Abstract
Purpose
Osteoarthritic (OA) pain is largely considered to be inflammatory pain. However, during the last stage of knee OA, sensory nerve fibers in the knee are shown to be significantly damaged when the subchondral bone junction is destroyed, and this can induce neuropathic pain. Several authors have reported that tumor necrosis factor-α (TNFα) in a knee joint plays a crucial role in pain modulation. The purpose of the current study was to evaluate the efficacy of etanercept, a TNFα inhibitor, for pain in knee OA.
Materials and Methods
Thirty-nine patients with knee OA and a 2-4 Kellgren-Lawrence grading were evaluated in this prospective study. Patients were divided into two groups; hyaluronic acid (HA) and etanercept injection. All patients received a single injection into the knee. Pain scores were evaluated before and 4 weeks after injection using a visual analogue scale (VAS) and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), and they were compared between the groups.
Results
Before injection, VAS and WOMAC scores were not significantly different between the groups (p>0.05). Significant pain relief was found in the etanercept group at 1 and 2 weeks by VAS, and at 4 weeks by WOMAC score, compared with the HA group (p<0.05). No adverse events were observed in either group.
Many patients suffer from knee osteoarthritis (OA) pin. In US, the patients with knee OA often results in early retirement and total knee arthroplasty.1 OA of the knee is generally considered to result in inflammatory pain. Intra-articular injection of monoiodoacetate into the knee joint of animals induces OA changes, and this model is widely used.2 In the early phase of this OA model, there is an increase in both inflammatory neuropeptides in the sensory nerves in the knee and several cytokines, and this is believed to be a stage of inflammatory pain.3 Subchondral bone pathology may result in neuropathy after destruction of the chondral structure during late phases of OA because of the dense innervation of subchondral bone. This stage is thought to be the neuropathic pain stage.4 Indeed, in human knee OA, the origin of OA pain is widely considered to be inflammatory, however, 6.7% to 34% of OA patients are likely to experience neuropathic pain.56
One of the sources of knee pain in OA is believed to be related to local chronic inflammation and sensory nerve injury of the knee joints, which involves the production of inflammatory cytokines such as tumor necrosis factor-α (TNFα), interleukin (IL)-6, and nerve growth factor (NGF) in the synovial membrane and subchondral bone; these cytokines are believed to promote pain from OA.789 TNFα and IL-6 concentrations in synovial fluid are correlated with knee OA progression and Western Ontario and McMaster Universitie's Osteoarthritis Index (WOMAC) scores, including a pain score, in patients with knee OA.7 Knee samples obtained from patients during surgery showed that sensory nerve fibers, cyclooxygenase, TNFα, and NGF are significantly increased, and these findings are closely related with the pathogenesis of pain.89
A systematic review of recommendations and guidelines for the management of knee OA has been reported.10 Pharmacologic modalities most recommended include acetaminophen/paracetamol (first-line) and non-steroidal anti-inflammatory drugs (NSAIDs) (topical or oral, second-line), and intra-articular corticosteroids are generally recommended for knee OA, while tramadol is recommended and consideration can be given to opioid treatment for refractory symptoms. However, these drugs sometimes have no effect on severe knee pain in knee OA patients.
Our hypothesis is that inhibition of cytokines is effective for moderate and severe OA pain in patients. Thus, the purpose of this study was to evaluate the efficacy of direct injection of etanercept into knee joints for knee OA pain in patients, by using a prospective trial.
The ethics committee of our institution approved the protocol for the human procedures used in this study. In addition, the protocol and publication of the study were approved by our institutional review board and informed consent was obtained from each participant (IRB No. 639). Participants were selected from outpatients who attended our hospitals for knee pain treatment. Thirty-nine patients were selected from 55 knee pain patients who matched the following criteria: the presence of knee pain for more than one month, evidence of OA of the knee joint upon examination of an anterior-posterior radiographic image, and oral NSAIDs administration of 200 mg of celecoxib per day (Pfizer Pharmaceutical Co., Ltd., Tokyo, Japan) was not fully effective for the knee pain. Exclusion criteria included a history of knee surgery, infection, or rheumatoid arthritis. We performed the screening protocol for tuberculosis using chest X-ray examination. If patients showed the possibility of pulmonary tuberculosis, they were excluded. Patient with heart failure, examined by ECG, was also excluded.
The patients completed a self-administered questionnaire related to sociodemographic factors (age and gender) and duration of knee symptoms.
All patients completed a visual analogue scale (VAS) evaluation of pain for movement (VAS: before, 1, 2, and 4 weeks after treatment), and the WOMAC questionnaire (WOMAC: before and 4 weeks after treatment). The WOMAC questionnaire consists of subsections for assessment of pain, stiffness, and physical function.11
Examination of an anterior-posterior view radiograph was performed for all the patients using the Kellgren-Lawrence (KL) grading system. The KL system is a validated method to classify joints into one of five grades, with 0 representing normal and 4 representing the most severe.12 Evaluation was performed by three blinded observers. If two or more of the observers concurred, the score was used to define the KL grade. Existence of increased synovial fluid was evaluated via a patella bollottement test performed by a single orthopaedic surgeon.
Thirty-nine knee OA patients were evaluated in this prospective study. Patients were divided into two groups: patients injected with 25 mg of hyaluronic acid (HA) (i.e., high molecular weight HA or Suvenyl®) (Chugai Pharmaceutical Co., Ltd., Tokyo, Japan), and patients injected with 10 mg of etanercept (Takeda Pharmaceutical Co., Ltd., Tokyo, Japan). Knee joint injections were performed once in all patients, with the first 20 patients being serially injected with HA and the next 19 patients being injected with etanercept. All patients continued to receive 200 mg of celecoxib daily. Other medications and injections into knees were not allowed in any patient.
All adverse events were reported together with an assessment of their severity (mild, moderate, or severe) and the investigator's opinion of their relationship to treatment with the administered drug (none, unlikely, possible, or probable).
The Kruskal-Wallis test was used to compare pain scales between the two groups, a one way ANOVA with post hoc comparisons for age, symptom duration, and follow-up, and Fisher's test for dichotomous/categorical variables. Data are re-ported as mean (±standard error of the mean) unless otherwise stated. p<0.05 was considered statistically significant.
No patients dropped out from the current study. Table 1 shows the demographic characteristics for patients. Thirty-nine patients (26 female, 13 male) with a mean age of 63.5±6.7 years were admitted into the study. The average duration of symptoms was 9.8±5.3 months. There was no significant difference in the number of patients, gender, age, or symptom duration between groups (p>0.05). Pain scores, as assessed using VAS and WOMAC scores, were also not significantly different between groups (p>0.05).
Table 2 shows evaluations of the KL grade and number of patients showing increased synovial fluid. There were no patients with KL grade 0 or 1, and all patients ranged from KL grade 2 to 4. The percentage and number of patients in each KL grade were not significantly different between groups (p>0.05). The number of patients showing increased synovial fluid included 8 patients (40%) in the HA group and 7 patients (37%) in the etanercept group. There was no significant difference in the number of patients showing increased synovial fluid between groups (p>0.05).
Table 3 shows reported pain during follow-up. Overall, both injections improved the pain score compared with pre-injection assessments. Significant pain relief was reported in the etanercept group, as assessed by the VAS score at 1 and 2 weeks and by the WOMAC score at 4 weeks, compared with the HA group (p<0.05). There was no significant pain relief experienced in the etanercept group as assessed by the VAS at 4 weeks, compared with the HA group (p>0.05).
In the current study, we investigated the efficacy of direct injection of etanercept for OA pain in OA patients, and found that etanercept was more effective for pain management than high molecular weight HA in OA patients. The finding suggests that TNFα is one of the factors that can induce pain in patients with OA.
Production of inflammatory cytokines such as TNFα, IL-6, and NGF in the synovial membrane and subchondral bone is believed to promote pain caused by OA.789 Indeed, some clinical trials have found that the most successful trial for treatment of OA pain reduction was anti-NGF therapy.1314 A total of 450 patients with OA pain received an intravenous injection of the anti-NGF antibody tanezumab or placebo.13 Treatment with tanezumab was significantly associated with a reduction in joint pain and improvement in function compared with placebo.13 Patients (n=83) with a KL grade of 2-4 were evaluated via radiographic assessment: by week 8, intravenous injection of tanezumab significantly improved knee pain and the WOMAC score compared with placebo,15 while seven patients reported adverse events of abnormal peripheral sensation such as allodynia, paresthesia, dysesthesia, thermohypoesthesia, and hypopallesthesia. When patients (n=604) with moderate to severe knee or hip OA were randomized and treated with intravenous tanezumab and placebo,14 tanezumab resulted in significant improvements in pain level, function, and global assessments in patients with OA compared with placebo, while osteonecrosis was reported in six patients treated with tanezumab.
Recently, it has been reported that compression and injury of spinal nerve roots are closely associated with cytokines such as TNFα and cyclooxygenase-2.1617 TNFα is the most widely used therapeutic target for radicular pain originating from lumbar disc herniation or spinal stenosis. A recent clinical study found that the TNFα inhibitor infliximab was effective for reducing sciatic nerve pain caused by lumbar disc herniation, and patients experienced no significant side effects.18 Similarly, results from our clinical studies indicate that the epidural administration of a TNFα inhibitor onto the spinal nerve provides relief of radicular pain with no adverse effects.19 Thus, TNFα inhibitors may be useful for the treatment of radicular pain caused by spinal stenosis.19
Beneficial effects of anti-TNFα therapy have also been reported in a single-arm, open-label clinical trial that evaluated adalimumab in 20 patients with OA over a 12-week period,20 and a significant improvement was observed in mean WOMAC pain, stiffness, and function, as well as target joint swelling at 12 weeks. Patients received six biweekly subcutaneous injections of 40 mg of adalimumab over 12 weeks.20 Furthermore, adverse events were minor with no serious events being recorded, and only one patient required an oral steroid for microscopic interstitial colitis. However, this study had limitations that included no placebo-controlled study design. In the current study, significant pain relief was reported in the group that received the single injection of etanercept as determined by VAS and the WOMAC score at 4 weeks, compared with the HA group. Based on these clinical findings, we recommend direct injection of anti-TNFα drug into the knee joint of patients who experience significant pain resulting from moderate to severe knee OA.
There are some limitations associated with the current study. First, we used only one drug dose in the two groups. In particular, we used a single injection of 10 mg of etanercept in this study. Generally, subcutaneous injection of 25-50 mg of etanercept is recommended for the treatment of rheumatoid arthritis in patients. However, we believe that direct injection of 25-50 mg of etanercept into the knee joint is excessive for OA patients and we were concerned about triggering adverse events. Therefore, we selected 10 mg of etanercept in this study. Second, we used a total of 39 patients, with 20 or less patients per group, and follow-up period was 1 month. This number of subjects does not provide sufficient power for the analyses required. Third, we think that etanercept has a strong effect for decrease of synovial fluid, although we examined synovial fluid only before injection. A future study, using a larger number of patients, longer follow-up, different drug dosages, multiple injection, and anti-inflammatory effect, is needed to clarify these points.
In conclusion, direct injection of etanercept, the TNFα inhibitor, was effective for pain manegement in OA patients. This finding also suggests that TNFα is one of the factors that can induce OA pain in patients.
Figures and Tables
Table 1
Patient Demographic Characteristics
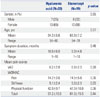
Table 2
Evaluations of Knee Conditions

Table 3
Change in Pain Scores

References
1. Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion. Arthritis types: overview. 2008. Available at: http://www.cdc.gov/arthritis/arthritis/osteoarthritis.htm.
2. van der Kraan PM, Vitters EL, van de Putte LB, van den Berg WB. Development of osteoarthritic lesions in mice by "metabolic" and "mechanical" alterations in the knee joints. Am J Pathol. 1989; 135:1001–1014.
3. Ochiai N, Ohtori S, Sasho T, Nakagawa K, Takahashi K, Takahashi N, et al. Extracorporeal shock wave therapy improves motor dysfunction and pain originating from knee osteoarthritis in rats. Osteoarthritis Cartilage. 2007; 15:1093–1096.

4. Ivanavicius SP, Ball AD, Heapy CG, Westwood FR, Murray F, Read SJ. Structural pathology in a rodent model of osteoarthritis is associated with neuropathic pain: increased expression of ATF-3 and pharmacological characterisation. Pain. 2007; 128:272–282.

5. Hochman JR, French MR, Bermingham SL, Hawker GA. The nerve of osteoarthritis pain. Arthritis Care Res (Hoboken). 2010; 62:1019–1023.
6. Ohtori S, Orita S, Yamashita M, Ishikawa T, Ito T, Shigemura T, et al. Existence of a neuropathic pain component in patients with osteoarthritis of the knee. Yonsei Med J. 2012; 53:801–805.

7. Orita S, Koshi T, Mitsuka T, Miyagi M, Inoue G, Arai G, et al. Associations between proinflammatory cytokines in the synovial fluid and radiographic grading and pain-related scores in 47 consecutive patients with osteoarthritis of the knee. BMC Musculoskelet Disord. 2011; 12:144.

8. Ogino S, Sasho T, Nakagawa K, Suzuki M, Yamaguchi S, Higashi M, et al. Detection of pain-related molecules in the subchondral bone of osteoarthritic knees. Clin Rheumatol. 2009; 28:1395–1402.

9. Walsh DA, McWilliams DF, Turley MJ, Dixon MR, Fransès RE, Mapp PI, et al. Angiogenesis and nerve growth factor at the osteochondral junction in rheumatoid arthritis and osteoarthritis. Rheumatology (Oxford). 2010; 49:1852–1861.

10. Nelson AE, Allen KD, Golightly YM, Goode AP, Jordan JM. A systematic review of recommendations and guidelines for the management of osteoarthritis: the chronic osteoarthritis management initiative of the U.S. bone and joint initiative. Semin Arthritis Rheum. 2014; 43:701–712.

11. Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988; 15:1833–1840.
12. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthritis. Ann Rheum Dis. 1957; 16:494–501.
13. Lane NE, Schnitzer TJ, Birbara CA, Mokhtarani M, Shelton DL, Smith MD, et al. Tanezumab for the treatment of pain from osteoarthritis of the knee. N Engl J Med. 2010; 363:1521–1531.

14. Balanescu AR, Feist E, Wolfram G, Davignon I, Smith MD, Brown MT, et al. Efficacy and safety of tanezumab added on to diclofenac sustained release in patients with knee or hip osteoarthritis: a double-blind, placebo-controlled, parallel-group, multicentre phase III randomised clinical trial. Ann Rheum Dis. 2014; 73:1665–1672.
15. Nagashima H, Suzuki M, Araki S, Yamabe T, Muto C. Tanezumab Investigators. Preliminary assessment of the safety and efficacy of tanezumab in Japanese patients with moderate to severe osteoarthritis of the knee: a randomized, double-blind, dose-escalation, placebo-controlled study. Osteoarthritis Cartilage. 2011; 19:1405–1412.

16. Ohtori S, Takahashi K, Aoki Y, Doya H, Ozawa T, Saito T, et al. Spinal neural cyclooxygenase-2 mediates pain caused in a rat model of lumbar disk herniation. J Pain. 2004; 5:385–391.

17. Olmarker K, Larsson K. Tumor necrosis factor alpha and nucleus-pulposus-induced nerve root injury. Spine (Phila Pa 1976). 1998; 23:2538–2544.
18. Korhonen T, Karppinen J, Malmivaara A, Autio R, Niinimäki J, Paimela L, et al. Efficacy of infliximab for disc herniation-induced sciatica: one-year follow-up. Spine (Phila Pa 1976). 2004; 29:2115–2119.
19. Ohtori S, Miyagi M, Eguchi Y, Inoue G, Orita S, Ochiai N, et al. Epidural administration of spinal nerves with the tumor necrosis factor-alpha inhibitor, etanercept, compared with dexamethasone for treatment of sciatica in patients with lumbar spinal stenosis: a prospective randomized study. Spine (Phila Pa 1976). 2012; 37:439–444.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download