Abstract
Purpose
Spontaneous pneumomediastinum (SPM) is a rare entity, with only a few cases reported, especially in adolescents. We aimed to analyze the clinical characteristics of SPM in adolescents and the diagnostic implications of computed tomography (CT) and esophagography therein.
Materials and Methods
This retrospective descriptive study was conducted as a review of medical records of 416 adolescents (10-18 years of age) with chest pain from March 2005 to June 2013. Information on clinical presentation, methods of diagnosis, hospital stay, and outcomes were collected and analyzed.
Results
Among adolescents complaining of chest pain, 11 patients had SPM (11/416, 2.64%). All patients presented with pleuritic chest pain, and 54.5% reported neck pain as the most common associated complaint. Clinical findings were nonspecific, and initial chest X-ray assessment was diagnostic only in three of 11 patients. However, reassessment of chest X-ray revealed diagnostic findings of SPM in five of the remaining eight patients. CT was diagnostic in all patients, while esophagography and echocardiogram were uninformative. Symptomatic improvement was noted within 2.45±1.2 hours (range, 0.5 to 4) after supportive care; mean hospital stay was 4.54±0.99 days (range, 2 to 6). No recurrence was observed.
Conclusion
SPM is a rare disease that should be considered in adolescent patients with pleuritic chest pain. Careful reading of initial chest X-rays is important to avoiding further unnecessary investigations. SPM is self-limited and treatment is supportive; nevertheless, if there are no indications of esophageal rupture, urgent esophagography is not recommended.
Spontaneous pneumomediastinum (SPM) is rare in pediatric practice, with an incidence of about 1/30000 emergency department referrals12 and an average age of 17.5 to 25 years.123 SPM is self-limiting and benign in nature, and it usually occurs in young healthy men without any trigger events or diseases.124 A pressure gradient exists between the peripheral pulmonary alveoli and the hilum, and increased intra-alveolar pressure causes rupture of the terminal alveoli.567 Alveolar rupture allows air to extend along the pulmonary vasculature towards the hilum, the peribronchial spaces, and subsequently, into the mediastinum.2 The most common symptoms at presentation are the acute onset of pleuritic or retrosternal chest pain and dyspnea. Because of its low incidence and its mild intensity, the diagnosis can be easily missed. According to the published reports, there have not been more than 25 patients with SPM at a single center.189 This study describes our experience with SPM, our efforts to analyze the clinical characteristics of adolescents with SPM, and the utility of urgent chest computed tomography (CT) and esophagography for the diagnosis of pneumomediastinum in adolescents.
We retrospectively reviewed the records of patients between the ages of 10 and 18 years who were discharged from Samsung Changwon Hospital with a diagnosis of SPM between March 2005 and June 2013. SPM was confirmed using plain chest X-ray or chest CT. We excluded the subjects with pneumomediastinum caused by the following trigger events: 1) positive pressure mechanical ventilation, 2) recent apparent trauma, 3) thoracic surgery, 4) endobronchial or esophageal procedures, 5) pneumothorax, 6) asthma exacerbation due to respiratory tract infection, and 7) lung parenchymal disease. Patients with a history of foreign body aspiration, those under the age of 10 years, and those older than 18 years were excluded. Although the average age of patients with SPM is known to range from 17.5 to 25 years,123 this study was designed to focus on young adolescents, who commonly present with chest pain requiring medical care from pediatricians or emergency doctors. Also, patients with connective tissue diseases, such as Marfan syndrome, were excluded.
Patient characteristics, past history, precipitating factors, clinical presentation, methods of diagnosis, treatment, length of hospital stay, and outcomes were reviewed. All parameters were expressed as mean±standard deviation. Approval of this retrospective study was obtained by the Institutional Review Board of our institution.
A total of 416 adolescent patients with chest pain visited our hospital at the emergency room or outpatient clinic during the study period. A total of 11 patients were diagnosed with SPM (11/416, 2.64%) during this period. There were 10 males and one female. The mean age at diagnosis was 15.96±1.5 years (range, 13.1 to 17.9 years) (Table 1). One patient was a smoker.
There were no apparent precipitating events, such as severe coughing, vigorous vomiting, or drug abuse. None of the patients had risk factors for venous thromboembolism. Also, none reported previous experience of either pneumomediastinum or pneumothorax. One patient had been swimming (not diving) three days before developing chest pain. None complained of upper respiratory tract symptoms, and no patient had a history of asthma. There was no evidence of severe malnutrition in any patient that would suggest anorexia nervosa. The mean time from developing chest pain to visiting the hospital was 8.3±2.9 hours (range, 5 to 15 hours), and three patients initially visited the outpatient clinic department. There were no cases of severe dyspnea or tachypnea, and the mean respiration rate was 18.7±3.3 (range, 16 to 28 per min). The main symptom complaint was sudden development of pleuritic chest pain, and it was not associated with positional change, respiration, or exercise.
The severity of chest pain was usually mild and was of a short duration. All patients experienced pleuritic chest pain, although three patients had no chest pain upon hospital presentation, and the mean duration of chest pain was 2.45±1.2 hours (range, 0.5 to 4 hours after supportive care). The most common symptom associated with chest pain was neck pain (6/11, 54.5%); others included sore throat (3/11, 27.3%), cough (3/11, 27.3%), odynophagia (1/11, 9.1%), and anxiety (1/11, 9.1%). The most common known physical examination finding of SPM is subcutaneous emphysema on the neck or chest wall upon palpation,3 which was observed in only one patient in this study. On physical examination, only three cases exhibited cardiac auscultation findings of distant heart sound, and there were no specific descriptions of lung sound in all cases.
When patients visited the hospital, an urgent chest radiograph was performed via postero-anterior and lateral chest radiographs in the upright position. Suspicion of SPM on initial chest X-rays was generated in three of 11 patients (Fig. 1); nevertheless, reinterpretation of the chest X-rays in this study revealed diagnostic findings of SPM in five of the remaining eight patients (Table 1). No finding was associated with pneumothorax on chest X-ray.
Chest CTs of all patients were analyzed to rule out pneumothorax, pneumopericardium, or pulmonary thromboembolism, and the mean time from visiting the hospital to checking the CT was 1.54±0.75 hours (range, 0.5 to 3). CT findings were diagnostic for all patients (Figs. 2 and 3), and there was no evidence of esophageal rupture.
Esophagography was performed in eight of 11 patients (72.7%), and there were no cases of esophageal leakage or rupture. Electrocardiography was performed for all patients, and there was no evidence of ST change or reduction in the amplitude of the QRS complex. Echocardiography was done in four of 11 patients to rule out pericardial effusion or pericarditis, and there were no specific findings. All patients were hospitalized for treatment and observation of their clinical course. The mean hospital stay was 4.54±0.99 days (range, 2 to 6 days) and supportive care included O2 inhalation, bed rest, and analgesics. There was no worsening of chest pain, and mediastinitis did not occur in any patient. When the patients were discharged, they were clinically and radiographically fully recovered from pneumomediastinum, according to chart review. There was no recurrence during the follow-up period.
This study was designed to investigate clinical manifestations of SPM in adolescents between the ages of 10 and 18 years, making it the first study of this age group, to the best of our knowledge.89 Published articles usually describe adult SPM,89 and there are only a few case reports about SPM in a young child and adolescents.71011 SPM is a rare disease that should be considered in adolescents with pleuritic chest pain. Due to the low incidence of this entity, there is no consensus on the most appropriate diagnostic approach and treatment. While careful reading of chest X-rays is important to avoid unnecessary studies, we wondered whether chest X-rays would be sufficient to diagnose this disease. Through our study, we discerned that urgent esophagography may not be recommendable if there are no clues of esophageal rupture among clinical or chest CT findings.
SPM or mediastinal emphysema is characterized by the presence of free air in the mediastinal tissue outside the esophagus without previous traumatic events. The mechanism underlying the development of SPM was described by Macklin and Macklin.6 According to the Macklin effect, a pressure gradient exists between the peripheral pulmonary alveoli and the hilum, and increased intra-alveolar pressure causes rupture of the terminal alveoli.567 Alveolar rupture allows air to extend along the pulmonary vasculature toward the hilum, into the peribronchial spaces and subsequently into the mediastinum.2
In most previous reports, the vital signs and general appearance of patients were normal, reflecting the benign course of SPM. Typically, SPM presents in young adults, and the incidence is low, occurring in about one in 30000 emergency department referrals.12 Among 416 patients, 319 patients initially presented to the emergency (76.7%) during the study period. Among 11 patients with SPM, three patients initially visited our outpatient clinic. Therefore, the incidence of SPM in our study was about eight out of 319 (2.5%) emergency department referrals. However, considering the low incidence of this disease, the incidence of SPM in our single-center experience was relatively high (11/416 adolescents with chest pain). This finding is probably related to the fact that our institution is the only tertiary medical center in Changwon City, which has a population of about one million people. In our study, this condition presented predominantly in men (10/11, 90.9%); this was also reported by Mondello, et al.3 in their review of 18 adult patients. The apparent precipitating factors of SPM are severe coughing, vigorous vomiting, asthma exacerbation, and drug abuse.378 In this study, no known triggers, such as history of asthma, presence of upper respiratory tract infection symptoms, or drug abuse, were noted. Purging behavior, such as self-induced vomiting, is common among anorexia nervosa patients, and severe vomiting is a known cause of pneumomediastinum. Therefore, anorexia nervosa patients with severe vomiting are thought to be at high risk for developing SPM; however, in most reports, pneumomediastinum in anorexic patients is not preceded by vomiting.12 Further, in this study, there was no indication of malnutrition or prolonged vomiting that would suggest anorexia nervosa.
Pleuritic chest pain is the most common symptom of SPM,3 and is found in up to 75% of patients.13 The chest pain is usually accompanied by dyspnea and dysphagia, occurring in 49% and 18%, respectively.13 Although the chest pain is typically retrosternal and may radiate to the neck, shoulders, and arms,314 there were no descriptions thereof in the chart review conducted in our study. This suggests that, first, chest pain of SPM may be localized without radiation to other sites and that, second, history taking, and physical examinations may not have been conducted carefully enough at the emergency room in this study. All patients in our study presented with one or more symptoms related to pneumomediastinum. The main symptom was pleuritic chest pain, and the most common associated symptom was neck pain (6/11, 54.5%), which was more common than that reported in another study (39%);13 others included sore throat (3/11, 27.3%), cough (3/11, 27.3%), odynophagia (1/11, 9.1%), and anxiety (1/11, 9.1%). Compared to a study by Sahni, et al.,13 there were fewer complaints of odynophagia (9.1% vs. 23%) and dyspnea (0% vs. 49%) prior to diagnosis of SPM in this study. Hamman's sign (crunching or dry crackling sound or crepitation synchronous with the heart beat on chest auscultation) is well known to be a pathognomonic sign of SPM.2 When reviewing the charts in this study, we only found one patient with crepitation on chest auscultation, and the patient had a diagnostic chest X-ray finding of SPM. The most common physical examination finding of SPM is subcutaneous emphysema on the neck or chest wall upon palpation,3 which was present in only one patient in this review. This was less common than that reported in another study (9.1% vs. 92%).15 The lack of presentations of Hamman's sign and subcutaneous emphysema in this study could be explained by missing documents or reduced attention during physical examinations for SPM at the emergency room: physical examinations can be normal in up to 30% of SPM patients.13161718 Hence, a normal physical examination never excludes a SPM.
Chest X-ray remains the gold standard diagnostic tool for SPM, and the sensitivity of postero-anterior and lateral chest radiographs is nearly 100%.1719 Patients with suspected pneumomediastinum should be checked with upright frontal and lateral chest X-ray, which should include the cervical region.192021 Chest X-rays are found to be falsely normal in up to 10-30% of patients, especially in supine radiographs.131720 Chest X-ray shows an air shadow within the mediastinum in the standard postero-anterior view, and the typical radiologic finding of pneumomediastinum is lucent streaks of gas that outline mediastinal structures, elevate the mediastinal pleura, and often extend into the neck or chest wall.222324 On the lateral view, lucent streaks may outline the ascending aorta, aortic arch, retrosternal, pre-cardiac, periaortic, and peritracheal areas.2125 Concerning the importance of carefully interpretation of chest X-rays in patients with chest pain, we emphasize the radiographic signs of pneumomediastinum. There are other several radiological signs to look for in suspected cases of SPM. First, if there is sufficient air within the mediastinum, the thymus can become elevated to produce a "thymic sail sign," which is more common in pediatric patients.1324 Second is a "continuous diaphragm sign," which is mediastinal gas outlining the superior surface of the diaphragm and separating it from the heart.23 Third, a "ring or ring around the artery sign" can be caused by air surrounding the intramediastinal portion of the pulmonary artery, especially the right pulmonary artery.1826 Additionally, the "V sign of Naclerio" can be caused by air outlining the lateral margin of the descending aorta, extending laterally between the parietal pleura and the medial left hemidiaphragm.18 If a definitive diagnosis can be made with a plain chest radiograph via these radiologic signs, no further testing is needed and the patients may be observed.13 Unfortunately, this study was retrospective design and a skillful radiologist was not included in this study, thus there were no specific descriptions of these radiographic findings in this study. Nevertheless, we emphasize the importance of these radiologic signs in patients with chest pain and that it is important to understand these signs and pay attention while interpreting chest X-rays for clinical physicians, especially pediatricians. In this study, there were only three of 11 patients with an initial finding of SPM on diagnostic chest X-ray, and reinterpretation of the X-rays during this study revealed diagnostic findings of SPM in five of the eight remaining patients. The low detection rate by chest X-ray was likely due to reduced attention in the interpretation of the chest X-ray at the initial checkup. This result suggests that the findings of pneumomediastinum on chest X-ray in the emergency department are easily missed due to their rare incidence, and it is important to carefully interpret the chest X-rays for adolescents with chest pain.
From the standpoint of accurate diagnosis, diagnosis of SPM can be easily made with chest CT because the anatomical location of the air is prominent on cross-sectional display. CT scanning is important to diagnoses in clinically suspected cases when chest X-ray is normal or equivocal. Of course, it may lead physicians to perform a greater number of CTs. However, for the differential diagnosis of chest pain in adolescents, it is important to check CT, depending on the established diagnostic workflow for patients highly suspicious of SPM.13 In other words, chest pain suspicious of SPM can be initially evaluated with a plain chest radiograph and results, after which further investigations such as CT may be ordered. Once again, careful reading of initial chest X-rays is important to preventing further unnecessary investigations. The mean time from visiting the hospital to checking the CT was 1.54±0.75 hours (range, 0.5 to 3) in this study. These findings indicate that fast and careless reading of chest radiographs can lead to an early aggressive CT study with consequent low rates of positive results. SPM can and must be distinguished from pneumomediastinum secondary to chest trauma, thoracic surgery, endobronchial or esophageal procedures, mechanical ventilation, and other invasive procedures.4 Even though SPM is relatively benign and self-limited, secondary pneumomediastinum due to esophageal perforation is a life-threatening disorder because of the development of fatal mediastinitis. The presentation of esophageal perforation, referred to as the Mackler triad, includes vomiting, chest pain, and subcutaneous emphysema. Because the symptoms are similar to those of SPM, the diagnosis of esophageal perforation is occasionally difficult. When it is difficult to rule out esophageal perforation on a CT, an esophagography should be considered for pneumomediastinum secondary to trauma. The addition of oral contrast to CT may increase the accuracy of detecting esophageal perforation and enable diagnosis of aerodigestive tract injury in patients with suspected pneumomediastinum via one single study.18 For SPM without apparent trauma history and with mild severity and immediately improved chest pain, the effectiveness of urgent esophagography should be considered. In this study, esophagography was done in eight of 11 patients, and there were no cases of esophageal leakage or rupture. Although our study showed only one patient with odynophagia and three patients with sore throat, esophagography was done in 8 patients. Also, all 11 CT findings showed no evidence of esophageal rupture. The reason for performing relatively high rate of esophagography in our study was probably related to a lack of diagnostic and treatment workflow for SPM during the study period in our hospital and a lack of understanding on the clinical course of SPM. Thus, there was much more fear about misdiagnosing esophageal rupture in SPM patients. However, according to our study and the report by Haam, et al.9 and Dissanaike, et al.,27 additional esophageal evaluation, such as esophagography or endoscopy, might be not useful in SPM patients without apparent history of esophageal injury or evidence of mediastinitis.
For better accuracy among diagnostic tools for pneumomediastinum, ultrasonography of the thorax has been increasingly used in the emergency department recently and can help in the diagnosis of pneumomediastinum.1828 Its usefulness, however, is limited because the diagnostic criteria for ultrasonography are not as well-established as those for ruling out pneumothorax.1828
Treatment for SPM is not specific, and it involves careful observation, bed rest, oxygen inhalation, and treatment with analgesics.8 Sometimes, antibiotic prophylaxis is used to prevent the development of mediastinitis.8 In this review study, there were no clear, concise algorithms for treatment and discharge. In this study, the time from the onset of chest pain to the medical service was relatively long [mean time of 8.3±2.9 hours (range, 5 to 15 hours)], and chest pain was typically mild severity and disappeared relatively quickly. For example, three patients had no chest pain when they visited the hospital, and the mean duration of chest pain was 2.45±1.2 hours (range, 0.5 to 4 hours after supportive care). The mean hospital stay was 4.54±0.99 days (range, 2 to 6 days), and supportive care included oxygen inhalation.
There was no worsening of chest pain during the hospital stay for any patient. When the patients were discharged, they were clinically and radiographically fully recovered from pneumomediastinum according to chart review. There was no recurrence during the follow-up period, suggesting that chest pain due to SPM has mild severity and a short duration.
Limitations to this study include its retrospective design and the small number of patients from a single, medium-sized hospital. Therefore, the results of our study may not allow generalization of the findings in SPM. However, SPM is a rare condition, and this study is the first to analyze its clinical characteristics in adolescents from a pediatrician's perspective. Multicenter collaborative study may clarify what discharge criteria should be used and the rationale for management that should be undertaken.
In conclusion, SPM is a rare self-limited condition with a benign natural course in young healthy adolescents. SPM should be considered in the diagnosis of adolescents with pleuritic chest pain. Careful interpretation of initial chest X-rays is important for avoiding unnecessary investigations. CT scanning is important to diagnosing clinically suspected cases when chest X-ray is normal or equivocal. If there are no clues for esophageal perforation, urgent esophagography is not recommended.
Figures and Tables
 | Fig. 1Spontaneous pneumomediastinum in a 16-year-old male patient. Postero-anterior radiograph demonstrates streaks of air outlining the mediastinal blood vessels, without evidence of rib fracture or pneumothorax. |
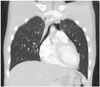 | Fig. 2Spontaneous pneumomediastinum in a 16-year-old male patient. Chest CT scan clearly demonstrating air within the superior mediastinum. |
 | Fig. 3Spontaneous pneumomediastinum in a 16-year-old male patient. Chest CT scan clearly demonstrating air within the superior mediastinum. |
Table 1
Clinical Characteristics of Patients with SPM

References
1. Abolnik I, Lossos IS, Breuer R. Spontaneous pneumomediastinum. A report of 25 cases. Chest. 1991; 100:93–95.
2. Newcomb AE, Clarke CP. Spontaneous pneumomediastinum: a benign curiosity or a significant problem? Chest. 2005; 128:3298–3302.
3. Mondello B, Pavia R, Ruggeri P, Barone M, Barresi P, Monaco M. Spontaneous pneumomediastinum: experience in 18 adult patients. Lung. 2007; 185:9–14.

4. Schulman A, Fataar S, Van der Spuy JW, Morton PC, Crosier JH. Air in unusual places: some causes and ramifications of pneumomediastinum. Clin Radiol. 1982; 33:301–306.
5. Panacek EA, Singer AJ, Sherman BW, Prescott A, Rutherford WF. Spontaneous pneumomediastinum: clinical and natural history. Ann Emerg Med. 1992; 21:1222–1227.

6. Wintermark M, Schnyder P. The Macklin effect: a frequent etiology for pneumomediastinum in severe blunt chest trauma. Chest. 2001; 120:543–547.
7. Bullaro FM, Bartoletti SC. Spontaneous pneumomediastinum in children: a literature review. Pediatr Emerg Care. 2007; 23:28–30.
8. Koullias GJ, Korkolis DP, Wang XJ, Hammond GL. Current assessment and management of spontaneous pneumomediastinum: experience in 24 adult patients. Eur J Cardiothorac Surg. 2004; 25:852–855.

9. Haam SJ, Lee JG, Kim DJ, Chung KY, Park IK. Oesophagography and oesophagoscopy are not necessary in patients with spontaneous pneumomediastinum. Emerg Med J. 2010; 27:29–31.

10. Ozdemir H, Kendirli T, Dinçaslan HU, Ciftçi E, Ince E. Spontaneous pneumomediastinum in a child due to 2009 pandemic influenza A (H1N1) virus. Turk J Pediatr. 2010; 52:648–651.
11. Takada K, Matsumoto S, Hiramatsu T, Kojima E, Watanabe H, Sizu M, et al. Management of spontaneous pneumomediastinum based on clinical experience of 25 cases. Respir Med. 2008; 102:1329–1334.

12. van Veelen I, Hogeman PH, van Elburg A, Nielsen-Abbring FW, Heggelman BG, Mahieu HF. Pneumomediastinum: a rare complication of anorexia nervosa in children and adolescents. A case study and review of the literature. Eur J Pediatr. 2008; 167:171–174.

13. Sahni S, Verma S, Grullon J, Esquire A, Patel P, Talwar A. Spontaneous pneumomediastinum: time for consensus. N Am J Med Sci. 2013; 5:460–464.

14. Banki F, Estrera AL, Harrison RG, Miller CC 3rd, Leake SS, Mitchell KG, et al. Pneumomediastinum: etiology and a guide to diagnosis and treatment. Am J Surg. 2013; 206:1001–1006.

15. Jougon JB, Ballester M, Delcambre F, Mac Bride T, Dromer CE, Velly JF. Assessment of spontaneous pneumomediastinum: experience with 12 patients. Ann Thorac Surg. 2003; 75:1711–1714.

16. Yellin A, Gapany-Gapanavicius M, Lieberman Y. Spontaneous pneumomediastinum: is it a rare cause of chest pain? Thorax. 1983; 38:383–385.

17. Kaneki T, Kubo K, Kawashima A, Koizumi T, Sekiguchi M, Sone S. Spontaneous pneumomediastinum in 33 patients: yield of chest computed tomography for the diagnosis of the mild type. Respiration. 2000; 67:408–411.

18. Mansella G, Bingisser R, Nickel CH. Pneumomediastinum in blunt chest trauma: a case report and review of the literature. Case Rep Emerg Med. 2014; 2014:685381.

19. Iyer VN, Joshi AY, Ryu JH. Spontaneous pneumomediastinum: analysis of 62 consecutive adult patients. Mayo Clin Proc. 2009; 84:417–421.

20. Rezende-Neto JB, Hoffmann J, Al Mahroos M, Tien H, Hsee LC, Spencer Netto F, et al. Occult pneumomediastinum in blunt chest trauma: clinical significance. Injury. 2010; 41:40–43.

21. Bejvan SM, Godwin JD. Pneumomediastinum: old signs and new signs. AJR Am J Roentgenol. 1996; 166:1041–1048.

22. Ba-Ssalamah A, Schima W, Umek W, Herold CJ. Spontaneous pneumomediastinum. Eur Radiol. 1999; 9:724–727.

23. Levin B. The continuous diaphragm sign. A newly-recognized sign of pneumomediastinum. Clin Radiol. 1973; 24:337–338.
24. Moseley JE. Loculated pneumomediastinum in the newborn. A thymic "spinnaker sail" sign. Radiology. 1960; 75:788–790.
25. Zylak CM, Standen JR, Barnes GR, Zylak CJ. Pneumomediastinum revisited. Radiographics. 2000; 20:1043–1057.
27. Dissanaike S, Shalhub S, Jurkovich GJ. The evaluation of pneumomediastinum in blunt trauma patients. J Trauma. 2008; 65:1340–1345.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download