Abstract
Purpose
Bridge anticoagulation therapy is mostly utilized in patients with mechanical heart valves (MHV) receiving warfarin therapy during invasive dental procedures because of the risk of excessive bleeding related to highly vascular supporting dental structures. Bridge therapy using low molecular weight heparin may be an attractive option for invasive dental procedures; however, its safety and cost-effectiveness compared with unfractionated heparin (UFH) is uncertain.
Materials and Methods
This study investigated the safety and cost-effectiveness of enoxaparin in comparison to UFH for bridge therapy in 165 consecutive patients (57±11 years, 35% men) with MHV who underwent invasive dental procedures.
Results
This study included 75 patients treated with UFH-based bridge therapy (45%) and 90 patients treated with enoxaparin-based bridge therapy (55%). The bleeding risk of dental procedures and the incidence of clinical adverse outcomes were not significantly different between the UFH group and the enoxaparin group. However, total medical costs were significantly lower in the enoxaparin group than in the UFH group (p<0.001). After multivariate adjustment, old age (≥65 years) was significantly associated with an increased risk of total bleeding independent of bridging methods (odds ratio, 2.51; 95% confidence interval, 1.15-5.48; p=0.022). Enoxaparin-based bridge therapy (β=-0.694, p<0.001) and major bleeding (β=0.296, p=0.045) were significantly associated with the medical costs within 30 days after dental procedures.
Patients with mechanical heart valves (MHV) are at the highest risk for thromboembolism without anticoagulation; therefore, lifelong oral anticoagulation (OAC) treatment is mandatory for preventing thromboembolic events.1,2,3 However, temporary discontinuation of long-acting OAC drugs (e.g., warfarin) may be inevitable to allow patients with MHV to undergo an invasive dental procedure or surgery. The recommendation for the management of OAC in minor dental procedures such as simple dental extraction has been proposed on the basis of clinical data; however, a consensus on which patients require invasive dental procedures is lacking.4,5,6 In clinical practice, conventional care with a short-acting anticoagulant as "bridge therapy" is commonly used to decrease the risk of thromboembolism during the cessation of OAC therapy.7,8,9 Intravenous unfractionated heparin (UFH) is the conventional medication used for bridging; however, it can be expensive and time-consuming, because periprocedural hospitalization for administering and laboratory monitoring is imperative. Despite the higher drug price of low molecular weight heparin (LMWH) compared with UFH, LMWH may be an attractive option for bridge therapy because it is relatively short-acting, requires no coagulation monitoring, and can be self-administered by the patient without hospitalization. However, there are only limited clinical data for the safety and medical costs of LMWH as bridge therapy for dental procedures that are associated with a moderate to high bleeding risk in patients with MHV. The present study compared the safety and cost-effectiveness between enoxaparin and UFH for bridge therapy in MHV patients receiving long-term warfarin therapy who were to undergo invasive dental procedures and who posed a moderate to high bleeding risk.
We analyzed clinical data from 169 consecutive patients with MHV receiving long-term OAC therapy with warfarin. Between January 2008 and December 2011, the patients visited the Severance Dental Hospital (Seoul, Korea) for elective invasive dental procedures. Only patients with stable anticoagulation status and general status were included. Patients (n=4) who had undergone mechanical valve surgery within the previous 3 months were excluded. We finally enrolled 165 patients in this study. The study protocol was approved by the local ethics committee of our institution. Each patient provided informed consent for the procedure.
All patients stopped taking warfarin 4 days before their dental procedures, and they received bridge therapy with UFH or enoxaparin during the temporary cessation of warfarin. Initial bridge therapy started 24 to 36 h after the last dose of warfarin, irrespective of the bridging method. All patients treated with UFH-based bridging were hospitalized to maintain the activated partial thromboplastin time between 1.5 to 2.5 times the control values during the intravenous administration of weight-adjusted UFH. Enoxaparin-based bridge therapy was performed on an outpatient basis. A therapeutic dose of enoxaparin (1 mg/kg) was subcutaneously administered twice daily. Warfarin was resumed 12 to 24 h after the dental procedure, and the bridge therapy was continued until the international normalized ratio was in the therapeutic range (more than 2.0 for most cases) for at least 2 consecutive days. Total medical costs were calculated for the period beginning 10 days before and lasting until 30 days after the dental procedures. The HAS-BLED score, which is a useful predictor of major bleeding, was calculated for all patients before their dental procedures.10 The bleeding risk of dental procedures was categorized as moderate or high. Dental procedures with moderate bleeding risk included restorations with subgingival preparations (n=54), standard root canal therapy (n=36), simple extractions (n=46), and regional injection of local anesthesia (n=80). Dental procedures with high bleeding risk included extensive surgery (n=2), apicoectomy (root removal) (n=1), alveolar surgery (bone remove) (n=5), and multiple extractions (n=51). Multiple procedures involving different bleeding risks were performed simultaneously in patients receiving bridge therapy; the more invasive dental procedure was considered the main procedure. Dental procedures with a low bleeding risk (e.g., supragingival scaling, local anesthetic injection, and simple restorations) were excluded in the present study.
Major bleeding was defined as overt bleeding with 2 g/dL or greater decrease in hemoglobin, a transfusion of 2 U or more packed red blood cells, bleeding that required surgical intervention, or life-threatening bleeding. Minor bleeding was defined as any bleeding that was self-limiting such as epistaxis, ecchymoses, hematoma, or an incision site bleeding that did not require withholding anticoagulation therapy.11
Clinical characteristics are presented, based on the bridge therapy method used. Values are expressed as the mean±standard deviation for continuous variables and as numbers and percentages [i.e., n (%)] for categorical variables. Continuous variables were compared using Student's t-test, and categorical variables were compared using Fisher's exact test or χ2 test. Multivariate logistic regression analysis was used to evaluate the clinical risk factors for total bleeding within 30 days after dental procedures. Multivariate linear regression analysis was used to evaluate the clinical factors for medical costs. The dependent variable of medical cost was transformed with the natural logarithm function. SPSS software version 18 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses. All statistical tests were 2-tailed and p<0.05 was considered significant.
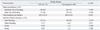
Table 1 presents the baseline characteristics of the 165 patients (57±11 years, 35% men) with MHV in this study. Of the 165 patients, 75 (45%) patients were treated with UFH-based bridge therapy, and 90 (55%) patients were treated with enoxaparin-based bridge therapy. The mean body mass index (BMI) and the HAS-BLED score were significantly higher in the enoxaparin group than in the UFH group (BMI: 23.5±3.4 vs. 22.1±3.3, p=0.006; HAS-BLED score: 1.5±1.2 vs. 1.1±1.0, p=0.018). The incidence of non-steroidal anti-inflammatory drugs was significantly higher in the enoxaparin group than in the UFH group (20% vs. 5%, p=0.006).
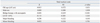
The bleeding risk of the dental procedures was not significantly different between the UFH group and the enoxaparin group. The incidence of clinical adverse outcomes including total bleeding, major bleeding, stroke, and death was not significantly different between the UFH group and the enoxaparin group. However, medical costs were significantly higher in the UFH group than in the enoxaparin group $2227±$3133 vs. $699±$1503, p<0.001) (Table 2).
Multivariate logistic regression analysis for clinical factors associated with total bleeding within 30 days after dental procedures revealed that enoxaparin was not significantly associated with total bleeding after dental procedures [odds ratio (OR), 0.64; 95% confidence interval (CI), 0.29-1.44; p=0.280]. Old age (≥65 years) was an independent clinical factor associated with an increased risk of total bleeding after dental procedures (OR, 2.51; 95% CI, 1.15-5.48; p=0.022) (Table 3).
Multivariate linear regression analysis revealed that bridge therapy with enoxaparin (β=-0.694, p<0.001) and major bleeding (β=0.296, p=0.045) were clinical factors significantly associated with medical costs within 30 days after dental procedures (Table 4).
The present study demonstrated that in patients with MHV who underwent invasive dental procedures, enoxaparin-based bridge therapy had a similar complication rate but was more cost-effective than UFH-based bridge therapy. Old age (i.e. ≥65 years) was significantly associated with total bleeding within 30 days after the dental procedures, independent of the type of bridge therapy.
With respect to dental procedures or surgeries, optimal management varies considerably for patients at high risk of thromboembolism receiving long-term OAC.4,5,6 Periprocedural anticoagulation therapy is especially important in patients with MHV receiving long-term OAC, since they have the highest annualized risk of thromboembolic complications in the absence of anticoagulation therapy.2 A previous meta-analysis study reported that maintaining a regular dose of warfarin may not confer an increased bleeding risk as opposed to interrupting or modifying the warfarin dose for patients who undergo minor dental procedures.12 The American College of Chest Physicians guidelines also recommended continuing warfarin around the time of dental procedures in patients receiving long-term OAC.13 However, the safety of maintaining warfarin during invasive dental procedures remains unclear, especially in patients with MHV. Dentists furthermore have concerns about excessive bleeding from highly vascular supporting dental structures and a residual anticoagulation effect of warfarin after invasive procedures or surgeries. For these reasons, bridge anticoagulation therapy is commonly applied in patients with MHV after temporary cessation of warfarin in clinical practice. In the present study, we compared the safety and cost-effectiveness between bridge therapy with enoxaparin or UFH in MHV patients at moderate to high bleeding risk who required dental procedures.
While both UFH and LMWH have been used for bridge therapy, UFH is costly and time-consuming, as it requires extended periprocedural hospitalization and laboratory monitoring. The risk of heparin-induced thrombocytopenia is also higher in patients treated with UFH than in patients treated with LMWH.14 Therefore, LMWH may be an attractive option for bridge therapy, compared to UFH. Several previous studies reported an increased risk of hemorrhagic complications associated with general surgical procedures in patients treated with LMWH.15,16 However, the clinical significance of hemorrhagic complications related to bridge therapy with LMWH remains unclear in the field of dentistry.
Bui, et al.17 recently reported that enoxaparin is safe for outpatient bridge therapy in patients with MHV. However, they did not provide clinical data related to the safety of enoxaparin in dentistry because dental procedures were not included in their study, and the study included no comparison group that received UFH; therefore, they could not compare the efficacy and safety of LMWH and UFH as bridge therapies. The present study demonstrated that bridge therapy with enoxaparin was not significantly associated with adverse clinical outcomes, compared to bridge therapy with UFH, in patients with MHV who underwent dental procedures with a moderate to high bleeding risk. Old age was significantly associated with total bleeding within 30 days after dental procedures, independent of the type of bridge therapy. These results suggested that enoxaparin could replace conventional bridging with UFH without increasing complications in patients with MHV who require invasive dental procedures. Close observation of bleeding complications may be needed in elderly patients during bridge therapy.
Several previous studies have evaluated the medical costs of LMWH therapy during invasive procedures or surgeries in patients receiving OAC therapy who had a high risk of thromboembolism; the results were inconsistent. Pettinger and Owens18 reported that the use of LMWH may result in avoidable costs during dental extractions. However, in this study, LMWH therapy was not performed on an outpatient basis, and the duration of LMWH therapy was somewhat long, extending from 30 days before the procedures to 5 days thereafter. Meanwhile, Spyropoulos, et al.19 reported that the mean total health care costs during the perioperative period were significantly lower in patients bridging with LMWH than in patients bridging with UFH for an elective general surgical procedures. This cost saving was associated with avoiding or minimizing hospitalization and no increase in clinical adverse events when bridging with LMWH than when bridging with UFH. However, this report was different from our study in that they included patients who underwent a variety of surgical procedures and the comparison between LMWH and UFH was not contemporary.
The present study found that enoxaparin-based bridge therapy in patients with MHV was significantly associated with reducing total medical costs without increasing adverse clinical events, compared to UFH-based bridge therapy during the invasive dental procedure period. Major bleeding was significantly associated with an increase in medical cost, independent of the bridging method. Thus, for patients with MHV who require invasive dental procedures, using enoxaparin as a bridge therapy on an outpatient basis may be a cost-effective and safe method, compared to using UFC.
This study has several limitations. First, there is no official protocol for bridge therapy; we therefore complied with the American College of Chest Physicians guidelines.13 Second, several previous studies on bridge therapy had a follow-up period lasting up to 3 months after the procedures.20,21,22 However, it could be difficult to determine the cause of thromboembolic or bleeding events if the follow-up period was too long in patients who need mandatory life-long anticoagulation therapy. We therefore evaluated the adverse clinical outcomes associated with bridge therapy during a 30-day tracking period after invasive dental procedures. The rate of adverse clinical events may be somewhat different in comparison to previous studies. Third, we evaluated the cost-effectiveness of different bridge therapies including only total medical costs occurred during the periprocedural period. However, most previous studies comparing the cost-effectiveness of bridge therapy between UFH and enoxaparin used total medical costs during the periprocedural period. Additionally, in contrast with UFH-based bridge therapy, enoxaparin-based bridge therapy was performed on an outpatient basis in this study. Lastly, we only compared safety and cost-effectiveness between UFH and enoxaparin in regards to bridge therapy. We did not evaluate these clinical outcomes with regard to the maintenance of warfarin without bridging therapy during invasive dental procedures. Further prospective studies with larger sample sizes are required to address these issues.
In conclusion, considering the benefit of enoxaparin in regards to cost-effectiveness, enoxaparin may be more efficient than UFH for bridge therapy in patients with MHV who require invasive dental procedures. Close observation may be necessary in elderly patients as old age was shown to be an independent predictor of bleeding complications after invasive dental procedures.
Figures and Tables
Table 1
Baseline Characteristics

ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin receptor blockers; LVEF, left ventricular ejection fraction; MHV, mechanical heart valve; NSAIDs, non-steroidal anti-inflammatory drugs; UFH, unfractionated heparin.
Data are expressed as mean±standard deviation or as the number and percent, i.e., n (%).
ACKNOWLEDGEMENTS
This research was supported by the Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea, funded by the Ministry of Education, Science and Technology (2012027176).
References
1. Cannegieter SC, Rosendaal FR, Briët E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation. 1994; 89:635–641.

2. Ansell J, Hirsh J, Poller L, Bussey H, Jacobson A, Hylek E. The pharmacology and management of the vitamin K antagonists: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126:3 Suppl. 204S–233S.
3. Palareti G, Hirsh J, Legnani C, Manotti C, D'Angelo A, Pengo V, et al. Oral anticoagulation treatment in the elderly: a nested, prospective, case-control study. Arch Intern Med. 2000; 160:470–478.
4. Wahl MJ, Howell J. Altering anticoagulation therapy: a survey of physicians. J Am Dent Assoc. 1996; 127:625–626. 629–630. 633–634 passim.

5. Lim W, Wang M, Crowther M, Douketis J. The management of anticoagulated patients requiring dental extraction: a cross-sectional survey of oral and maxillofacial surgeons and hematologists. J Thromb Haemost. 2007; 5:2157–2159.

6. Ward BB, Smith MH. Dentoalveolar procedures for the anticoagulated patient: literature recommendations versus current practice. J Oral Maxillofac Surg. 2007; 65:1454–1460.

7. Katholi RE, Nolan SP, McGuire LB. The management of anticoagulation during noncardiac operations in patients with prosthetic heart valves. A prospective study. Am Heart J. 1978; 96:163–165.

8. Bonow RO, Carabello BA, Chatterjee K, de Leon AC Jr, Faxon DP, Freed MD, et al. 2008 focused update incorporated into the ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1998 guidelines for the management of patients with valvular heart disease). Endorsed by the Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2008; 52:e1–e142.
9. Vahanian A, Baumgartner H, Bax J, Butchart E, Dion R, Filippatos G, et al. Guidelines on the management of valvular heart disease: The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Eur Heart J. 2007; 28:230–268.

10. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010; 138:1093–1100.

11. Schulman S, Kearon C. Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005; 3:692–694.

12. Nematullah A, Alabousi A, Blanas N, Douketis JD, Sutherland SE. Dental surgery for patients on anticoagulant therapy with warfarin: a systematic review and meta-analysis. J Can Dent Assoc. 2009; 75:41.
13. Douketis JD, Berger PB, Dunn AS, Jaffer AK, Spyropoulos AC, Becker RC, et al. The perioperative management of antithrombotic therapy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008; 133:6 Suppl. 299S–339S.
14. Warkentin TE, Levine MN, Hirsh J, Horsewood P, Roberts RS, Gent M, et al. Heparin-induced thrombocytopenia in patients treated with low-molecular-weight heparin or unfractionated heparin. N Engl J Med. 1995; 332:1330–1335.

15. Bickler P, Brandes J, Lee M, Bozic K, Chesbro B, Claassen J. Bleeding complications from femoral and sciatic nerve catheters in patients receiving low molecular weight heparin. Anesth Analg. 2006; 103:1036–1037.

16. Hardy RG, Williams L, Dixon JM. Use of enoxaparin results in more haemorrhagic complications after breast surgery than unfractionated heparin. Br J Surg. 2008; 95:834–836.

17. Bui HT, Krisnaswami A, Le CU, Chan J, Shenoy BN. Comparison of safety of subcutaneous enoxaparin as outpatient anticoagulation bridging therapy in patients with a mechanical heart valve versus patients with nonvalvular atrial fibrillation. Am J Cardiol. 2009; 104:1429–1433.

18. Pettinger TK, Owens CT. Use of low-molecular-weight heparin during dental extractions in a medicaid population. J Manag Care Pharm. 2007; 13:53–58.

19. Spyropoulos AC, Frost FJ, Hurley JS, Roberts M. Costs and clinical outcomes associated with low-molecular-weight heparin vs unfractionated heparin for perioperative bridging in patients receiving long-term oral anticoagulant therapy. Chest. 2004; 125:1642–1650.

20. Ferreira I, Dos L, Tornos P, Nicolau I, Permanyer-Miralda G, Soler-Soler J. Experience with enoxaparin in patients with mechanical heart valves who must withhold acenocumarol. Heart. 2003; 89:527–530.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download