Abstract
Purpose
Recent studies show positive association of early repolarization (ER) with the risk of life-threatening arrhythmias in patients with coronary artery disease (CAD). This study was to investigate the relationships of ER with myocardial scarring and prognosis in patients with CAD.
Materials and Methods
Of 570 consecutive CAD patients, patients with and without ER were assigned to ER group (n=139) and no ER group (n=431), respectively. Myocardial scar was evaluated using cardiac single-photon emission computed tomography.
Results
ER group had previous history of myocardial infarction (33% vs. 15%, p<0.001) and lower left ventricular ejection fraction (57±13% vs. 62±13%, p<0.001) more frequently than no-ER group. While 74 (53%) patients in ER group had myocardial scar, only 121 (28%) patients had in no-ER group (p<0.001). During follow up, 9 (7%) and 4 (0.9%) patients had cardiac events in ER and no-ER group, respectively (p=0.001). All patients with cardiac events had ER in inferior leads and horizontal/descending ST-segment. Patients with both ER in inferior leads and horizontal/descending ST variant and scar had an increased adjusted hazard ratio of cardiac events (hazard ratio 16.0; 95% confidence interval: 4.1 to 55.8; p<0.001).
Early repolarization (ER), which is characterized by an elevation of the junction between the end of the QRS complex and the beginning of the ST segment (J-point) from baseline on a standard 12-lead electrocardiography (ECG), has commonly been regarded as a benign finding.1,2 However, recent data demonstrated an association between ER in the inferior leads and fatal arrhythmias or sudden cardiac death in patients without structural heart diseases.3,4,5,6,7
Furthermore, many studies reported numerous similarities between the ECG and clinical features of acute myocardial ischemia and those of Brugada and ER syndrome.8,9,10 ST-segment abnormalities of acute myocardial ischemia involving the right ventricular outflow tract is similar to those of Brugada syndrome.11 The fundamental mechanisms responsible for ST segment elevation and ventricular fibrillation considered to be similar in the early phases of acute myocardial ischemia and in inherited J-wave syndrome.12 It was also reported that ER in the inferior leads was associated with increased risk of fatal ventricular arrhythmias in patients with coronary artery disease (CAD).13 Recently, we reported that vasospastic angina patients with ER ≥0.1 mV and horizontal/descending ST variant had an increased age- and gender-adjusted hazard ratio (HR) for cardiac events.14
To the best of our knowledge, the cause of ER in CAD patients has not been completely delineated. Moreover, the associations between the ER and myocardial scar and prognosis were not evaluated. In this study, we analyzed the relationship between ER and myocardial scarring or ischemia in CAD patients. We also evaluated the prognostic value of ER pattern and myocardial scarring in CAD patients.
Between May 2005 and May 2011, we identified 2034 consecutive patients with CAD who underwent coronary angiography using ICD-9 codes. Patients without fixed coronary lesion (n=964) and without cardiac single-photon emission computed tomography (SPECT) (n=946) were excluded. Patients older than 70 years, suspected Brugada syndrome, characterized by ST elevation in the right precordial leads (V1 to V3) and long and short QT syndrome were excluded.15,16 Finally, we enrolled 570 patients in this study. ECGs of all patients were reviewed. The patients were divided into two groups according to ER; ER group (n=139) and no ER group (n=431). Clinical characteristics were obtained through chart review. All patients provided informed consents for their participation in this study, which was approved by the Institutional Review Board of Severance Cardiovascular Hospital, Seoul, Korea and complied with the Declaration of Helsinki.
In all study subjects, we evaluated serial ECGs one month after coronary angiography. ECGs recorded during chest pain were excluded from the analysis. Twelve-lead ECGs were manually downloaded from the GE Marquette MUSE system (GE Medial System, Milwaukee, WI, USA). The presence or absence of left ventricular hypertrophy was assessed according to the Sokolow-Lyon criteria, and the QTc interval (corrected for heart rate according to Bazett's formula) was automatically measured. The ECGs were independently reevaluated in random order by two trained cardiologists who were unaware of clinical characteristics, patient grouping and outcome status.
The interobserver variations showed substantial agreement (kappa value, 0.79).17 J-point was defined as a junction between the end of the QRS complex and the beginning of the ST segment. The amplitude of J-point elevation from baseline was also measured. ER patterns were stratified according to J-point elevation that was either notched (a positive J deflection inscribed on the S-wave) or slurred (a smooth transition from QRS to ST-segment) in at least two consecutive inferior or lateral leads.4,18
ST-segment patterns after the J-point were coded as follows: 1) horizontal/descending and 2) concave/rapidly ascending. The horizontal/descending type was defined as ≤0.1 mV elevation of the ST segment within 100 ms after the J-point (arrow of Fig. 1A-1).7 The concave/rapidly ascending ST segment was defined as >0.1 mV elevation of ST segment within 100 ms after the J-point or a persistently elevated ST segment of >0.1 mV throughout the ST segment (arrow of Fig. 1B-1). The isoelectric line (baseline) was defined as the level between 2 T-P intervals. The J-point or ST-segment patterns had to be present in at least two inferior or lateral leads for positive grading. A prolonged QTc interval was defined as at least 440 ms for men and at least 460 ms for women.15,16
Stress/rest 99mTC-methoxyisobutylosonitrile (MIBI) myocardial perfusion SPECT was performed using a 1-day protocol. All patients underwent Tc-99m-MIBI gated SPECT one year after index procedure. Imaging was begun 30 minutes after the administration of 14.7 MBq/kg Tc-99m-MIBI. Image acquisition was obtained in supine position with a dual-head rotating gamma camera (GE, Fairfield, CT, USA) equipped with a low-energy, high-resolution collimator. A total of 34 projections were acquired over a 180° rotation with an acquisition time of 25 seconds each. At each projection angle, eight individual ECG-gated frames per R-R interval were acquired. Transverse sections were reconstructed in a 64×64-pixel matrix by using a filtered back projection with a Butterworth filter. No attenuation correction was used. Immediately after this first imaging, continuous intravenous infusion of low dose dobutamine (LDD); at a dose of 7.5 ug/kg of body mass/min was started and the second acquisition began 5 minutes later. The same imaging acquisition protocol was used for the rest and LDD SPECT.
Stress/rest SPECT imaging was interpreted by 2 expert nuclear cardiologists. A semi-quantitative visual interpretation was made using short axis-, horizontal-, and vertical long axis-myocardial tomograms and a 5-grade (0--4) scoring system in a 20-segment model. The summed stress score (SSS) and summed rest score (SRS) were obtained by adding the scores of the 20 segments on stress and rest imaging, respectively. A study was judged normal if the summed difference score between SSS and SRS was 0. Segment was classified as reversible defect if difference score ≥4, and fixed defect if difference score <4 and rest score >1.
Cardiac events including cardiac death, aborted sudden cardiac death or fatal arrhythmia were analyzed. To distinguish cases of sudden death from arrhythmia, we reviewed all deaths from cardiac causes. After reviewing data available from death certificates, hospital records and ECGs during events, we classified the deaths as follows; cardiac death from heart failure aggravation and aborted sudden cardiac death from fatal arrhythmia. The patient's activity and time of day when the event occurred were evaluated.
Continuous variables were reported as mean±SD, and categorical variables were presented as number and percentage in each group. Comparisons of continuous variables and categorical variables were performed using the two-sided t-test and chi-square test, respectively. The HRs and 95% confidence intervals (CIs) for death were calculated with the Cox proportional-hazards model, in which each subgroups with ER were compared with a reference groups that did not have ER. The multivariate model included age, gender, body mass index, heart rate, QRS duration, QTc duration, ECG signs of left ventricular hypertrophy, and ECG signs of CAD. Kaplan-Meier survival curves were plotted for different ER types and were compared by means of the log-rank test. The SPSS statistical package (SPSS Inc., Chicago, IL, USA) was used to perform all statistical evaluations. A p-value less than 0.05 was considered statistically significant.
ER, which is characterized by an elevation of the J-point in leads other than V1 through V3 on 12-lead ECG, was persistently observed at least 30 days after chest pain in 139 (24.4%) patients with CAD. The clinical characteristics of the patients are described in Table 1. Subjects with ER were more often men (79.1% vs. 66.8%, p=0.006), had lower left ventricular ejection fraction (LVEF) (56.5±12.9% vs. 62.0±12.6%, p<0.001) and previous myocardial infarction (MI) (33.1% vs. 14.6%, p<0.001) more frequently than those with no-ER.
Among 139 CAD subjects with ER, 120 (86.3%) and 31 (22.3%) patients had ER in inferior and lateral leads, respectively. Fourteen (10.1%) of the patients had ER in both inferior and lateral leads. The J-point was notched in 72 (51.8%), slurred in 46 (33.1%), and undetermined in 21 subjects (15.1%). The pattern of ST segment was horizontal/descending in 126 subjects (90.6%) and concave/rapidly ascending in 13 subjects (9.4%).
Fig. 1A shows an example of ER in a patient with CAD and low LVEF of 35%. ST elevation (arrows of Fig. 1A-1) was observed in inferior leads after percutaneous coronary intervention. The notched type J-point elevation in inferior leads persisted for 2 years following intervention (Fig. 1A-2). Fig. 1B shows another example of ER in a patient with CAD and normal LVEF of 60%. ST elevation (arrows of Fig. 1B-1) was observed in lateral leads after coronary artery bypass graft. One month later, the notched and slurred type J-point elevation in V4, V5 and V6 leads were resolved (Fig. 1B-2).
The analysis of serial change in ECG was available for 563 (98.8%) CAD patients among whom were 428 (76%) with no ER and 135 (24%) with ER. ER was persistently observed in 126 (93%) of 135 patients during follow up. ER was persistently observed in 116 (93%) and 32 (25%) patients at inferior and lateral leads, respectively. Twenty-two (17%) patients had ER in both inferior and lateral leads. However, ER was observed in 7 (5.2%) patients transiently during chest pain, and disappeared less than one month after chest pain. ER was observed at lateral leads in all 7 patients. Five (71%) patients had ER in both lateral and inferior leads.
Fig. 2 shows a typical example of ER in a patient with CAD and myocardial scarring. The prominent J-point elevation was observed in inferior leads one year after acute MI (Fig. 2A). Cardiac SPECT at one year after MI showed an irreversible perfusion defect in the anterior portion of mid to apex of the heart (Fig. 2B). Coronary angiography showed near total occlusion of the left anterior descending artery (Fig. 2C). Fig. 3 shows an example of no ER in a patient with CAD but without myocardial scar. ER pattern was not observed (Fig. 3A). There was no defect in cardiac SPECT (Fig. 3B). The critical stenosis of the left anterior descending artery was revascularized with angioplasty and stent implantation (Fig. 3C).
While 74 (53.2%) patients in the ER group had myocardial scarring (fixed defect), only 121 (28.1%) patients had scarring in the no-ER group (p<0.001). In both groups, inferior and anterior walls were the commonest sites of fixed defects. Reversible defect was also more frequently observed in the ER group than in the no-ER group (22.3% vs. 13.5%, p=0.02). Two groups did not differ in numbers of sites with fixed defects (Table 1).
Twelve (2%) patients were lost to follow-up. Table 2 shows the comparison of cardiac events including cardiac death, aborted sudden cardiac death or fatal arrhythmia between ER and no-ER patients. During the follow-up period of 59±36 months, while 9 (6.5%) patients had cardiac events in the ER group, 4 (0.9%) patients had in the no-ER group (p=0.001). Among 13 patients with cardiac arrhythmic events, 9 (69%) patients had ER in the inferior leads with horizontal/descending ST-segment variant. No patients and 2 (1.4% of ER) patients died from cardiac causes in patients with no-ER and ER, respectively (p=0.06). Patients with ER [5% (n=7)] had more frequently aborted sudden cardiac death or fatal arrhythmia than no-ER group [0.9% (n=4), p=0.006]. During the follow-up period, 3 (0.7%) and 4 (2.9%) patients had cardiac events in no-ER and ER groups, respectively. Ventricular fibrillation or arrhythmia was also more frequently observed in ER [3.6% (n=5)] than in no-ER group [0.5% (n=2), p=0.01]. The ER group also had higher incidence of hospitalization for heart failure than the no-ER group (3.6% vs. 0.5%, p=0.01).
Table 3 presents unadjusted, age- and gender-adjusted, and multivariate-adjusted HR for cardiac arrhythmic events associated with different ER and ST-segment patterns. Subjects with ER and horizontal/descending ST segments had a higher risk of cardiac events (age- and gender-adjusted HR: 5.73; 95% CI: 1.7 to 19.5; p=0.005). In contrast, no patients with ER and concave/rapidly ascending ST segments had cardiac events (Table 3).
A separate analysis of subjects with inferior ER demonstrated a higher risk of cardiac events (age- and gender-adjusted HR: 6.39; 95% CI: 1.9 to 21.6; p=0.003). Among subjects with inferior ER and horizontal/descending ST segments (n=110), the HR was 6.9 (95% CI: 2.1 to 23.6; p=0.002) for arrhythmic death after adjustments for age and gender (Table 3).
Patients with both ER in the inferior leads and horizontal/descending ST variant and myocardial scar had an increased age and gender adjusted HR of cardiac events (HR: 10; 95% CI: 2.7 to 37.7; p=0.001), and age, gender, body mass index, heart rate, QTc duration, QRS duration, ECG signs of left ventricular hypertrophy and ECG signs of CAD adjusted HR of cardiac events (HR: 16.0; 95% CI: 4.1 to 52.3; p<0.001). Interestingly, in patients without myocardial scar, ER in inferior leads and horizontal/descending ST variant did not increase the risk of cardiac event.
Fig. 4 shows the Kaplan-Meier survival curves for cardiac events in patients with different inferior ER and ST-segment patterns. The patients with ER in inferior leads and scar had lower cumulative survival free of cardiac events than patients without ER (p<0.001).
The main finding of this study was that ER was observed in one-fourth of patients with CAD. The second finding was that one-half of CAD patients with ER also had myocardial scar. Thirdly, CAD patients with ER more frequently had cardiac events during follow up including cardiac deaths, aborted sudden cardiac death or fatal arrhythmias than those patients with no-ER. Fourthly, CAD patients who had ER and horizontal/descending ST segments had a higher risk of cardiac events, if they had myocardial scar. In the absence of scarring, however, this same ECG pattern was not associated with excess risk. Our study suggests that ER may be related with myocardial scarring, predicting cardiac events in patients with CAD.
ER has been considered a benign finding observed among healthy and young individuals. However, recent studies reported that inferolateral ER is related with idiopathic VF in patients without structural heart disease.4,5,18,19
In this study, ER was observed in one-fourth of patients with CAD. ER in CAD patients might be caused by irreversible myocardial damage or scarring. A high incidence of ER has been reported in patients with healed myocardial infarction.13 In this study, one-half of CAD patients with ER had myocardial scar. ER pattern persisted in most patients even after resolution of ischemia. Another possible explanation of ER in CAD patients is that the ER in CAD patients might be due to ECG change caused by myocardial ischemia or vasospastic angina.14,20,21 In in vitro models, early phase ischemia and genetic J-wave syndromes showed similar features in ECG appearance and arrhythmogenesis pathophysiology.11 Myocardial ischemia reduces inward currents (principally INa and ICa), increases outward potassium currents by opening KATP channels, and intensifies Ito, particularly in the epicardium. Blocking the INa current, KATP opening and the Ito current generate J-waves both in genetically proven channelopathies and in experimental drug-induced models.3,11 Finally, patients with ER might be more susceptible to myocardial ischemia, fatal arrhythmia and sudden death than those with no-ER. Compared to those with no-ER, early and easy diagnosis of CAD can be possible by this serious feature of CAD patients with ER.
Patients with structural heart disease, however, may have another acquired form of terminal notching of the QRS complex, formerly called peri-infarction block. Peri-infarction block, another form of terminal notching of the QRS complex, has been known to be caused not by early repolarization but by delayed depolarization of heterogenous myocardial scar tissues.22,23 It has also been known to be frequently associated with ventricular late potentials in signal-averaged ECGs and increased risk of malignant ventricular arrhythmias and sudden death, caused by macro-reentry.22,23
In the present study, the prevalence of ER was found to be much higher than that of congestive heart failure (CHF) patients (12.1%) and vasospastic angina (VA) patients (21.4%).14,24 However, it was lower than 32% reported in myocardial infarct patients with ventricular arrhythmia.13 Therefore, it can be explained by myocardial damage, and might expect cardiac events.
It is not fully elucidated why ventricular fibrillation (VF) occurs only in some patients, although they all have similar clinical variables. CAD patients with ER and horizontal/descending ST segment had cardiac events more frequently than did those with no-ER. These results are consistent with previous observations that ER patterns in the inferior leads6,13 and ER patterns with horizontal/descending ST segment7 were associated with mortality risk. However, in these studies, even CAD patients with ER did not have cardiac events, if they did not have myocardial scar. Moreover, reversible ischemia was not associated with increased risk of cardiac events.
The presence of a prominent action potential notch in epicardium but not endocardium produce a transmural voltage gradient during ventricular activation that manifests as a J wave.11,25 Preexisting myocardial scars can produce tissue heterogeneity to produce fatal arrhythmia. Thus, CAD patients with both ER and scar might have an arrhythmogenic substrate, and are more susceptible to myocardial ischemia or triggers.26
There are several limitations in this study. First, absolute number of events was small in both groups. Therefore, a study with larger number of patients is needed. Second, because most patients experienced fatal arrhythmias at out of hospital, the association between ER during acute ischemia and the occurrence of fatal arrhythmias was not evaluated.
Early repolarization in the inferior leads and horizontal/descending ST-segment variant was more frequently observed in CAD patients with myocardial scar. Furthermore, the CAD patients with ER and myocardial scarring had higher incidence of cardiac events. Our findings suggest that ER pattern may be related to myocardial scar, predicting the prognosis in CAD patients.
Figures and Tables
Fig. 1
Classification of ECG patterns. (A) Horizontal/descending ST-segment patterns. The patient presented horizontal/descending ER in leads II, III, and aVF (arrows) at one month after PCI (A-1) and persisted for 2 years after PCI (A-2). (B) Concave/rapidly ascending ST-segment patterns. The patient presented concave/rapidly ascending ER in lateral leads one month after CABG (B-1). These ER resolved after one month (B-2). ECG, electrocardiography; ER, early repolarization.

Fig. 2
Early repolarization in a 64-year-old male patient with history of ST-elevation, anterior wall myocardial infarction and scar. (A) 12-lead ECG at one year after MI showed prominent J-point elevations (arrows) in leads of II, III and aVF. (B) Cardiac SPECT at one year after MI showed irreversible perfusion defect in the anterior portion of mid to apex of the heart. (C) Coronary angiography showed near-total occlusion of the left anterior descending artery. MI, myocardial infarction; SPECT, single-photon emission computed tomography; ECG, electrocardiography.

Fig. 3
Findings in a 59-year-old patient with CAD but without ER and without myocardial scar formation. (A) ER pattern was not observed. (B) No defect detected by SPECT. (C) Revascularization of the critical stenosis of left anterior descending artery. CAD, coronary artery disease; ER, early repolarization; SPECT, single-photon emission computed tomography.

Fig. 4
The Kaplan-Meier survival curves for cardiac events according to the presence of myocardial scarring and J wave. The patients with J wave and myocardial scar had lowest cumulative event-free survival (log rank p<0.001).
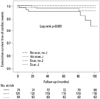
Table 3
Hazard Ratios of Cardiac Events According to ER and ST-Segment Groups

HR, hazard ratio; CI, confidence interval; ER, early repolarization; ECG, electrocardiography.
The p-values were calculated with the Cox proportional-hazard model, in which each ER subgroup was compared with a reference group with no ER.
*Adjusted for age and sex.
†Adjusted for age, sex, body-mass index, heart rate, QTc duration, QRS duration, and ECG signs of left ventricular hypertrophy.
‡Adjusted for age, sex, body-mass index, heart rate, QTc duration, QRS duration, ECG signs of left ventricular hypertrophy and ECG signs of coronary artery disease.
ACKNOWLEDGEMENTS
This study was supported in part by research grants of the Basic Science Research Program through the National Research Foundation of Korea, funded by the Ministry of Education, Science and Technology (NRF-2010-0021993, NRF-2012R1A2A2A02045367), and a grant of the Korean Healthcare technology R&D project, Ministry of Health & Welfare (HI12C1552). We thank Hyuk Jeon for his technical support.
References
1. Goldman MJ. RS-T segment elevation in mid- and left precordial leads as a normal variant. Am Heart J. 1953; 46:817–820.

2. Klatsky AL, Oehm R, Cooper RA, Udaltsova N, Armstrong MA. The early repolarization normal variant electrocardiogram: correlates and consequences. Am J Med. 2003; 115:171–177.

3. Haïssaguerre M, Chatel S, Sacher F, Weerasooriya R, Probst V, Loussouarn G, et al. Ventricular fibrillation with prominent early repolarization associated with a rare variant of KCNJ8/KATP channel. J Cardiovasc Electrophysiol. 2009; 20:93–98.
4. Nam GB, Kim YH, Antzelevitch C. Augmentation of J waves and electrical storms in patients with early repolarization. N Engl J Med. 2008; 358:2078–2079.

5. Rosso R, Kogan E, Belhassen B, Rozovski U, Scheinman MM, Zeltser D, et al. J-point elevation in survivors of primary ventricular fibrillation and matched control subjects: incidence and clinical significance. J Am Coll Cardiol. 2008; 52:1231–1238.

6. Tikkanen JT, Anttonen O, Junttila MJ, Aro AL, Kerola T, Rissanen HA, et al. Long-term outcome associated with early repolarization on electrocardiography. N Engl J Med. 2009; 361:2529–2537.

7. Tikkanen JT, Junttila MJ, Anttonen O, Aro AL, Luttinen S, Kerola T, et al. Early repolarization: electrocardiographic phenotypes associated with favorable long-term outcome. Circulation. 2011; 123:2666–2673.
8. Kataoka H. Electrocardiographic patterns of the Brugada syndrome in right ventricular infarction/ischemia. Am J Cardiol. 2000; 86:1056.

9. Indik JH, Ott P, Butman SM. Syncope with ST-segment abnormalities resembling Brugada syndrome due to reversible myocardial ischemia. Pacing Clin Electrophysiol. 2002; 25:1270–1273.

10. Jastrzebski M, Kukla P. Ischemic J wave: novel risk marker for ventricular fibrillation? Heart Rhythm. 2009; 6:829–835.

11. Yan GX, Antzelevitch C. Cellular basis for the electrocardiographic J wave. Circulation. 1996; 93:372–379.

12. Hlaing T, DiMino T, Kowey PR, Yan GX. ECG repolarization waves: their genesis and clinical implications. Ann Noninvasive Electrocardiol. 2005; 10:211–223.

13. Patel RB, Ng J, Reddy V, Chokshi M, Parikh K, Subacius H, et al. Early repolarization associated with ventricular arrhythmias in patients with chronic coronary artery disease. Circ Arrhythm Electrophysiol. 2010; 3:489–495.

14. Oh CM, Oh J, Shin DH, Hwang HJ, Kim BK, Pak HN, et al. Early repolarization pattern predicts cardiac death and fatal arrhythmia in patients with vasospastic angina. Int J Cardiol. 2013; 167:1181–1187.

15. Antzelevitch C, Brugada P, Borggrefe M, Brugada J, Brugada R, Corrado D, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005; 111:659–670.

16. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992; 20:1391–1396.

17. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174.

18. Haïssaguerre M, Derval N, Sacher F, Jesel L, Deisenhofer I, de Roy L, et al. Sudden cardiac arrest associated with early repolarization. N Engl J Med. 2008; 358:2016–2023.

19. Gussak I, Antzelevitch C. Early repolarization syndrome: clinical characteristics and possible cellular and ionic mechanisms. J Electrocardiol. 2000; 33:299–309.

20. Myerburg RJ, Kessler KM, Mallon SM, Cox MM, deMarchena E, Interian A Jr, et al. Life-threatening ventricular arrhythmias in patients with silent myocardial ischemia due to coronary-artery spasm. N Engl J Med. 1992; 326:1451–1455.

21. Amsterdam EA. Relation of silent myocardial ischemia to ventricular arrhythmias and sudden death. Am J Cardiol. 1988; 62:24I–27I.

22. Castle CH, Keane WM. Electrocardiographic "peri-infarction block". A clinical and pathologic correlation. Circulation. 1965; 31:403–408.
23. Scherlag BJ, Gunn CG, Berbari EJ, Lazzara R. Peri-infarction block (1950)-late potentials (1980): their relationship, significance and diagnostic implications. Am J Cardiol. 1985; 55:839–841.

24. Furukawa Y, Yamada T, Morita T, Iwasaki Y, Kawasaki M, Kikuchi A, et al. Early repolarization pattern associated with sudden cardiac death: long-term follow-up in patients with chronic heart failure. J Cardiovasc Electrophysiol. 2013; 24:632–639.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download