Abstract
Purpose
A recent study demonstrated that exertional desaturation is a predictor of rapid decline in lung function in patients with chronic obstructive pulmonary disease (COPD); however, the study was limited by its method used to detect exertional desaturation. The main purpose of this study was to explore whether exertional desaturation assessed using nadir oxygen saturation (SpO2) during the 6-minute walk test (6MWT) can predict rapid lung function decline in patients with COPD.
Materials and Methods
A retrospective analysis was performed on 57 patients with moderate to very severe COPD who underwent the 6MWT. Exertional desaturation was defined as a nadir SpO2 of <90% during the 6MWT. Rapid decline was defined as an annual rate of decline in forced expiratory volume in 1 second (FEV1) ≥50 mL. Patients were divided into rapid decliner (n=26) and non-rapid decliner (n=31) groups.
Results
A statistically significant difference in exertional desaturation was observed between rapid decliners and non-rapid decliners (17 vs. 8, p=0.003). No differences were found between the groups for age, smoking status, BODE index, and FEV1. Multivariate analysis showed that exertional desaturation was a significant independent predictor of rapid decline in patients with COPD (relative risk, 6.8; 95% CI, 1.8 to 25.4; p=0.004).
Chronic obstructive pulmonary disease (COPD) is characterized by persistent airflow limitation that is usually progressive and associated with an enhanced chronic inflammatory response to noxious particles or gases in the airways and the lung. COPD is a leading cause of morbidity and mortality worldwide, with an economic and social burden that is both substantial and increasing.1 It is now widely recognized that COPD is a complex syndrome in which significant heterogeneity exists with respect to clinical presentation, physiology, imaging, response to therapy, decline in lung function, and survival.2
As the disease progresses, alveolar hypoxia and consequent hypoxemia are more prevalent. Chronic hypoxemia is associated with the development of adverse sequelae, including pulmonary hypertension, polycythemia, systemic inflammation, skeletal muscle dysfunction, and neurocognitive dysfunction.3 A combination of these factors leads to reduced health-related quality of life and exercise tolerance, and ultimately increased risk of death in patients with COPD.4 Although the main cause of resting hypoxemia in individuals with COPD is considered to be ventilation-perfusion mismatching, other causes such as reduced mixed venous oxygen tension may play a important role in hypoxemia during exercise.5 The prevalence of exertional desaturation without resting hypoxemia in COPD is unknown, but is estimated to be not so rare according to recent reports.6,7 Moreover, COPD patients with exertional desaturation were reported to exhibit a higher mortality than those without exertional desaturation.8, 9, 10
It is well established that patients with COPD lose lung function at a steeper rate than subjects without COPD. The rate of decline in lung function has been traditionally used to indicate disease progression. A number of studies have shown that smoking status affects the rate of lung function decline.11 Meanwhile, a recent report from the Hokkaido COPD Cohort study found that emphysema severity was independently associated with rapid annual decline of lung function.12 This association between baseline radiologic burden of emphysema and subsequent decline in lung function is consistent with other recently published data.13,14 The Korean Obstructive Lung Disease (KOLD) study group recently proposed exertional desaturation as a potential clinical parameter associated with rapid lung function decline in their most recent report, but the study was limited in terms of its definition of exertional desaturation.7
The main purpose of this study was to explore whether exertional desaturation assessed using nadir oxygen saturation can predict rapid lung function decline in patients with COPD. We also attempted to identify other long-term clinical outcomes in COPD patients with exertional desaturation, such as the need for oxygen therapy and death.
A retrospective analysis was performed in patients with moderate to very severe COPD who underwent a 6-minute walk test (6MWT) at Kangdong Sacred Heart Hospital of Hallym University Medical Center (Seoul, Korea) between January 2007 and June 2010. The inclusion criteria for the present study were a smoking history ≥10 pack-years; a ratio of forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) <0.7; FEV1 <80% of predicted; and an oxygen saturation (SpO2) on room air ≥90% according to pulse oximetry.
Among 80 subjects who underwent 6MWT, 23 patients did not satisfy the inclusion criteria (15 patients had a smoking history of less than 10 pack-years and 8 patients had a FEV1 ≥80% of predicted). Finally, a total of 57 patients with moderate to very severe COPD were included. The study was approved by the Kangdong Sacred Heart Hospital Institutional Review Board (Approval No. 12-2-041).
Spirometry was performed using Vmax 22 (Sensor Medics, Yorba Linda, CA, USA) and PFDX (Medgraphics, St. Paul, MN, USA), as recommended by the American Thoracic Society.15 The following values were obtained: FEV1, FVC, and FEV1/FVC ratio. Post-bronchodilator spirometry values were obtained 15 minutes after the administration of a 400 µg dose of salbutamol, which was delivered via a metered dose inhaler connected to a spacer. The predicted values of FEV1, FVC, and FEV1/FVC ratio were calculated from Korean equations formulated using data from a healthy non-smoking population.16
The methods of the 6MWT were mainly based on the guidelines of the American Thoracic Society.17 The 6MWT was performed indoors, along a flat, straight, enclosed corridor with a hard surface. The walking course was 30 m in length. The patient was instructed to sit at rest in a chair for at least 10 minutes before the test was begun, and during this time, resting heart rate, blood pressure, and SpO2 were monitored. The test was avoided in patients with musculoskeletal problems that limited walking or with cardiovascular contraindications (unstable angina or myocardial infarction during the previous month, a resting heart rate of more than 120, and a systolic blood pressure of more than 100 mm Hg). Patients were instructed to walk as far as possible in a 6-minute time period and to set the pace of ambulation with rest stops as needed. The time elapsed and statements of encouragement were provided at standardized intervals during the test. The total distance walked was measured to the nearest foot and recorded. Nadir SpO2 and post-exercise SpO2 were monitored by a lightweight pulse oximeter. Number of rest periods and duration of rest periods were also measured.
Exercise capacity and exertional desaturation were assessed using the 6MWT. The particular form of exercise taken may affect the ability to detect exertional desaturation in patients with COPD, and the 6MWT been shown to be more sensitive than maximal incremental cycle testing for detecting oxygen desaturation.18 Exertional desaturation was defined as nadir SpO2 of <90% during the 6MWT. Rapid lung function decline was defined as annual rate of decline in FEV1 ≥50 mL over a 2-year period of follow-up.
We calculated the body-mass index (BMI) in kilograms per meters squared. The Charlson index was used to determine the degree of comorbidity.19 The BMI (B), the degrees of airflow obstruction (O) and functional dyspnea (D), and exercise capacity (E) as assessed by the 6MWT were integrated into the BODE index.20 The degree of dyspnea was measured with the use of the modified medical research council (mMRC) dyspnea scale.21
All statistical analyses were performed using the statistical software package SPSS version 12.0.1 (SPSS Inc., Chicago, IL, USA). The assumption of a normal distribution of data was tested with the Shapiro-Wilk statistics. Bivariate comparisons were made using Student's t-test, Mann-Whitney U test, or Pearson's χ2 test. Logistic regression analysis was conducted to identify independent predictors of rapid lung function decline. The last observation carried forward method was used for missing data. All p-values ≤0.05 were considered statistically significant.
The mean age of the 57 patients was 67.8±8.2 years. The sample included only male patients. The mean BMI was 21.1 kg/m2. Average smoking history, measured in terms of pack-years, was 43.6 years. A total of 7 (12.3%) patients were current smokers. During baseline spirometry, the mean FEV1 was 1.26 L/min (47.5% of predicted value) and most patients had moderate to severe COPD, according to the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines. Of these, 43.9% were classified as GOLD II (moderate COPD), 50.9% as GOLD III (severe COPD), and 5.3% as GOLD IV (very severe COPD).
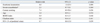
Rapid lung function decline was detected in 26 patients (45.6%) over a 2-year period of follow-up. The baseline data of the rapid decliners (n=26) and the non-rapid decliners (n=31) were then compared. The statistically significant differences observed between the groups were exertional desaturation (p=0.003) and nadir SpO2 (p=0.004) during the 6MWT. The mean change in SpO2 during 6MWT was greater in the rapid decliners. No differences were observed for age, smoking status, FEV1, BMI, mMRC dyspnea scale, BODE index, comorbidity index, 6-minute walk distance, or the use of respiratory medications (Table 1).
The number of patients who visited an emergency department or were hospitalized for exacerbation of COPD was greater among the rapid decliners (38.5%) than the non-rapid decliners (16.1%) during 2 years of follow-up, but this difference was not statistically significant (p=0.074). The mean number of emergency department visits or hospitalizations per patient for 2 years was 0.7 in the rapid decliners, compared with 0.2 in the non-rapid decliners (p=0.071). No significant differences between the groups were observed in terms of the number of patients who visited an emergency department or were hospitalized for respiratory causes (including COPD exacerbation, pneumonia, pneumothorax, lung cancer, non-tuberculous mycobacterial disease, angina, and tachyarrhythmia) for 2 years (Table 2).
Multivariate logistic regression analysis was conducted to indentify independent factors associated with rapid lung function decline in patients with COPD. Exertional desaturation was independently associated with rapid decline, and the relative risk was 6.8 (95% CI, 1.8 to 25.4; p=0.004). However, no statistically significant association was found for severe COPD exacerbation requiring emergency department visit or hospitalization, current smoking, age, BODE index, Charlson index, or FEV1 (Table 3).
Six deaths occurred during the follow-up period, and all of them were in the group of patients with exertional desaturation. Accordingly, death was significantly more frequent in the COPD patients with exertional desaturation (p=0.011). The leading cause of death was pneumonia (n=4). One patient died from hepatocellular carcinoma, and the other was dead on arrival in the emergency department. Meanwhile, two patients among the desaturators required long-term oxygen therapy within 2 years, versus none of the non-desaturators.
The primary aim of this study was to explore whether exertional desaturation, assessed using nadir SpO2, can be a predictor of rapid lung function decline in patients with COPD. We found that exertional desaturation was strongly associated with an increased rate of decline in lung function.
Although many clinical trials of pharmacotherapy for COPD have been conducted, there is no medication for COPD that has been proven to modify long-term decline in lung function. Moreover, patients with COPD exhibit considerable heterogeneity in terms of clinical presentation and disease progression. Therefore, identification of clinical factors related to rapid lung function decline is critical for assessing and treating patients with COPD. So far, smoking status and severity of emphysema assessed by CT scan are the only clinical parameters validated as predictors of rapid lung function decline in large COPD cohorts.12, 13, 14 In a recent report, the KOLD study group suggested exertional desaturation as a potential clinical parameter associated with rapid lung function decline. However, the study was limited in terms of its defining of exertional desaturation.7
In the present study, the mortality rate was significantly higher in the desaturator group. Research has already suggested that COPD patients with exertional desaturation are more likely to have a poor prognosis in terms of mortality.8, 9, 10 However, no previous studies have estimated the value of exertional desaturation as a predictor of rapid lung function decline in patients with COPD, except the report of the KOLD study group.7 In the KOLD cohort study, exertional desaturation was defined as a post-exercise SpO2 of <90% or a ≥4% decrease compared to baseline. That study revealed statistically significant differences between the desaturator and non-desaturator groups in terms of change in FEV1 over three years. However, the authors pointed out the definition of exertional desaturation as a limitation, because the availability of nadir SpO2 may have led to the identification of more patients with exertional desaturation. Therefore, the present study has an advantage over the KOLD cohort study in the aspect of using nadir SpO2 of <90% during the 6MWT rather than post-exercise SpO2 in defining exertional desaturation. Perhaps, nadir SpO2 may be a more precise measure of identifying patients with exertional desaturation, as it is allowed to set the pace of ambulation with rest stops as needed during 6MWT. Actually, in our data, eight patients with a nadir SpO2 of <90% showed a post-exercise SpO2 of ≥90%, but all patients with a post-exercise SpO2 of <90% demonstrated a nadir SpO2 of <90%. Mean post-exercise SpO2 was also numerically greater than nadir SpO2. Consequently, the present study reconfirmed one of the KOLD study results with a more exact definition using a different statistical method. Exertional desaturation can be easily assessed using the relatively simple 6MWT, and the 6MWT is a valuable test for identifying rapid decliners among patients with COPD.
As previously stated, smoking status is closely related to the rate of lung function decline.11 Exacerbations of COPD are also well known to accelerate the rate of decline in lung function.22,23 Therefore, we included current cigarette smoking and severe COPD exacerbation requiring emergency department visits or hospitalization in the present logistic regression analysis. The number of current smokers was too small to evaluate a difference between the rapid decliners and the non-rapid decliners, and the cumulative cigarette smoking exposure expressed as pack-years did not differ significantly between the rapid decliners and the non-rapid decliners. However, the number of patients with a severe exacerbation and the mean number of severe exacerbations per patient were greater in the rapid decliners. Nevertheless, the difference was not statistically significant, probably due to the small sample size of the study.
There is no uniform definition of rapid lung function decline in patients with COPD. Pertaining to the effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1, the Lung Health Study reported that the average annual decrease in FEV1 was greater in the usual care group (53.4 mL) than in the smoking intervention-only group (41.8 mL) and the group assigned to smoking intervention and inhaled anticholinergics (36.8 mL).24 In the ECLIPSE study, the mean rate of decline in FEV1 was 33 mL per year, and 38% of the participants had an estimated rate of decline more than 40 mL per year.13 Nishimura, et al.12 classified subjects in the Hokkaido COPD cohort study based on the magnitude of annual decline in FEV1 and labeled those of less than the 25th percentile (more than 47.6 mL per year) as rapid decliners. We defined rapid lung function decline as an annual rate of decline in FEV1 ≥50 mL in consideration of the degree of annual decline observed in these trials and the number of subjects of the present study.
The present study had several limitations. First, CT data for assessment of emphysema severity were not available, and were not included in the analysis. Emphysema severity is the only clinical parameter other than smoking status that has been validated as a predictor of rapid lung function decline in COPD. However, the KOLD cohort study and the report of Taguchi, et al.25 showed that CT emphysema severity was independently associated with exertional desaturation.7 Therefore, it may not be necessary to include CT emphysema severity as a covariate in the present logistic regression analysis. Second, the present study was conducted retrospectively with a small number of subjects from a single institute. Third, the sample included only male patients. Therefore, the results cannot be generalized to female COPD patients, since a previous study suggests that gender might influence COPD manifestations.26
In conclusion, the present study suggests that exertional desaturation is an independent predictor of rapid lung function decline in male patients with moderate to very severe COPD. The mortality rate was higher in the desaturator group than in the non-desaturator group. Further studies with larger samples including female patients with COPD and prospective design are warranted to clarify the results of the present study and the feasibility of the 6MWT for estimating rapid decline in lung function in COPD.
Figures and Tables
Table 1
Baseline Characteristics of the Two Study Groups*

FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; mMRC, Modified Medical Research Council; SpO2, oxygen saturation; LAMA, long acting muscarinic antagonist; ICS/LABA, inhaled corticosteroid/long acting beta-2 agonist.
*Plus-minus values are means±SD. The body-mass index is the weight in kilograms divided by the square of the height in meters.
†Change in SpO2 is the mean change in SpO2 during the 6-minute walk test (resting SpO2 minus nadir SpO2).
References
1. From the Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2014. Available from: http://www.goldcopd.org/.
2. Han MK, Agusti A, Calverley PM, Celli BR, Criner G, Curtis JL, et al. Chronic obstructive pulmonary disease phenotypes: the future of COPD. Am J Respir Crit Care Med. 2010; 182:598–604.
3. Kent BD, Mitchell PD, McNicholas WT. Hypoxemia in patients with COPD: cause, effects, and disease progression. Int J Chron Obstruct Pulmon Dis. 2011; 6:199–208.
4. Kim V, Benditt JO, Wise RA, Sharafkhaneh A. Oxygen therapy in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008; 5:513–518.

5. Panos RJ, Eschenbacher W. Exertional desaturation in patients with chronic obstructive pulmonary disease. COPD. 2009; 6:478–487.

6. van Gestel AJ, Clarenbach CF, Stöwhas AC, Teschler S, Russi EW, Teschler H, et al. Prevalence and prediction of exercise-induced oxygen desaturation in patients with chronic obstructive pulmonary disease. Respiration. 2012; 84:353–359.

7. Kim C, Seo JB, Lee SM, Lee JS, Huh JW, Lee JH, et al. Exertional desaturation as a predictor of rapid lung function decline in COPD. Respiration. 2013; 86:109–116.

8. Tojo N, Ichioka M, Chida M, Miyazato I, Yoshizawa Y, Miyasaka N. Pulmonary exercise testing predicts prognosis in patients with chronic obstructive pulmonary disease. Intern Med. 2005; 44:20–25.

9. Takigawa N, Tada A, Soda R, Date H, Yamashita M, Endo S, et al. Distance and oxygen desaturation in 6-min walk test predict prognosis in COPD patients. Respir Med. 2007; 101:561–567.

10. Casanova C, Cote C, Marin JM, Pinto-Plata V, de Torres JP, Aguirre-Jaíme A, et al. Distance and oxygen desaturation during the 6-min walk test as predictors of long-term mortality in patients with COPD. Chest. 2008; 134:746–752.

11. Lee PN, Fry JS. Systematic review of the evidence relating FEV1 decline to giving up smoking. BMC Med. 2010; 8:84.
12. Nishimura M, Makita H, Nagai K, Konno S, Nasuhara Y, Hasegawa M, et al. Annual change in pulmonary function and clinical phenotype in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012; 185:44–52.

13. Vestbo J, Edwards LD, Scanlon PD, Yates JC, Agusti A, Bakke P, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med. 2011; 365:1184–1192.

14. Mohamed Hoesein FA, de Hoop B, Zanen P, Gietema H, Kruitwagen CL, van Ginneken B, et al. CT-quantified emphysema in male heavy smokers: association with lung function decline. Thorax. 2011; 66:782–787.

15. Standardization of Spirometry, 1994 Update. American Thoracic Society. Am J Respir Crit Care Med. 1995; 152:1107–1136.
16. Choi JK, Paek D, Lee JO. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005; 58:230–242.

17. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002; 166:111–117.
18. Poulain M, Durand F, Palomba B, Ceugniet F, Desplan J, Varray A, et al. 6-minute walk testing is more sensitive than maximal incremental cycle testing for detecting oxygen desaturation in patients with COPD. Chest. 2003; 123:1401–1407.

19. Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994; 47:1245–1251.

20. Celli BR, Cote CG, Marin JM, Casanova C, Montes de Oca M, Mendez RA, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004; 350:1005–1012.

21. Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988; 93:580–586.

22. Kanner RE, Anthonisen NR, Connett JE. Lung Health Study Research Group. Lower respiratory illnesses promote FEV(1) decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease: results from the lung health study. Am J Respir Crit Care Med. 2001; 164:358–364.

23. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002; 57:847–852.

24. Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, et al. Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. JAMA. 1994; 272:1497–1505.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download