Abstract
Purpose
Plantarmedial release and first ray extension osteotomy are often combined to treat paralytic cavovarus foot deformity. The purpose of this study is to evaluate the effect of additional first ray extension osteotomy in terms of dynamic pedobarography.
Materials and Methods
We reviewed findings of pre- and postoperative plain radiography and dynamic pedobarography for 25 patients in whom the flexibility of the hindfoot was confirmed by the Coleman block test. The results of treatment by extensive plantar medial release with first ray osteotomy (group I) were compared with the results of treatment by extensive plantar medial release alone (group II).
Foot deformity is one of the most frequent orthopedic problems in neuromuscular disease and is caused by imbalances between the intrinsic and extrinsic muscles. Cavovarus foot deformity, which increases the height of the medial longitudinal arch and induces heel varus, may develop in patients with cerebral palsy, myelomeningocele, poliomyelitis, Charcot-Marie-Tooth disease, and other neuromuscular diseases.1,2,3
The purpose of treatment for paralytic cavovarus is to improve the flexibility and stability of the foot and to promote a plantigrade foot. This evens the distribution of plantar force and enables the use of a brace. Surgery for paralytic cavovarus may be classified as soft tissue release, osteotomy, fusion, and a combination of these procedures.2,3,4,5,6,7 A good outcome may be anticipated depending on the use of a surgical technique appropriate for the cause of disease, age at the time of surgery, and especially the flexibility of the foot.5,7,8 Cavovarus creates a tripod effect, in which plantar flexion of the first ray induces forefoot pronation and hindfoot varus develops.5,9 When the flexibility of the hindfoot varus is confirmed by the Coleman block test,9 selective soft tissue release and midfoot or forefoot osteotomies are generally recommended.6,9,10,11
However, the combination of soft tissue release and midfoot or forefoot osteotomies was decided subjectively by the operator. Although radiographic correction or clinical improvement of cavovarus with flexible hindfoot after surgery has been reported, these outcomes cannot directly be compared because the investigators have used different techniques for treatment. Furthermore, many studies had only evaluated static changes in terms of radiological observations.
We reviewed medical records for patients who underwent extensive plantar medial release with elective first ray osteotomy for paralytic cavovarus foot deformity with flexible hindfoot varus. Using plain radiography and dynamic pedobarography, we evaluated the effect of the addition of the first ray extension osteotomy in paralytic cavovarus foot deformity with flexible hindfoot varus.
This study was approved by the Institutional Review Board of our hospital. Pediatric patients below 16 years old with neuromuscular disease and cavovarus foot deformity who were able to walk without assistive devices and underwent extensive plantar medial release from March 2005 to April 2009 were recruited. The exclusion criteria were: 1) use of any kind of tendon transfer surgery around ankle, such as tibialis anterior or posterior split transfer, 2) presence of other skeletal deformity, such as hip dislocation or subluxation, knee contracture, excessive femoral anteversion above 50 degrees, excessive external tibial torsion above 40 degrees, excessive internal tibial torsion above 15 degrees and excessive varus or valgus ankle deformity. Flexibility of the hindfoot was confirmed in these patients using the Coleman block test (Fig. 1), and hindfoot varus was determined to be <5 mm using the radiological test suggested by Paulos, et al.5
Twenty five patients (37 affected feet) who were available for follow-up for a minimum of 2 years after surgery were included in this study. This included 15 boys and 10 girls with a mean age of 9 years and 11 months (range, 4 years and 3 months to 15 years and 6 months) at the time of surgery. The average follow-up period was 25 months (range, 16-58 months). Cavovarus foot deformity was caused by myelomeningocele in 26 cases, Charcot-Marie-Tooth disease in 7 cases, and spinal tumor resection in 4 cases. All patients were able to walk independently before and after surgery, and weight-bearing radiological measurements and dynamic pedobarography were performed.
Extensive plantarmedial release began with a medial incision, followed by release of the abductor hallucis from the first metatarsal bone and exposure of the plantarmedial area. After confirming the medial and lateral plantar nerves and blood vessels, Z-lengthening was performed on the flexor hallucis longus and the flexor digitorum longus, if required. Contractured ligaments of the subtalar joint, talonavicular joint, plantar fascia, and muscles originating from the tarsal bone were also released. As a first ray osteotomy, a first metatarsal extension wedge osteotomy was performed in 21 feet, and a medial cuneiform extension wedge osteotomy was performed in 1 foot.
For correcting equinus, the Achilles tendon was lengthened in 27 feet. In 5 feet in which equinus deformity was not sufficiently corrected by lengthening of the Achilles tendon, posterolateral release was performed by additional release of calcaneofibular ligament and capsulotomy of tibiotalar and subtalar joint. In 4 feet, although the tibia external rotation was below 40 degrees, distal tibial rotational osteotomy was performed to make tibia rotation similar to the contralateral side. Tendon transfer was not performed in any case.
The first metatarsal-talus angle and the talocalcaneal angle were measured on pre- and postoperative weight-bearing anteroposterior radiographs. The talocalcaneal angle, calcaneal pitch, first metatarsal-talus angle (Meary angle), and first metatarsal-calcaneus angle (Hibb's angle) were measured on lateral radiographs.
F-scan (Tekscan High Resolution Pressure Assessment System, South Boston, MA, USA) was used to measure dynamic foot pressure. Pressure was recorded at 50 Hz using a pressure-sensitive insole consisting of a 0.15-mm-thick sensor with an embedded grid-work of 960 pressure-sensing cells distributed evenly at 0.5-cm intervals. Before use, a disposable insole was trimmed to fit into each patient's shoes. Patients walked approximately 20 meters to acquaint themselves with the system. Foot pressure in 9 areas, namely, the hallux, 5 metatarsal heads, midfoot, medial calcaneus, and lateral calcaneus, was recorded for 5 steps in the middle of the test walk, and the mean value was calculated. The pressure-reading data were saved and then processed using custom-made software (FSCAN version 4.19F). The pressure-time data for each individual area were graphed using a normalized pressure and time scale. The peak forces (PF) of each area were obtained during the stance phase.
To evaluate the effects of first ray osteotomy on the outcome, we compared results for 22 feet treated with a first metatarsal extension wedge osteotomy and medial cuneiform extension wedge osteotomy (group I) with results for 15 feet not treated with osteotomy (group II). At the time of surgery, the mean age of the patients was 10 years and 8 months (range, 4 years and 3 months to 15 years and 6 months) in group I and 8 years and 5 months (range, 4 years and 3 months to 15 years and 2 months) in group II (p=0.765). In group I, posterolateral release was performed in 2 feet and Achilles tendon lengthening in 18 feet. In group II, posterolateral release was performed in 3 feet and Achilles tendon lengthening in 9 feet.
The plantar force measurements and radiographic findings of patients were compared with corresponding data for 16 normal individuals older than 4 years. To minimize measurement errors, 2 fellowship-trained pediatric orthopedic surgeons obtained all radiographic and pedobarographic measurements. All parameters were measured twice by each author, and these measurements were then averaged. Statistical analyses were performed using the SAS software package (version 9.1, SAS Institute, Cary, NC, USA).
To ensure validity of the results and to identify significant group differences, a mixed model was used to enable repeated measurements from individual patients and was adjusted for intra-person correlations. In addition, to adjust for the effects of age, gender, leg length, and time to assessment, we performed multivariate analysis. The values measured on plain radiographs and dynamic pedobarographs were compared between groups. The level of significance was set at p<0.05.
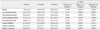
Values measured on the anteroposterior and lateral views of weight-bearing radiographs did not differ significantly between groups, except for postoperative calcaneal pitch (Table 1). Although anteroposterior 1st metatarsal-talus angle, Meary angle and Hibb's angle were slightly improved after operation, there was no statistically significant improvement in the radiologic indices in both groups (p=0.192, 0.520, 0.205, 0.269, 0.529, 0.476 in group I and 0.369, 0.745, 0.090, 0.210, 0.799, 0.537 in group II, respectively) (Fig. 2).
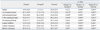
Preoperatively, the PF at the medial and lateral calcaneus were higher in group I than in group II. PF at the hallux, first through fourth metatarsal heads, and medial and lateral calcaneus were lower in both groups than in normal controls, but did not differ significantly from controls in the midfoot (Table 2).
Postoperatively, PF at the first through fourth metatarsal heads were higher in group I than in group II. PF at each area, except for the first metatarsal head in group I and the midfoot in group II, were lower than those in normal controls (Table 3).
Only in group I, PF at the 1st metatarsal head (p=0.015), 2nd metatarsal head (p=0.024) and medial calcaneus (p=0.041) were increased after operation (p=0.483, 0.362, 0.200, 0.148, 0.293 in other areas, respectively). There were no significant changes in group II after operation (p=0.079, 0.833, 0.614, 0.686, 0.753, 0.457, 0.232, 0.079, respectively).
Pes cavovarus is a multidimensional deformity involving several joints in the foot and may require a combination of surgical treatments depending on the level of deformity. The choice of surgical technique generally depends on the level of flexibility in the hindfoot varus.9 Reports suggest that simple plantar release provides satisfactory results for feet with hindfoot flexibility, whereas feet with relative stiffness respond better to extensive plantarmedial release.5 McCluskey, et al.2 recommended that soft tissue release and tendon transfer be performed for patients aged <8 years with flexible hindfoot varus, and that extensive plantar medial release or calcaneal osteotomy be used for patients aged >12 years with stiff hindfoot varus.
Some conflicting results from previous studies indicate a primary dependence on the clinical judgment and experience of the surgeon to decide the course of treatment.3,5,6,12 For example, the Coleman block test,9 is judged by clinical criteria. Furthermore, studies that used combined surgical methods cannot evaluate outcomes for a single procedure. In this study, therefore, we selected patients with paralytic cavovarus and confirmed the flexibility in the hindfoot using the Coleman block test.9 Furthermore, we further selected patients with hindfoot varus <5 mm, measured by the radiological reference suggested by Paulos, et al.,5 and extensive plantarmedial release alone was the only soft tissue surgery to correct cavovarus in this study.
If extensive plantar medial release alone did not provide satisfactory correction, first ray osteotomy was added. First ray osteotomy is performed to improve the cavus and varus of the hindfoot by correcting the forefoot pronation resulting from the tripod effect.6 When soft tissue release does not adequately correct the cavovarus, an extension osteotomy on the first metatarsal bone or the medial cuneiform bone may improve the hindfoot varus.3 Nevertheless, the use of osteotomy is based on the age of the patient or the surgeon's discretion during surgery, rather than on objective criteria. Azmaipairashvili, et al.13 reported that the degree of forefoot pronation, as measured using lateral radiographic views obtained while performing the Coleman block test, may indicate the need for metatarsal osteotomy. In our study, although we did not assess lateral radiographic views during the Coleman block test, groups I and II did not differ significantly in the other radiological assessments, either pre- or postoperatively. These measurements of static deformity alone cannot be used to evaluate the outcome of the addition of first ray osteotomy or suggest indications of the additional first ray osteotomy.
Previous studies have been based on radiological measurements of the Meary angle, reflecting the level of cavovarus correction, or on measurements of the talocalcaneal angle, reflecting the correction of hindfoot varus. However, the cavovarus foot deformity increases pressure on the lateral midfoot, which promotes ulceration of the foot and instability while walking. This condition requires dynamic evaluation. The measurement of dynamic foot pressure can be used to evaluate the pressure on the foot during walking at a single point in time. This measurement can also be used to evaluate the imbalances at each area of the foot as force changes throughout the gait cycle. Static radiological assessment cannot provide the same type or quantity of information.11,14,15,16
In both groups, peak forefoot and calcaneal forces were lower than those in normal controls, and only the peak midfoot force was similar. Metaxiotis, et al.16 used measurements of dynamic plantar pressure to classify adult cavovarus into 3 types. In type 1, the pressure at the first metatarsal head and the midfoot are high; in type 2, the pressure at each metatarsal head is high; and in type 3, pressure is high at the fifth metatarsal head and the lateral midfoot area. Although parameters of groups I and II in our study, did not fit well into the Metaxiotis classification, they did resemble a type 3, because forces at the metatarsal heads were decreased and midfoot were increased.
In dynamic foot pressure, patients in group I had increased PF at calcaneus than group II. However, those are lower than normal control. After operation, only PF at the 1st metatarsal head, 2nd metatarsal head and medial calcaneus in group I were increased, but only PF at the 1st metatarsal head was comparable to the normal control. In group II, there were no significant changes after operation and postoperatively PF at 1-4th metatarsal heads were lower than group I. In our study, we cannot suggest the indication of the addition of first ray extension osteotomy because there was a little difference between groups. However, the addition of first ray extension osteotomy increased forefoot peak pressure compared with extensive plantarmedial release alone (Fig. 3).
Because this was a retrospective study, we cannot suggest the indication of first ray osteotomy. However, in terms of radiography, we can conclude that the preoperative static deformity did not differ significantly between patients who required an additional first ray osteotomy and those who required only extensive plantarmedial release. In terms of dynamic pedobarography, patients who received a first ray osteotomy showed improvement in peak pressure distribution than patients in group II.
Our study considered only paralytic cavovarus foot deformity, apart from the underlying disease. Because of the different manifestation according to the different neuromuscular disease entity, research about the single disease entity would give more information about the effect of the surgery. We did not consider about the imbalance of the extrinsic tendon, because we excluded patients who had undergone tendon transfer. However, the imbalance of the extrinsic tendon can affect the foot pressure distribution. Results of our study can apply to patients with minimal imbalance. Although we found differences in dynamic foot function that may indicate the need for first ray osteotomy, a larger prospective study is required to confirm and extend these indications. Nevertheless, when selecting a surgical procedure for patients with paralytic cavovarus, findings of dynamic pedobarography should be considered in addition to radiographic findings.
Figures and Tables
Fig. 2
Ten year old boy with myelomeningocele has a cavovarus deformity. He underwent extensive plantarmedial release with Achilles tendon lengthening. Preoperative (A) and postoperative (B) standing lateral foot radiography was compared. After operation, Hibb's angle was increased from 124 degree to 126 degree and Meary angle was decreased from 21 degree to 15 degree.

Fig. 3
After operation, the peak forces in the forefoot area were increased in group I, but still decreased in group II.

Table 1
Comparisons of Pre- and Post-Operative Radiographic Parameters (Degree) between Group I and II

References
1. Holmes JR, Hansen ST Jr. Foot and ankle manifestations of Charcot-Marie-Tooth disease. Foot Ankle. 1993; 14:476–486.

2. McCluskey WP, Lovell WW, Cummings RJ. The cavovarus foot deformity. Etiology and management. Clin Orthop Relat Res. 1989; 27–37.
3. Schwend RM, Drennan JC. Cavus foot deformity in children. J Am Acad Orthop Surg. 2003; 11:201–211.

4. Mubarak SJ, Van Valin SE. Osteotomies of the foot for cavus deformities in children. J Pediatr Orthop. 2009; 29:294–299.

5. Paulos L, Coleman SS, Samuelson KM. Pes cavovarus. Review of a surgical approach using selective soft-tissue procedures. J Bone Joint Surg Am. 1980; 62:942–953.

6. Samilson RL, Dillin W. Cavus, cavovarus, and calcaneocavus. An update. Clin Orthop Relat Res. 1983; 125–132.
7. Sherman FC, Westin GW. Plantar release in the correction of deformities of the foot in childhood. J Bone Joint Surg Am. 1981; 63:1382–1389.

8. Jahss MH. Evaluation of the cavus foot for orthopedic treatment. Clin Orthop Relat Res. 1983; 52–63.

9. Coleman SS, Chesnut WJ. A simple test for hindfoot flexibility in the cavovarus foot. Clin Orthop Relat Res. 1977; 60–62.

10. Drennan JC. Current concepts in myelomeningocele. Instr Course Lect. 1999; 48:543–550.
11. Herring JA. Tachdjian's pediatric orthopaedics. 4th ed. Philadelphia: WB Saunders Co;2008. p. 1139–1186.
12. Bradley GW, Coleman SS. Treatment of the calcaneocavus foot deformity. J Bone Joint Surg Am. 1981; 63:1159–1166.

13. Azmaipairashvili Z, Riddle EC, Scavina M, Kumar SJ. Correction of cavovarus foot deformity in Charcot-Marie-Tooth disease. J Pediatr Orthop. 2005; 25:360–365.

14. Chang CH, Miller F, Schuyler J. Dynamic pedobarograph in evaluation of varus and valgus foot deformities. J Pediatr Orthop. 2002; 22:813–818.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download