hypertrophic cardiomyopathy. Am J Cardiol. 1998; 81:1339–1344.
30. Spirito P, Maron BJ, Bonow RO, Epstein SE. Occurrence and significance of progressive left ventricular wall thinning and relative cavity dilatation in hypertrophic cardiomyopathy. Am J Cardiol. 1987; 60:123–129.

31. Hina K, Kusachi S, Iwasaki K, Nogami K, Moritani H, Kita T, et al. Progression of left ventricular enlargement in patients with hypertrophic cardiomyopathy: incidence and prognostic value. Clin Cardiol. 1993; 16:403–407.

32. Tsunakawa H, Wei D, Mashima S, Harumi K. Study on the genesis of giant negative T wave in apical hypertrophic cardiomyopathy using a three-dimensional computer model. Jpn Heart J. 1991; 32:799–809.

33. Rowin EJ, Maron BJ, Appelbaum E, Link MS, Gibson CM, Lesser JR, et al. Significance of false negative electrocardiograms in preparticipation screening of athletes for hypertrophic cardiomyopathy. Am J Cardiol. 2012; 110:1027–1032.

34. Lakdawala NK, Thune JJ, Maron BJ, Cirino AL, Havndrup O, Bundgaard H, et al. Electrocardiographic features of sarcomere mutation carriers with and without clinically overt hypertrophic cardiomyopathy. Am J Cardiol. 2011; 108:1606–1613.

35. Park SY, Park TH, Kim JH, Baek HK, Seo JM, Kim WJ, et al. Relationship between giant negative T-wave and severity of apical hypertrophy in patients with apical hypertrophic cardiomyopathy. Echocardiography. 2010; 27:770–776.

36. Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA, et al. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med. 2009; 361:2529–2537.

37. Jeong JH. Prevalence of and risk factors for atrial fibrillation in Korean adults older than 40 years. J Korean Med Sci. 2005; 20:26–30.

38. Iguchi Y, Kimura K, Aoki J, Kobayashi K, Terasawa Y, Sakai K, et al. Prevalence of atrial fibrillation in community-dwelling Japanese aged 40 years or older in Japan: analysis of 41,436 non-employee residents in Kurashiki-city. Circ J. 2008; 72:909–913.

39. Lok NS, Lau CP. Prevalence of palpitations, cardiac arrhythmias and their associated risk factors in ambulant elderly. Int J Cardiol. 1996; 54:231–236.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download