Abstract
Purpose
To evaluate the effects of the deviation from the mid-sagittal plane, fetal image size, tissue harmonic imaging (THI), and speckle reduction filter (SRF) on the measurement of the nuchal translucency (NT) thickness using Volume NT™ software.
Materials and Methods
In 79 pregnant women, NT was measured using Volume NT™. Firstly, the three-dimensional volumes were categorized based on the angle of deviation in 10° intervals from the mid-sagittal plane. Secondly, the operator downsized the fetal image to less than 50% of the screen (Method A) and by magnifying the image (Method B). Next, the image was magnified until the fetal head and thorax occupied 75% of the screen, and the NT was measured (Method C). Lastly, NT values were acquired with THI and SRF functions on, with each function alternately on, and with both functions off.
Results
The mean differences in NT measurements were -0.09 mm (p<0.01) between two-dimensional (2D) and a deviation of 31-40° and -0.10 mm (p<0.01) between 2D and 41-50°. The intraclass correlation coefficients (ICC) for 2D-NT and NT according to image size were 0.858, 0.923, and 0.928 for methods A, B, and C, respectively. The ICC for 2D-NT and NT with respect to the THI and SRF were 0.786, 0.761, 0.740, and 0.731 with both functions on, THI only, SRF only, and with both functions off, respectively.
Measurement of nuchal translucency (NT) thickness during the first trimester has proven to be one of the single most effective screening tests for fetal chromosomal abnormalities.1 However, accurate image acquisition and appropriate training of imaging professionals are essential for effective NT screening. The Fetal Medicine Foundation (FMF) has provided guidelines in an effort to control image quality,2 and Herman, et al.3 suggested a novel image-scoring method, the Herman score, which demonstrated reliable and reproducible audit quality.
The reproducibility and compatibility of Volume NT™ software when compared with conventional two-dimensional (2D) and three-dimensional (3D) techniques has been proven in a previous study.4 Obtaining the NT measurement using the Volume NT™ program is a three-stage process: 1) acquisition of the fetal head volume in the sagittal plane; 2) automatic manipulation of the volume to yield the mid-sagittal plane; and 3) automatic vertical placement of the calipers along the widest part of the NT. Furthermore, given that image settings such as the angle of deviation from the mid-sagittal axis of the fetus, magnification status, tissue harmonic imaging (THI), and speckle reduction filter (SRF) influence NT measurements, these factors may also affect the precision of Volume NT™.5678 THI enables a sharper image to be obtained without degrading the image quality caused by using a low frequency in the NT measurement.8 Also, speckle should be filtered out to measure the exact NT value, as speckle can be a confounding factor in the captured ultrasound image.9
In light of these findings, the aim of this study was to evaluate the influence of magnification, angle of acquisition, THI, and SRF on NT measurements using Volume NT™.
The present study was approved by the Institutional Review Board of our institution. Between February 2011 and February 2012, normal singleton pregnancies at 11+0 to 13+6 weeks of gestation that were subjected to NT screening were enrolled. All fetuses included in this study presented normal NT values and normal neonatal outcomes. All 2D and Volume NT™ examinations were carried out transabdominally using an Accuvix V20 Prestige (Medison Co., Ltd., Seoul, Korea) ultrasound machine by a single expert (J.Y.K.) accredited by the FMF for the measurement of NT.
For the 2D ultrasound NT (2D-NT) measurements, a 2-6-MHz transabdominal transducer was used, while a 4-8-MHz volume transducer was used for 3D volume acquisition by Volume NT™. The crown-rump length (CRL) and the 2D-NT were measured according to the FMF protocol.2 The 3D volume was obtained in a sagittal sweep of the fetus to include the head and thorax and stored for later analysis.
Automatic NT measurement was performed off-line using Volume NT™ as described previously.4 Briefly, the stored 3D volume was archived, and Volume NT™ was activated to yield a reconstructed mid-sagittal section. A box caliper was then placed manually at the posterior region of the fetal neck to activate automatic caliper placement at the widest NT.
After obtaining a mid-sagittal section of the fetus with the transducer placed parallel to the nasal bone, the operator rotated the transducer sideways to an arbitrary angle in the range of 0-90°, and the 3D volume was acquired. When the 3D volume was reconstructed using Volume NT™ to precisely determine the mid-sagittal plane, the angle of deviation from the mid-sagittal plane was automatically calculated. The 3D volumes were categorized by the angle of deviation in 10° intervals in order to evaluate the influence of the angle of acquisition on the precision of Volume NT™. The success rate was calculated from 79 cases where NT measurements were possible at each angle deviation using Volume NT™.
The following magnification conditions were used to evaluate the effects of magnification on the NT measured automatically using Volume NT™ (Fig. 1):
1) Automated mid-sagittal section reconstruction and automated caliper placement with the fetal head and thorax occupying less than 50% of the image (method A).
2) Automated mid-sagittal section reconstruction at low magnification, zoomed-in to magnify the fetus so that it occupied the whole screen and followed by automated caliper placement (method B).
3) Automated mid-sagittal section reconstruction and automated caliper placement with the fetal head and thorax occupying the whole screen (method C).
THI and a SRF were applied in order to evaluate the effect of noise reduction functions when using Volume NT™ (Fig. 2). Values of 2D-NT with THI were acquired after achieving the best image quality by adjusting the depth, gray scale, gain, frame rate, focus, and magnification on conventional ultrasonography. Next, THI and SRF were used when acquiring the 3D volume using Volume NT™. These 3D volumes were acquired with both functions on, with each function on individually, and without either of the two functions. We measured the NT value using Volume NT™ on each of these four original images.
Data were analyzed using the Kolmogorov-Smirnov test to confirm that they were normally distributed. To determine if there were differences in the NT values according to the angle of deviation, the mean difference values were compared with a paired t-test. Next, intraclass correlation coefficients (ICC) were used to examine the degree of agreement between 2D measurements and Volume NT™ measurements based on each image size and setting. In addition, mean differences among the values from 2D and Volume NT™ measurements were assessed using Bland-Altman plots. Continuous variables are presented as means±standard deviations (SDs). p-values less than 0.05 were considered statistically significant. Statistical analysis was carried out using SPSS version 18.0 (SPSS Inc., Chicago, IL, USA).
The characteristics of the 79 enrolled patients are summarized in Table 1. The mean NT thickness was 1.31 (±0.43) mm on 2D ultrasound, and this value was considered to be the NT value at the true mid-sagittal plane. The mean fetal NT thickness decreased as the deviation angle increased (Table 2), while the NT measurement success rate using Volume NT™ also decreased. However, Volume NT™ did succeed in acquiring the mid-sagittal plane and measuring the NT value for all cases up to a deviation angle of 30°; nevertheless, it failed in three cases (3.8%) for deviation angles ranging from 31° to 40°. Moreover, Volume NT™ was unable to obtain NT measurements for 78 cases (98.7%) at deviation angles from 51° to 60°. Four cases of NT measurement failure occurred at the stage of automated mid-sagittal plane acquisition, and once the mid-sagittal plane was acquired with Volume NT™, NT measurement could be completed after placing the box caliper at the fetal posterior neck. Therefore, we believe that the angle of deviation from the mid-sagittal plane has more of an effect on the success of Volume NT™ during acquisition of the mid-sagittal plane.
The mean differences in the NT measurements between 2D and 3D imaging were -0.09 mm (-0.14, -0.03; p<0.01) at a deviation of 31-40° and -0.10 mm (-0.17, -0.03; p<0.01) at a deviation of 41-50°. Therefore, the NT value at a deviation angle greater than 31° was statistically different from the 2D-NT measurement (Table 2). Table 3 shows the mean 2D and Volume NT™ measurements with respect to magnification. Measurements obtained using methods B and C showed greater correlation with the 2D-NT measurement than method A, and the Bland-Altman plots confirmed these results (Fig. 3).
Lastly, we evaluated the effect of THI and SRF on Volume NT™. Table 4 shows the mean values obtained using the 2D image and Volume NT™ with respect to each function. The 2D-NT values and those obtained using Volume NT™ with THI and SRF were more highly correlated than the other function conditions, and the lowest correlation between values was obtained when neither THI nor SRF were used (Fig. 4).
This study suggests that Volume NT™ showed better correlation with 2D values when measured with a fetal head deviation of less than 30 degrees. When measuring NT with Volume NT™, images should be magnified before setting the mid-sagittal plane or measuring NT according to FMF guidelines. Lastly, 2D-NT values correlated highly with NT measurements taken by Volume NT™ with THI and SRF.
Obtaining a proper fetal nuchal translucency plane for first trimester scanning requires a well-trained technician. This is the most important component of the screening procedure for achieving reproducible and standardized results. The importance of the mid-sagittal plane in NT measurement has been emphasized by many authors,510 and NT measurement with Volume NT™ is no exception, as overestimated NT measurements lead to increased false-positive rates whereas underestimated NT values lead to decreased detection rates of trisomy 21.9 Recently, use of Volume NT™ has been shown to be effective in overcoming operator-dependency compared with conventional methods. Volume NT™ has many advantages such as high agreement with 2D-NT, more constant results, easy identification of the exact mid-sagittal plane, and time effectiveness in NT screening; thus, it is helpful for inexperienced operators.4
Previously, we observed that, in cases with large insonation angle deviations of over 30° from the mid-sagittal plane at the time of volume sweep, fetal movements during volume acquisition, absence of amniotic fluid in front of the face, close contact of the fetal neck with the uterine wall, and acoustic shadowing in the NT region caused by the maxilla led to unsuccessful or incorrect NT measurements using Volume NT™.4 However, exact guidelines for the effective use of Volume NT™ in the context of the plane of acquisition and image settings have not been established.
In this study, we evaluated the effects of the plane of acquisition, degree of magnification, and the influence of THI and SRF on measuring NT using Volume NT™. The underestimation of fetal NT thickness determined using Volume NT™ increased as the deviation angle increased. The fetal NT values at a deviation angle greater than 40° from the mid-sagittal plane were significantly underestimated compared with the 2D measurement.
Abele, et al.5 obtained the 3D volume in the exact mid-sagittal plane of the fetus and measured each NT thickness by rotating the head from 5° up to 25°. They found that the NT value using the 3D volume was reduced by about 7% at a deviation of 5° and the NT thickness could be measured at up to 25° of deviation from the mid-sagittal plane. Furthermore, Wah, et al.10 reported that when eight operators obtained a mid-sagittal plane using 3D volume, the mean angle of deviation was 5.7°, resulting in an NT underestimation of 1.8%, although this did not reach statistical significance. As shown by our results, NT measurements did not have an effect on screening results while the angle of deviation remained less than 30°. Deviation angles ranging from 31° to 40° and from 41° to 50° were related with a decrease in the fetal NT measurement by 0.7 and 0.8 mm, respectively.
In addition, we demonstrated that the mean NT without magnification according to FMF guidelines differed significantly from the 2D NT measurement. Therefore, it is important to magnify images according to the FMF guidelines when using Volume NT™. Herman, et al.11 reported that NT measurement is significantly affected by fetal image size despite their finding that the effect of image size was negligible. Edwards, et al.6 showed that changes in image magnification from 60% to 100% to 200% resulted in a constant decrease in the mean NT measurement. Another study demonstrated that 200% image magnification led to a significant reduction in the screen-positive rate.7 Both of these studies suggest that higher magnification results in greater pixelation and lower image resolution, subsequently resulting in blurring, which in turn makes the two NT margins look thicker and thereby causes relatively underestimated NT.7 Therefore, automatic techniques for enhancement of border detection have been developed to supplement manual methods.12
We obtained the smallest NT value when using an unmagnified fetal image or an image with a magnification of less than 50%, which is in contrast to previous studies. One reason for this discrepancy could be due to the use of an independent program algorithm by Volume NT™ for NT margin detection, which may be less affected by weak edges than manual methods. Furthermore, the two previous studies mentioned above reprocessed images acquired according to FMF guidelines at 200% magnification, which then needed gain correction8 to correct the blurred margin, whereas we used images without further processing.
We also demonstrated that NT measurements processed using THI and SRF in Volume NT™ showed similar agreement with 2D NT measurements. Among the four settings used in our study, THI and SRF resulted in the highest correlation with the 2D-NT values. However, the actual clinical significance is likely low as the mean differences were very small. The absolute paired differences were 0.2 mm when using SRF alone, and all others were less than 0.1 mm (data not shown). Moreover, the SRF function caused an overestimation of the NT measurement using Volume NT™; thus, the use of SRF should be consistent. The THI and SRF used in this study were acceptable to the clinician as these differences were not extreme. We found that the NT values varied: the NT value decreased when THI was used, whereas it increased when SRF was used. This result was in line with a previous study of 2D-NT measurements.8 The use of THI with conventional 2D ultrasound technique is associated with underestimation of NT measurement. Furthermore, one study on image setting using semi-automated methods developed by another ultrasound company also showed that the use of THI significantly reduced the NT values.13 However, further study is necessary to determine other effects of image settings that were not examined in this study, such as gain, gray map, contrast, etc., in addition to different combinations of these settings.
In conclusion, for optimal results using the Volume NT™ program, we suggest that operators ensure that the sagittal volume is initiated at a plane deviated less than 30° from the precise mid-sagittal plane. Additionally, the fetus should be properly magnified prior to either volume acquisition or automated caliper placement. Moreover, use of THI and SRF settings correlated with better 2D-NT measurements.
Figures and Tables
 | Fig. 1Representative images of nuchal translucency (NT) thickness measurements using Volume NT™ at three different magnifications: (A and B) automated NT measurement with the fetal head and thorax occupying less than 50% of the image (method A); (C and D) automated mid-sagittal reconstruction in low magnification then zoomed-in to magnify the fetus so as to occupy the whole screen (method B); (E and F) automated NT measurement with fetal head and thorax occupying the whole screen (method C). |
 | Fig. 2Images of effects of tissue harmonic imaging (THI) and speckle reduction filter (SRF): (A) THI and SRF functions on; (B) THI function on; (C) SRF function on; (D) both functions off. |
 | Fig. 3Bland-Altman plots of the variability of nuchal translucency (NT) thickness measurements. (A) Using two-dimensional (2D) ultrasound and method A of Volume NT™, (B) 2D ultrasound and method B, and (C) 2D ultrasound and method C. Dotted lines represent mean±2 SD. US, ultrasonography. |
 | Fig. 4Bland-Altman plots of the variability of nuchal translucency (NT) thickness measurements. (A) Using two-dimensional (2D) ultrasound and the tissue harmonic imaging (THI) and speckle reduction filter (SRF) features of Volume NT™, (B) 2D ultrasound and THI of Volume NT™, (C) 2D ultrasound and SRF of Volume NT™, and (D) 2D ultrasound and both functions off. Dotted lines represent mean±2 SD. US, ultrasonography. |
Table 1
Characteristics of the Study Population (n=79)
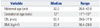
| Variable | Median | Range |
|---|---|---|
| Maternal age (yrs) | 32.0 | 26.0-42.0 |
| Gestational age (wks) | 12+1 | 11+0-13+6 |
| CRL (mm) | 55.1 | 39.0-77.9 |
| BMI (kg/m2) | 20.4 | 16.4-29.0 |
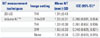
Table 2
Comparison of NT Measurements According to Angle Deviation from the Mid-Sagittal Plane (n=79)

Table 3
Mean NT Measurements and ICC for NT Measurements Using 2D and Image Size

Table 4
Comparison of NT Measurements According to THI and SRF
ACKNOWLEDGEMENTS
The Research and Development Center of Medison contributed to the development of the algorithm for the Volume NTTM program. Part of this work by Dr. J.Y. Kwon was supported by a grant from the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare & Family Affairs, Republic of Korea (A084120).
References
1. Nicolaides KH, Azar G, Byrne D, Mansur C, Marks K. Fetal nuchal translucency: ultrasound screening for chromosomal defects in first trimester of pregnancy. BMJ. 1992; 304:867–869.
2. The Fetal Medicine Foundation. Downs screening at 11 to 14 weeks. accessed on 2014 June. Available at: https://fetalmedicine.org/.
3. Herman A, Dreazen E, Maymon R, Tovbin Y, Bukovsky I, Weinraub Z. Implementation of nuchal translucency image-scoring method during ongoing audit. Ultrasound Obstet Gynecol. 1999; 14:388–392.
4. Cho HY, Kwon JY, Kim YH, Lee KH, Kim J, Kim SY, et al. Comparison of nuchal translucency measurements obtained using Volume NT(TM) and two- and three-dimensional ultrasound. Ultrasound Obstet Gynecol. 2012; 39:175–180.
5. Abele H, Wagner N, Hoopmann M, Grischke EM, Wallwiener D, Kagan KO. Effect of deviation from the mid-sagittal plane on the measurement of fetal nuchal translucency. Ultrasound Obstet Gynecol. 2010; 35:525–529.

6. Edwards A, Mulvey S, Wallace EM. The effect of image size on nuchal translucency measurement. Prenat Diagn. 2003; 23:284–286.

7. Teoh M, Meagher SE, Choong S, Shekleton P, Wallace EM. The effect of image size on screen-positive rates for nuchal translucency screening. BJOG. 2006; 113:479–481.

8. Pasquini L, Tondi F, Rizzello F, Pontello V, Paoletti E, Fontanarosa M. Impact of tissue harmonic imaging on measurement of nuchal translucency thickness. Ultrasound Obstet Gynecol. 2010; 36:423–426.
9. Munteanu C, Morales FC, Fernández JG, Rosa A, Déniz LG. Enhancing obstetric and gynecology ultrasound images by adaptation of the speckle reducing anisotropic diffusion filter. Artif Intell Med. 2008; 43:223–242.
10. Wah YM, Chan LW, Leung TY, Fung TY, Lau TK. How 'true' is a true midsagittal section? Ultrasound Obstet Gynecol. 2008; 32:855–859.

11. Herman A, Maymon R, Dreazen E, Caspi E, Bukovsky I, Weinraub Z. Image magnification does not contribute to the repeatability of caliper placement in measuring nuchal translucency thickness? Ultrasound Obstet Gynecol. 1998; 11:266–270.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download