Abstract
Purpose
Blastocyst transfer has been recommended to raise the implantation rate without affecting the pregnancy rate. The objective of this meta-analysis is to systematically evaluate whether the live birth rate and other pregnancy outcomes can be improved by blastocyst transfer compared with cleavage-stage embryos transfer.
Materials and Methods
EMBASE and MEDLINE databases were searched for papers published between March 2004 and March 2013. An extensive range of the electronic databases yielded initially 317 studies from which seven trials met the inclusion criteria for further analysis. Our outcome measures were the live birth rate, clinical pregnancy rate, implantation rate, ongoing pregnancy rate, multiple pregnancy rate, first trimester miscarriage rate and ectopic pregnancy rate. Fixed effects models were chosen to calculate the odds ratio (OR).
Results
Seven trials (n=1446 cases) were finally analyzed. Compared with cleavage-stage embryos transfer, the blastocyst transfer was statistically significantly associated with an increase in clinical pregnancy rate [OR 1.43; 95% confidence interval (CI), 1.15-1.78], implantation rate (OR 1.38; 95% CI, 1.09-1.74) and ongoing pregnancy rate (OR 2.15; 95% CI, 1.57-2.94), and also a reduction in the probability of first trimester miscarriage rate (OR 0.51; 95% CI, 0.30-0.87). The improvement in the live birth rate was also observed (OR 1.77; 95% CI, 1.32-2.37). Moreover, there was no evidence of difference in multiple pregnancy and ectopic pregnancy rates.
The transfer of early cleavage-stage embryos on Day 2 or Day 3 is a common practice in the assisted reproductive technology (ART) programs. However, many embryos can grow successfully to the blastocyst stage, allowing embryo transfer on Day 5 or 6 following oocyte retrieval. Recently, the blastocyst transfer based on an improved culture system has been proven effective for selection of embryos, resulting in a higher implantation rate without affecting pregnancy rate.1 The high implantation rates could allow fewer-transferring but higher-quality embryos at the blastocyst stage, thus avoiding the risk of multiple pregnancy.2
Extending the duration of embryo culture to the blastocyst stage for ART offers several theoretical advantages over the transfer of cleavage-stage embryos. These include 1) minimizing exposure of embryo to hyper-stimulated uterine environment, 2) supplying better physiological synchronization between embryo stage and the endometrium at the time of embryo transfer,3 3) optimizing selection of embryos with increased implantation potential, 4) increasing the possibility to undergo cryopreservation, and 5) reducing uterine contractions, etc. However, blastocysts have certain drawbacks. With current techniques, some cleavage embryos do not develop into blastocysts in vitro and some blastocysts can not be well cryopreserved. Therefore, it is still questionable whether the transfer of blastocyst-stage embryos is beneficial to all infertile patients.4, 5, 6, 7, 8
Several comparisons have been made recently between the benefits of cleavage-stage embryo or blastocyst culture and transfers. Most of the studies have proved that the prolonged culture in sequential media has led to a dramatic increase in the practice of blastocyst freezing, and much higher pregnancy rates. A number of studies summarized in a Cochrane review demonstrated a higher pregnancy rate and live birth rate after blastocyst transfer than that after cleavage-stage transfer.9 When an equal number of embryos, cultured in sequential media, were transferred, the summarized odds ratio (OR) for a live birth was 1.35 [95% confidence intervals (CIs): 1.05-1.74]. Another meta-analysis found a similar OR of 1.39 (95% CI, 1.10-1.76).10
A Cochrane review in 2012 reported that the live birth rate was higher in blastocyst transfer than that in cleavage-stage embryo transfer, although no evidence of difference was found between the two groups in regard with the rates of clinical pregnancy and miscarriage.11 However, the other adverse pregnancy outcomes, such as first trimester miscarriage and ectopic pregnancy rates, were not mentioned in their reviews, therefore, it is difficult to comprehensively understand the pregnancy outcomes after blastocyst transfer through this report.
As the embryo culture system is becoming stable since the year 2004, we aimed to perform a systematic review of randomized controlled trials (RCTs) to compare the effectiveness of equal number of cleavage-stage embryos transfer with that of blastocyst transfer on the outcomes of live birth, clinical pregnancy, ongoing pregnancy, implantation and multiple pregnancy rates. In addition, we used the combined dataset of randomized women to investigate the key outcomes, such as first trimester miscarriage and ectopic pregnancy rates which were not reported by the relevant previous trials.
As the embryo culture system was becoming stable after the year 2004, search strategies included online surveys of databases (MEDLINE, EMBASE) from March 2004 to March 2013. The following headings and text strings were used singly or in combination: embryo transfer, Day two or Day 2, Day three or Day 3, cleavage, Day five or Day 5, Day six or Day 6, blastocyst, randomized controlled trial, and clinical trial. There was no language restriction. Journals and abstracts from major infertility meetings were also hand-searched in an effort to identify any unpublished trials.
Criteria for inclusion/exclusion of the studies were established before the literature search.
1) The participants comprised subfertile women who underwent embryo transfer following in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI), or both, with their own gametes or as an oocyte/embryo donation recipient.
2) Only RCTs that compared the clinical effectiveness of cleavage-stage embryos with blastocyst transfer were deemed eligible for inclusion in the meta-analysis.
3) The study was considered eligible only if the researchers applied a policy to transfer an equal number of embryos in the compared two groups. Embryos were randomized by 1:1 ratio to undergo cleavage-stage embryo or blastocyst transfer.
4) Outcome measures included live birth, clinical pregnancy, ongoing pregnancy, implantation, multiple pregnancy, first trimester miscarriage and ectopic pregnancy rates.
5) RCTs in which women's age >45 years were excluded.
6) Cleavage-stage transfers versus blastocyst transfers in frozen cycles, in which no data were available from the fresh cycle, were not considered in this review.
A search of the electronic databases yielded 317 relevant studies that were assessed for inclusion in this review. In the case of duplicate studies, we included only the most comprehensive one. 265 studies were found to be potentially eligible and were subsequently scrutinized. The examination of the titles reduced the potentially eligible studies to 180. After screening the details, 171 studies were excluded because they did not compare cleavage-stage embryos transfer with blastocyst transfer (n=46), or not RCTs (n=125). By this process, studies were further excluded because they did not follow a policy of transferring equal number of embryos in the two groups compared (n=2). Ultimately, we identified seven trials to our review and meta-analysis (Fig. 1).12, 13, 14, 15, 16, 17, 18
Data extraction and assessment of trial quality were performed independently by two reviewers (Shan-Shan Wang and Hai-Xiang Sun). Any disagreement was resolved by discussion. A data collection form was used to collect raw data. Descriptive tables for study characteristics and outcome data for seven eligible studies were generated. For each trial, the first author, publication year, journal title, sample size, type of fertilization, inclusion criteria at randomization, ovarian stimulation protocol, type of gonadotropin administered, day of transfer, blastulation rate, culture media used and relevant outcomes (live birth, clinical pregnancy achievement, ongoing pregnancies, multiple pregnancy, first trimester miscarriage and ectopic pregnancy) were collected.
Our primary outcome measures chosen for meta-analysis were the live birth rate per couple, clinical pregnancy rate per couple randomized, implantation rate per embryo transfer and ongoing pregnancy rate per couple. The secondary outcome measures included multiple pregnancy rate per clinical pregnancy, first trimester miscarriage rate and ectopic pregnancy rate.
All outcomes were defined before the literature search was undertaken. The implantation rate was defined as the result from the number of gestational sacs with fetal heart beat seen on ultrasound scan divided by the total number of embryos transferred. Pregnancy was defined as a positive urinary or serum β-hCG result. Clinical pregnancies were considered as visualization by ultrasound of a gestational sac with fetal pole and fetal heart movements at ≥6 weeks' gestation. Ongoing pregnancies were those pregnancies beyond 10-12 weeks of gestation, at which stage the patients were referred out for antenatal care.
Statistical analysis was performed in accordance with the guidelines developed by the Menstrual Disorders and Subfertility Group (MDSG). The outcomes were pooled statistically. Meta-analysis was calculated with Rev Man software [version 5.0.16 (2008); The Nordic Cochrane Centre, Copenhagen, Denmark]. Dichotomous data for observational studies were expressed as an OR with 95% CI and combined using Mantel-Haenszel method and a fixed-effects model. Chi-square and I2 tests were employed to assess the heterogeneity among the studies and to assess the heterogeneity beyond chance. An I2 value greater than 50% may be considered to represent a substantial heterogeneity. p<0.05 was considered statistically significant.
Seven trials fulfilled the inclusion criteria. A total of 1446 participants were reviewed (blastocyst transfer: n=712; cleavage-stage transfer: n=734). The sample size varied between studies, with a mean of 206 couples, including both cleavage-stage and blastocyst groups per trial. For the cleavage-stage groups, most of the transfers took place on Day 3, with the exception of two trials on Day 2.12,17
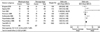
The characteristics of the seven studies included in the systematic review are presented in Table 1 and 2. Randomization was performed on the morning of embryo transfer by computer-generated randomized list, random permuted blocks or sealed envelopes. Regarding the policy of the applied embryo transfer in the seven studies, two studies applied the policy with a maximum of two embryos transferred in both groups, one study with a fixed number of two embryos (double-embryo transfer), three studies with a fixed number of one single embryo transfer (SET), and one study with a ratio of 1:1 in both groups. Fertilization methods included ICSI (n=1), IVF (n=1) and IVF/ICSI (n=5). Six trials used sequential media, of which four used Vitrolife G1/G2. Only one trial did not state the media used.16
Among the included trials, apart from one report that included women who had 6 follicles a day prior to hCG irrespective of the woman's age, all other trials included women with an upper age limit ranging between 35 and 42 years. The included women were of good prognosis, i.e. such women without a history of triple failed IVF cycles, and with one to four good-quality embryos. Criteria for embryo quality differed in the individual trials but generally involved visual morphological assessment, in addition to the number of blastomeres.
Ovarian stimulation protocols were clearly described in five trials (Table 2), but not in two.16,17 A combination of urinary and recombinant follicle-stimulating hormone was used in four studies, while in one study this was achieved with recombinant gonadotropins. To inhibit the premature luteinizing hormone (LH) surge, a long agonist protocol was used in one trial. The ovarian stimulation was used in other three trials by means of both the long gonadotropin-releasing hormone agonist and the antagonist protocol in the same study, while a fixed antagonist protocol on Day 6 was applied in one trial.
The live birth rate is the percentage of all cycles that lead to live birth, and is the pregnancy rate adjusted for miscarriages and stillbirths. Fig. 2 demonstrates that the live birth rate in cleavage-stage embryo transfer group (28%, 117/412) was lower than that in blastocyst transfer group (41%, 168/410) (4 RCTs, OR: 1.77, 95% CI: 1.32-2.37; p=0.0001; heterogeneity: p=0.35; fixed effects model). No heterogeneity was detected (I2=8%).
Large studies showed a high clinical pregnancy rate after blastocyst replacement. In this meta-analysis, the probability of clinical pregnancy was significantly higher in the patients with blastocyst transfer than those with cleavage-stage embryo transfer (7 RCTs, OR: 1.43, 95% CI: 1.15-1.78; p=0.001; heterogeneity: p=0.07; fixed effects model). No heterogeneity was detected (I2=48%) (Fig. 3).
The implantation rate, a limiting factor for success, represents the capacity of each embryo transferred during this period to implant in the uterus and to result in pregnancy. Fig. 4 showes that the implantation rate of the blastocysts (36%, 235/648) was significantly higher than the cleavage-stage embryos transfer (29%, 203/700) (4 RCTs, OR: 1.38, 95% CI: 1.09-1.74; p=0.007; heterogeneity: p=0.04; fixed effects model).
The established positive relationship between morphological embryo integrity and implantation potential in IVF/ICSI cycles indicates that the difference in the ongoing pregnancy rate is probably due to an embryonic factor. Evidence of a significant difference between the two treatment groups was found in the ongoing pregnancy rate per couple favoring blastocyst culture (4 RCTs, OR: 2.15, 95% CI 1.57-2.94; p<0.00001; heterogeneity: p=0.39; fixed effects model) (Day 2 to 3: 27% versus Day 5 to 6: 44%). No heterogeneity was detected (I2=1%) (Fig. 5).
There was no evidence of difference in multiple pregnancy per clinical pregnancy between the cleavage-stage embryo transfer group (20%, 42/209) and blastocyst transfer group (18%, 47/256) (5 RCTs, OR: 0.88, 95% CI: 0.54-1.42; p=0.59; heterogeneity: p=0.39; fixed effects model). No heterogeneity was detected (I2=2%) (Fig. 6).
The most common cause of spontaneous miscarriage during the first trimester is chromosomal abnormalities of the embryo or fetus. As shown in Fig. 7, the rate of first trimester miscarriage in the cleavage-stage embryo transfer group (26%, 43/168) was higher than that in blastocyst transfer group (18%, 35/197) (4 RCTs, OR: 0.51, 95% CI: 0.30-0.87; p=0.01; heterogeneity: p=0.43; fixed effects model). No heterogeneity was detected (I2=0%).
Ectopic pregnancy rate was not significantly different between the cleavage-stage embryo transfer group (0.02%, 3/197) and blastocyst transfer group (0.01%, 2/168) (4 RCTs, OR: 1.09, 95% CI: 0.27-4.34; p=0.90; fixed effects model). No heterogeneity was detected (I2=0%) (Fig. 8).
Transferring embryos at the blastocyst stage might be the most biologically correct stage for embryos in the uterus, because embryos in earlier stages are naturally in the fallopian tube, and the longer culture in the laboratory may give the scientist greater ability to select the best quality embryos for transfer.18 This systematic review and meta-analysis demonstrated that blastocyst (Day 5/6) transfer in a fresh IVF/ICSI treatment cycle significantly increased clinical pregnancy, implantation, ongoing pregnancy and live birth rates, simultaneously lowering first trimester miscarriage rate, in comparison with the equal number of cleavage-stage (Day 2/3) embryos transfer in the 7 RCTs. However, no evidence of difference in the rates of multiple pregnancy and ectopic pregnancy, was found between blastocyst and cleavage-stage embryo transfers.
Blastocyst culture has been associated with higher clinical pregnancy and live birth rates.19, 20, 21 Frattarelli, et al.22 performed a randomized controlled trial comparing Day 3 with Day 5 embryo transfer. The pregnancy rate was 69.2% for Day 5 transfers and 43.5% for Day 3, whereas the live birth rate was 57.7% for Day 5 transfers and 38.4% for Day 3. Thus, the current meta-analysis provides clinical confirmation of the above finding: the rate increased 9% clinical pregnancies and 13% live births if clinics used blastocyst transfer was compared with cleavage-stage embryo transfer. This could be explained by the synchrony between the endometrial and embryo development, thus overcoming the alterations in endometrium receptivity already induced by ovarian stimulation for IVF.23
The comparable implantation rates per developed embryo between the two groups showed that the implantation ability was obviously improved after blastocyst transfer (36% for blastocyst versus 29% for cleavage-stage), and it might be attributed to a good physiological adjustment between the stage of transferred embryo and the maturity of the endometrium. The in vivo stimulated endometrial environment can not be compared with endometrium in a natural cycle.24 In addition, progesterone (P) has been highlighted as the crucial molecule participating in the induction of this asynchrony in stimulated cycles.25 Papanikolaou, et al.26 reported that the modest rises of progesterone in the follicular phase (P above 1.5 ng/mL on the day of hCG administration) have a detrimental effect on the implantation potential of a good quality cleavage-stage embryo. In contrast, premature luteinization in the blastocyst group had no effect on the pregnancy outcome.
Miscarriage rate is a critical factor when evaluating a new mode of treatment and it has an obvious impact on treatment efficiency and live birth outcomes. The first trimester of pregnancy includes the first 13 weeks after the last menstrual period. Most of the spontaneous miscarriages after in vitro fertilization and embryo transfer (IVF-ET) occur during this period, which has a direct relationship with the potential of embryonic development. In line with our observations, selecting a blastocyst is more reassuring in terms of pregnancy achievement, because the selection is made through a cohort of cleavage-stage embryos which have already survived the process of initial selection. Therefore, they are more likely to implant and are less prone to be aborted. In our study, the first trimester miscarriage rate in the blastocyst transfer group decreased from 26% to 18% compared with the cleavage-stage embryo transfer group. The decreased pregnancy miscarriage with blastocyst transfer points to the important role of uterine receptivity for a successful pregnancy outcome. During the multi-follicular ovarian stimulation in IVF, the altered endometrial development was observed as early as the late follicular phase, and extended throughout the luteal phase. A cleavage-stage embryo might not be able to conquer the defects in endometrial receptivity.27
Multiple pregnancy, especially triplets or more, is one of the most serious issues in assisted reproductive technology (ART).28 There is no doubt that blastocyst transfer is a way to eliminate the burden of multiple pregnancy on children, due to the decreased number of embryos transferred. However, multiple pregnancy rates were not significantly different between groups receiving cleavage-stage embryos and blastocysts (20% for cleavage-stage versus 18% for blastocyst) in the current meta-analysis. In the studies that have reported the incidence of multiple pregnancy (three or more implanted embryos), the incidence in the groups receiving cleavage-stage embryos or blastocysts was not different.29
The blastocyst culture may increase the likelihood of selectively transferring viable and genetically normal embryos. Although the development to the blastocyst stage is not a guarantee of chromosomal normality, most embryos that fail to continue to develop in extended culture show multiple aneuploidies.30 Some investigators have shown that embryos up to 60% in the top quality cleavage-stage might be aneuploid, whereas this percentage might reach to 30% in the top quality blastocysts.31 The accumulating evidence suggests that embryos on Day 5 carry a lower risk of being aneuploid, thereby increasing a patient's chances of achieving an ongoing pregnancy. In this meta-analysis, ongoing pregnancy rate per couple was significantly raised from 27% (Day 2/3) to 44% (Day 5/6). Prolonging the duration of culture to Day 5 may allow chromosomally competent embryos to develop into the blastocyst stage and permit selecting the embryos that have a potential of continuing development under embryonic genomic control.32
Ectopic pregnancy has been reported to occur in approximately 2-5% of all clinical pregnancies after IVF cycles.33 Studies showing the decreased uterine contractility further along in the luteal phase would imply that the ectopic pregnancy rates should be reduced after a blastocyst transfer compared to a cleavage-stage transfer.34 The blastocyst with a large-diameter was proposed as an additional factor in reducing the rate of tubal pregnancies following Day 5 transfer.35 Even though these findings suggest an association of blastocyst transfer with a lowered ectopic pregnancy risk, our study failed to show such a trend. It is possible that when a blastocyst is transferred, it does indeed have a low probability of entering the fallopian tube to implant there.
The introduction of the sequential culture media has been suggested to improve blastocyst cultures, because they were designed according to the metabolic requirements of embryos at different stages of development.36,37 The sequential media for the culture of blastocysts are used for all of the trials included, except the report from Fisch, et al.16 The rate of blastocyst formation may also influence the pregnancy rate per embryo transfer in each trial. They ranged from 33%11 to 97%.17 Some studies in which sequential media were available found a dramatic increase in the practice of blastocyst freezing, much higher pregnancy and live birth rates.38
There are several potential risks of blastocyst transfer. The lack of accepted criteria for predicting blastocyst development increases the risk of having no embryos to transfer despite observations of adequate development in vitro on Day 2/3, and reduces the embryo freezing rate. The number of embryos frozen is an important factor to evaluate the effectiveness of a treatment, because it offers an additional opportunity for patients to achieve pregnancy. Assessing the embryo quality at different stages could help determine the embryos with the best potential for implantation.39 In the present study, embryo quality on Day 3 did not have any influence on the pregnancy rate of Day 3 transfers. On the contrary, however, if there was no good embryo on Day 3, the embryo quality would have a great impact on the pregnancy rate of Day 5 transfers. Coskun, et al.40 reported that the lack of good quality embryos on Day 3 resulted in no pregnancy for Day 5 transfer (versus 33% pregnancy for Day 3 transfers). In these studies, criteria for embryo quality differed but generally involved one to four good-quality embryos on Day 3, therefore, the clinical pregnancy and live birth rates were extremely high in blastocyst transfer on Day 5/6. In fact, it has been proposed to combine pronucleate embryo scoring with blastocyst culture, in order to determine which embryos grow into blastocysts in vitro.41 Moreover, the chance of blastocyst transfer has been shown to depend on the number of oocytes retrieved rather than age.42
The transfer of good quality blastocysts selected by using objective methods will be a central part of IVF treatment in the years to come. Compared with other previous study, the present review is in agreement with a systematic review published by Glujovsky, et al.11 who reported that the live birth rate was higher in blastocyst transfers than in the cleavage-stage embryos. Due to higher rates of frozen embryos obtained from the cleavage-stage protocols, cumulative pregnancy rates significantly favoured cleavage-stage transfer. Furthermore, their review showed no evidence of difference in the clinical pregnancy rate and miscarriage rate between the two groups, whereas the clinical pregnancy rate and first trimester miscarriage rate were drastically higher in our review's blastocyst transfer group. The current meta-analysis also includes implantation, ongoing pregnancy and ectopic pregnancy rates, comprehensively illustrating that the pregnancy outcomes after fresh IVF/ICSI are strikingly improved following the blastocyst transfer.
The relative weakness of the current meta-analysis is that the natural evolution of embryo transfer policies is internationally towards single embryo transfer; however, only three studies in this meta-analysis had a policy for single blastocyst transfer. Consequently, more large-scale RCTs designed to evaluate the pregnancy outcomes after single blastocyst transfer, would be needed to further strengthen this conclusion. Furghermore, cost comparisons of treatment have not been investigated in this review, nevertheless, are noteworthy. Often, an additional incubator is required due to additional 2-3 days during which the embryos remain in culture. Blastocyst culture is much labour intensive, and laboratory staff may be required to perform more weekend work, particularly if the embryos from two different stages of development are required to be cryopreserved. For patients, a higher chance of cancellation of the treatment cycle prior to embryo transfer may result in a lower treatment cost. Therefore, it is necessary to carry out multi-centre randomised trials with follow-up assessment, in which both clinical effectiveness and cost effectiveness should be included.
In conclusion, on the basis of evidence provided by the randomized studies available, blastocyst transfer seems to be an efficient method to improve the live birth rate. Additionally, less blastocyst transfer might reduce the multiple pregnancy rate whilst maintaining pregnancy success.
Figures and Tables
 | Fig. 2Forest plot of comparison: live birth rate per couple. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
 | Fig. 3Forest plot of comparison: clinical pregnancy rate per couple. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
 | Fig. 4Forest plot of comparison: implantation rate per embryo transfer. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
 | Fig. 5Forest plot of comparison: ongoing pregnancy rate per couple. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
 | Fig. 6Forest plot of comparison: multiple pregnancy rate per clinical pregnancy. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
 | Fig. 7Forest plot of comparison: first trimester miscarriage rate. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
 | Fig. 8Forest plot of comparison: ectopic pregnancy rate. The horizontal bars extending to the right and left of the black circles represent the widths of 95% confidence intervals (CIs). The variation in the CIs is a function of different sizes of the samples. M-H, Mantel-Haenszel. |
References
1. Mangalraj AM, Muthukumar K, Aleyamma T, Kamath MS, George K. Blastocyst stage transfer vs cleavage stage embryo transfer. J Hum Reprod Sci. 2009; 2:23–26.

2. Karaki RZ, Samarraie SS, Younis NA, Lahloub TM, Ibrahim MH. Blastocyst culture and transfer: a step toward improved in vitro fertilization outcome. Fertil Steril. 2002; 77:114–118.

3. Edwards RG, Beard HK. Blastocyst stage transfer: pitfalls and benefits. Hum Reprod. 1999; 14:1–4.
4. Gardner DK, Lane M. Culture and selection of viable blastocysts: a feasible proposition for human IVF? Hum Reprod Update. 1997; 3:367–382.
5. Pool TB, Atiee SR, Martin JE. Oocyte and embryo culture: basic concepts and recent advances. Infert Reprod Med Clinics N Amer. 1998; 9:181–203.
6. Tsirigotis M. Blastocyst stage transfer: pitfalls and benefits. Too soon to abandon current practice? Hum Reprod. 1998; 13:3285–3289.

7. Gardner DK, Schoolcraft WB. No longer neglected: the human blastocyst. Hum Reprod. 1998; 13:3289–3292.

8. Gardner DK, Balaban B. Choosing between day 3 and day 5 embryo transfers. Clin Obstet Gynecol. 2006; 49:85–92.

9. Blake DA, Farquhar CM, Johnson N, Proctor M. Cleavage stage versus blastocyst stage embryo transfer in assisted conception. Cochrane Database Syst Rev. 2007; CD002118.

10. Papanikolaou EG, Kolibianakis EM, Tournaye H, Venetis CA, Fatemi H, Tarlatzis B, et al. Live birth rates after transfer of equal number of blastocysts or cleavage-stage embryos in IVF. A systematic review and meta-analysis. Hum Reprod. 2008; 23:91–99.

11. Glujovsky D, Blake D, Farquhar C, Bardach A. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2012; 7:CD002118.

12. Hreinsson J, Rosenlund B, Fridström M, Ek I, Levkov L, Sjöblom P, et al. Embryo transfer is equally effective at cleavage stage and blastocyst stage: a randomized prospective study. Eur J Obstet Gynecol Reprod Biol. 2004; 117:194–200.

13. Kolibianakis EM, Zikopoulos K, Verpoest W, Camus M, Joris H, Van Steirteghem AC, et al. Should we advise patients undergoing IVF to start a cycle leading to a day 3 or a day 5 transfer. Hum Reprod. 2004; 19:2550–2554.

14. Papanikolaou EG, D'haeseleer E, Verheyen G, Van de Velde H, Camus M, Van Steirteghem A, et al. Live birth rate is significantly higher after blastocyst transfer than after cleavage-stage embryo transfer when at least four embryos are available on day 3 of embryo culture. A randomized prospective study. Hum Reprod. 2005; 20:3198–3203.

15. Papanikolaou EG, Camus M, Kolibianakis EM, Van Landuyt L, Van Steirteghem A, Devroey P. In vitro fertilization with single blastocyst-stage versus single cleavage-stage embryos. N Engl J Med. 2006; 354:1139–1146.

16. Fisch JD, Adamowicz M, Hackworth J, Ginsburg M, Keskintepe L, Sher G. Single embryo transfer (SET) day 3 vs. day 5 based on graduated embryo score (GES) and soluble human leukocyte antigen-g (sHLA-G): preliminary results of a prospective, randomized controlled trial. Fertil Steril. 2007; 88:Suppl 1. S332–S333.

17. Brugnon F, Bouraoui Z, Ouchchane L, Gremeau AS, Peikrishvili R, Pouly JL, et al. Cumulative pregnancy rates after single cleavage-stage versus blastocyst-stage embryo transfer: A randomized and prospective study. Hum Reprod. 2010; 25:Suppl 1. i60–i61. doi: 10.1093/humrep/de.25.s1.41.
18. Elgindy EA, Abou-Setta AM, Mostafa MI. Blastocyst-stage versus cleavage-stage embryo transfer in women with high oestradiol concentrations: randomized controlled trial. Reprod Biomed Online. 2011; 23:789–798.

19. Källén B, Finnström O, Lindam A, Nilsson E, Nygren KG, Olausson PO. Blastocyst versus cleavage stage transfer in in vitro fertilization: differences in neonatal outcome? Fertil Steril. 2010; 94:1680–1683.

20. Pantos K, Stavrou D, Pichos I, Grammatis M, Pappas K, Dafereras A, et al. The successful use of hatched blastocysts in assisted reproductive technology. Clin Exp Obstet Gynecol. 2001; 28:113–117.
21. Palmer GA, Traeger-Synodinos J, Davies S, Tzetis M, Vrettou C, Mastrominas M, et al. Pregnancies following blastocyst stage transfer in PGD cycles at risk for beta-thalassaemic haemoglobinopathies. Hum Reprod. 2002; 17:25–31.

22. Frattarelli JL, Leondires MP, McKeeby JL, Miller BT, Segars JH. Blastocyst transfer decreases multiple pregnancy rates in in vitro fertilization cycles: a randomized controlled trial. Fertil Steril. 2003; 79:228–230.

24. Bourgain C, Devroey P. The endometrium in stimulated cycles for IVF. Hum Reprod Update. 2003; 9:515–522.

25. Fleming R, Jenkins J. The source and implications of progesterone rise during the follicular phase of assisted reproduction cycles. Reprod Biomed Online. 2010; 21:446–449.

26. Papanikolaou EG, Kolibianakis EM, Pozzobon C, Tank P, Tournaye H, Bourgain C, et al. Progesterone rise on the day of human chorionic gonadotropin administration impairs pregnancy outcome in day 3 single-embryo transfer, while has no effect on day 5 single blastocyst transfer. Fertil Steril. 2009; 91:949–952.

27. Papanikolaou EG, Camus M, Fatemi HM, Tournaye H, Verheyen G, Van Steirteghem A, et al. Early pregnancy loss is significantly higher after day 3 single embryo transfer than after day 5 single blastocyst transfer in GnRH antagonist stimulated IVF cycles. Reprod Biomed Online. 2006; 12:60–65.

28. Tadin I, Roje D, Banovic I, Karelovic D, Mimica M. Fetal reduction in multifetal pregnancy--ethical dilemmas. Yonsei Med J. 2002; 43:252–258.

29. Practice Committee of American Society for Reproductive Medicine. Practice Committee of Society for Assisted Reproductive Technology. Blastocyst culture and transfer in clinical-assisted reproduction. Fertil Steril. 2008; 90:5 Suppl. S174–S177.
30. Magli MC, Jones GM, Gras L, Gianaroli L, Korman I, Trounson AO. Chromosome mosaicism in day 3 aneuploid embryos that develop to morphologically normal blastocysts in vitro. Hum Reprod. 2000; 15:1781–1786.

31. Staessen C, Platteau P, Van Assche E, Michiels A, Tournaye H, Camus M, et al. Comparison of blastocyst transfer with or without preimplantation genetic diagnosis for aneuploidy screening in couples with advanced maternal age: a prospective randomized controlled trial. Hum Reprod. 2004; 19:2849–2858.

32. Sandalinas M, Sadowy S, Alikani M, Calderon G, Cohen J, Munné S. Developmental ability of chromosomally abnormal human embryos to develop to the blastocyst stage. Hum Reprod. 2001; 16:1954–1958.

33. Strandell A, Thorburn J, Hamberger L. Risk factors for ectopic pregnancy in assisted reproduction. Fertil Steril. 1999; 71:282–286.

34. Fanchin R, Ayoubi JM, Righini C, Olivennes F, Schönauer LM, Frydman R. Uterine contractility decreases at the time of blastocyst transfers. Hum Reprod. 2001; 16:1115–1119.

35. Schoolcraft WB, Surrey ES, Gardner DK. Embryo transfer: techniques and variables affecting success. Fertil Steril. 2001; 76:863–870.

36. Gardner DK, Vella P, Lane M, Wagley L, Schlenker T, Schoolcraft WB. Culture and transfer of human blastocysts increases implantation rates and reduces the need for multiple embryo transfers. Fertil Steril. 1998; 69:84–88.

37. Ménézo YJ, Hamamah S, Hazout A, Dale B. Time to switch from co-culture to sequential defined media for transfer at the blastocyst stage. Hum Reprod. 1998; 13:2043–2044.

38. Balaban B, Urman B. Comparison of two sequential media for culturing cleavage-stage embryos and blastocysts: embryo characteristics and clinical outcome. Reprod Biomed Online. 2005; 10:485–491.

39. Van Royen E, Mangelschots K, De Neubourg D, Valkenburg M, Van de Meerssche M, Ryckaert G, et al. Characterization of a top quality embryo, a step towards single-embryo transfer. Hum Reprod. 1999; 14:2345–2349.

40. Coskun S, Hollanders J, Al-Hassan S, Al-Sufyan H, Al-Mayman H, Jaroudi K. Day 5 versus day 3 embryo transfer: a controlled randomized trial. Hum Reprod. 2000; 15:1947–1952.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download