Abstract
Purpose
ST-elevation myocardial infarction (STEMI) patients may visit the emergency department (ED) complaining of sensations of pain other than the chest. We investigated our performance of reperfusion therapy for STEMI patients presenting with non-chest pains.
Materials and Methods
This was a retrospective observational cohort study. STEMI patients who underwent primary percutaneous coronary intervention (PCI) were divided into a chest pain group and a non-chest pain group. Clinical differences between the two groups and the influence of presenting with non-chest pains on door-to-electrocardiograms (ECG) time, door-to-balloon time, and hospital mortality were evaluated.
Results
Of the 513 patients diagnosed with STEMI, 93 patients presented with non-chest pains. Patients in the non-chest pain group were older, more often female, and had a longer symptom onset to ED arrival time and higher Killip class than patients in the chest pain group. There was a statistically significant delay in door-to-ECG time (median, 2.0 min vs. 5.0 min; p<0.001) and door-to-balloon time (median, 57.5 min vs. 65.0 min; p<0.001) in patients without chest pain. In multivariate analysis, presenting with non-chest pains was an independent predictor for hospital mortality (odds ratio, 2.3; 95% confidence interval, 1.1-4.7). However, door-to-ECG time and door-to-balloon time were not factors related to hospital mortality.
Conclusion
STEMI patients presenting without chest pain showed higher baseline risk and hospital mortality than patients presenting with chest pain. ECG acquisition and primary PCI was delayed for patients presenting with non-chest pains, but not influencing hospital mortality. Efforts to reduce pre-hospital time delay for these patients are necessary.
One of the stumbling blocks that delays early diagnosis of myocardial infarction (MI) is that greater than one third of patients do not present with chest pain.1,2,3,4 Such patients may complain of symptoms such as dyspnea, weakness, syncope, mental change, and nausea/vomiting.5,6,7 These patients often are delayed in receiving 12-lead electrocardiogram (ECG). While early identification of these atypical patients is challenging, obtaining an immediate ECG for all patients presenting to the emergency department (ED) would be neither feasible nor cost-effective. Alternatively, Glickman, et al.5 has suggested a triage rule to prioritize patients who should receive a rapid ECG test.6
Timely reperfusion is crucial for the treatment of ST-elevation myocardial infarction (STEMI) patients.8,9 The 2010 American College of Cardiology/American Heart Association guidelines recommend that patients who may have the potential for acute coronary syndrome should have an ECG within 10 minutes of ED arrival and percutaneous coronary intervention (PCI) for STEMI patients should be performed within 90 minutes.10 Delay in receiving an ECG, due to the absence of chest pain complaints, can adversely affect outcomes for STEMI patients. The effect of chief complaints on timely reperfusion therapy and treatment outcomes in STEMI patients, however, is not well known.
In this study, we investigated the clinical characteristics, performance of door-to-ECG time and door-to-balloon time, and consequential hospital mortality in STEMI patients presenting with non-chest pains, compared to patients presenting with chest pain.
This was a retrospective observational cohort study conducted in two urban tertiary care hospitals with a combined ED census of 120000 visits per year for the study period. This study was approved by the hospitals' Institutional Review Board committees. In 2007, a critical pathway (CP) for STEMI patients was implemented in both hospitals to improve the timeliness of reperfusion therapy with primary PCI: After briefly taking a patient's history and reviewing an initial ECG, emergency physicians can contact the coronary catheterization laboratory by clicking the CP button in order communication system, resulting in the simultaneous transmission of a short message to the on-call cardiologist and coronary catheterization staff. Then, a cardiologist makes a final decision on whether to perform primary PCI or not.
We screened patients presenting to the ED between January 1, 2010 and December 31, 2012, who were suspected to have STEMI, and thus, had activated the CP. The ECG criteria for CP activation is based on standard guidelines: ST-segment elevation is defined as J-point elevation on two or more contiguous leads, with a threshold of ≥2 mm in precordial reads or ≥1 mm in other leads. A new or presumed new left bundle branch block is also included in ECG criteria. Among CP activated patients, this study investigated patients who underwent an emergency PCI and were diagnosed as STEMI. Patients who survived out-of-hospital cardiac arrest were excluded, because their chief complaints were unclear. Patients in whom ST-segment elevation was not seen in the initial ECG but emerged in follow-up ECG were also excluded.
Chief complaints, recorded by triage nurse who had at least five years experience working in ED, were extracted from electronic medical records. Because patients expressed their symptoms in various ways, similar symptoms needed to be categorized as one term. For example, synonyms for "chest pain", such as "chest discomfort", "chest tightness", and "chest pressure", were categorized as "chest pain"; meanwhile, "shortness of breath" and "difficulty breathing" were classified into "dyspnea". Some patients had more than one chief complaint. We categorized patients presenting with both "chest pain" and non-chest pain symptoms into "chest pain". In the absence of "chest pain", we prioritized the symptoms suggestive of STEMI and that are included in the Glickman rule: chest pain (in age ≥30 years); weakness, syncope, dyspnea, altered mental change, or upper extremity pain (in age ≥50 years); and abdominal pain or nausea/vomiting (in age ≥80 years).5 Lastly, all patients were divided into a chest pain group and a non-chest pain group.
The timing for patient arrival at the ED, ECG acquisition, STEMI CP activation, and coronary artery ballooning were taken from a hospital database. The time of ECG completion was extracted from computerized ECG logs, which was transmitted to the hospital database. The time of ballooning, where the interventional cardiologist passed the coronary catheter guidewire to the culprit lesion, was collected from the medical records. The time intervals for door-to-balloon time and the composites of door-to-ECG time, ECG-to-CP time, and CP-to-balloon time were analysed. Achieving door-to-ECG time ≤10 min and door-to-balloon time ≤90 min was compared between the two groups.
Patient characteristics, duration of symptoms, mode of ED arrival, initial ED blood pressure and pulse rate, severity of heart failure on admission by Killip class,11 and results of management, including hospital mortality (expiration during admission) and length of stay in hospital, were collected from the medical records.
Comparisons of patient characteristics, treatments, and outcomes between the two groups were conducted using a Student's t-test or Mann-Whitney U test for continuous variables and chi-squared test or Fisher's exact test for dichotomous variables. We used Mann-Whitney U test for the time factors due to a positively skewed distribution. To determine factors associated with door to ECG time, door to balloon time, and hospital mortality, a multivariable logistic regression was performed. A p-value of <0.05 was regarded as statistically significant. Statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software, version 20.0, for Windows (SPSS Inc., Chicago, IL, USA).
During the study period, the CP was activated in 1043 patients who met the ECG criteria. Emergent coronary angiography was performed in 729 (69.9% of total) patients and 560 (76.8%) patients were diagnosed with STEMI. No patients received intravenous fibrinolytic agent. Among 560 STEMI patients, 47 patients were excluded: 23 with out-of-hospital cardiac arrest and 24 with ST-segment elevation on follow-up ECG. Finally, 513 STEMI patients were included in the analysis: 420 (81.8%) patients in the chest pain group and 93 (18.1%) patients in the non-chest pain group.
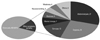
The patients' chief complaints are portrayed in Fig. 1. After chest pain, the most common complaints included abdominal pain (27, 5.3%) and dyspnea (25, 4.9%). Among the 27 patients with abdominal pain, the pain location was the epigastrium in 18 patients. When the Glickman triage rule was applied retrospectively, 91.0% (462/513) of patients could be screened. For patients in the non-chest pain group, 49 of 93 patients met the criteria. There were 24 patients with abdominal pain under the age of 80, who were not included in the Glickman rule.
Demographics and clinical characteristics of patients presenting with non-chest pain were compared with patients presenting with chest pain (Table 1). Patients without chest pain at presentation were significantly older (69.2 years vs. 61.7 years, p<0.001) and female (32.3% vs. 18.6%, p=0.003). They had a higher prevalence of chronic renal failure, stroke and heart failure, and a lower prevalence of being a current smoker. Patients with non-chest pain had a greater delay of onset of symptoms to ED arrival (4.0 hours vs. 0.5 hours, p=0.001), although both groups used ambulances in similar proportions. At initial evaluation, degree of heart failure was more severe in the non-chest pain group, by Killip class III (22.6% vs. 9.5%, p<0.001) and Killip class IV (22.6% vs. 10.5%, p<0.001). Patients with non-chest pains showed a longer duration of hospitalization (p=0.020) and higher hospital mortality than patients with chest pain (p<0.001).
Time intervals are presented in Table 2. Patients in the non-chest pain group had a longer median door-to-balloon time (65.0 min vs. 57.5 min, p<0.001). Time to obtain an ECG was delayed for patients in the non-chest pain group (5 min vs. 2 min, p<0.001). The remaining components of the time interval were similar between the two groups.
An ECG was obtained within 10 minutes for 92.0% of all patients: 95.7% in the chest pain group and 75.3% in the non-chest pain group, p<0.001 (Fig. 2). 93.3% of all patients had a door-to-balloon time within 90 minutes. Reperfusion was delayed for 4.2% of patients presenting with chest pain and 18.0% of patients with non-chest pain (p<0.001).
Table 3 shows the logistic regression analysis for ECG delay (door to ECG time >10 minutes) and balloon delay (door-to-balloon time >90 minutes). Presentation with non-chest pains was the most important predictor for both ECG delay [odds ratio (OR), 6.41; p<0.001] and balloon delay (OR, 4.25; p<0.001). Female gender and walking arrival to the ED were related to the ECG delay, but not related to the balloon delay. Age influenced neither ECG delay nor balloon delay.
Hospital mortality was higher in the non-chest pain group than the chest pain group (17.2% vs. 6.0%). We conducted logistic regression analysis to determine the effects of chief complaints and hospital intervention (ECG and PCI time) on hospital mortality (Table 4). Other variables, such as age, gender, diabetes mellitus, and hypertension, suspected to be associated with hospital mortality of MI, were included in analysis. Age and non-chest pain complaints were identified as independent predictors of hospital mortality. Female gender, door-to-ECG time, and door-to-balloon time were not associated with hospital mortality.
In our study, the proportion of STEMI patients who complained of non-chest pain was 18.1%, which was relatively high, compared to past studies, which reported proportions of 5.2-19.9%.5,8,12,13 Our study population had a higher proportion of Killip class III & IV patients and hospital mortality rates than prior studies. In studies investigating MI patients, including both STEMI and non-STEMI, the number of patients without chest pain increased to 33-47%.1,2,6 The proportion of patients without chest pain presentation in STEMI is lower than in non-STEMI. However, atypical chief complaints in STEMI patients cause a delay in primary PCI and lead to higher fatalities, and thus, deserve greater attention. Unfortunately, the Glickman triage rule for timely detection of STEMI patient screened only half of patients who presented without chest pains. Especially, patients with abdominal pain under the age of 80 accounted for a large part of the omitted patients, and perhaps the age limit of abdominal pain presentation should be extended to heighten sensitivity. There is concern, however, that the efficiency of the screening tool would be reduced because so many patients presenting with abdominal pain visit the ED. Thus the usefulness of a triage tool composed of only age and chief complaint would be limited, despite its simplicity and convenience.
STEMI patients presenting with non-chest pain were more frequently older and female. They had longer symptom onset-to-door time, a higher Killip class on presentation, and a higher hospital mortality rate. Gender and old age have already been shown to be independent predictors of hospital mortality in STEMI patients.2,11,14,15,16,17,18 Several studies reported that being female was related to delayed primary PCI and women had worse outcomes than men.14,15,16,17,19 Our multivariate analysis of presenting with non-chest pains, however, revealed that being female was not an independent predictor for delayed PCI and hospital mortality. This is consistent with the results of prior studies that show that sex differences in mortality rates is caused by baseline comorbidities.20,21 We may reduce the differences in door-to-balloon time between males and females by enhancing reperfusion therapy for patients with non-chest pain presentation. Over the last decade, the hospital process facilitating emergent PCI for STEMI patients has been improved, achieving a shorter door-to-balloon time for all patients.22,23,24,25,26,27 Recently, trials with a focus on high risk patients with delayed PCI reported that triage process changes, triage staff education, and a feedback system could improve the door-to-ECG time and door-to-balloon time of STEMI patients presenting non-chest pain.12,13
Delay in primary PCI is known to be associated with increased mortality for STEMI patients.8,9,28,29 However, there was a poor correlation between the door-to-balloon time and hospital mortality in our results. This may be explained as follows: we achieved the guideline's goal of door-to-ECG time within 10 minutes in 92.0% patients and door-to-balloon time within 90 minutes in 93.3% patients, which shows a higher performance than suggested by existing research that reports a positive correlation between PCI delay and hospital mortality.8,9,30,31 Our high performance was possible because of the implementation of CP for STEMI patients; moreover, we have been continuing education and feedback for staff in the relevant departments, with efforts to reduce the door-to-balloon time, as a quality indicator. Also, our research was performed later than other studies. Decreased variation of reperfusion time for each patient might not have as great an effect on hospital mortality as originally thought. Other researchers proposed a similar opinion that the extent of benefits from earlier PCI reaches a point of diminishing returns and there is little room to reduce mortality.23,32,33,34 Currently, a patient's condition, such as progression of the disease and heart failure on presentation, are considered more important to treatment outcomes.35,36 Recently, some have postulated that the time from the onset of symptoms to reperfusion is a more important determinant of outcomes than door-to-balloon time.33,37 Decreasing delays due to patients is a difficult problem because it requires reducing pre-hospital time. Accordingly, as patients presenting with non-chest pains have longer pre-hospital times, educating the public and emergency medical technicians about symptoms of MI other than chest pain and transportation to hospital without delay are necessary.
This study has several limitations. First, characteristics and competence of triage nurses could affect the recording of chief complaints. Second, it is not easy to get the exact time of symptom onset because of patient reporting errors. Patients frequently do not remember the exact onset time and report an estimate. Because of this limitation, we could not reveal the relationship between symptom onset-to-door time and hospital mortality. Third, high-risk patients are more likely to have pre-hospital arrest events or expire prior to trying a primary PCI. Excluding these patients may diminish the effects of symptom duration on hospital mortality. Lastly, this study was a retrospective cohort analysis based on medical records and we could not collect follow up data concerning the survival of discharged patients. The one-month or long-term mortality may be higher than the hospital mortality reported herein.
In conclusion, STEMI patients presenting without chest pain showed longer door-to-ECG time and door-to-PCI time and higher hospital mortality than patients presenting with chest pain. Non-chest pain presentation was an independent predictor of hospital mortality after the primary PCI. To reduce hospital mortality of these patients, efforts reducing pre-hospital time delay, as well as providing timely reperfusion therapy, is necessary.
Figures and Tables
Fig. 2
Proportion of patients who achieved the goal door-to-ECG time and door-to-balloon time. ECG, electrocardiogram.

References
1. Gupta M, Tabas JA, Kohn MA. Presenting complaint among patients with myocardial infarction who present to an urban, public hospital emergency department. Ann Emerg Med. 2002; 40:180–186.

2. Canto JG, Shlipak MG, Rogers WJ, Malmgren JA, Frederick PD, Lambrew CT, et al. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA. 2000; 283:3223–3229.

3. Coronado BE, Pope JH, Griffith JL, Beshansky JR, Selker HP. Clinical features, triage, and outcome of patients presenting to the ED with suspected acute coronary syndromes but without pain: a multicenter study. Am J Emerg Med. 2004; 22:568–574.

4. Brieger D, Eagle KA, Goodman SG, Steg PG, Budaj A, White K, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004; 126:461–469.

5. Glickman SW, Shofer FS, Wu MC, Scholer MJ, Ndubuizu A, Peterson ED, et al. Development and validation of a prioritization rule for obtaining an immediate 12-lead electrocardiogram in the emergency department to identify ST-elevation myocardial infarction. Am Heart J. 2012; 163:372–382.

6. Graff L, Palmer AC, Lamonica P, Wolf S. Triage of patients for a rapid (5-minute) electrocardiogram: a rule based on presenting chief complaints. Ann Emerg Med. 2000; 36:554–560.

7. Osborne AD, Ali K, Lowery-North D, Capes J, Keadey M, Franks N, et al. Ability of triage decision rules for rapid electrocardiogram to identify patients with suspected ST-elevation myocardial infarction. Crit Pathw Cardiol. 2012; 11:211–213.

8. McNamara RL, Wang Y, Herrin J, Curtis JP, Bradley EH, Magid DJ, et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006; 47:2180–2186.

9. Hannan EL, Zhong Y, Jacobs AK, Holmes DR, Walford G, Venditti FJ, et al. Effect of onset-to-door time and door-to-balloon time on mortality in patients undergoing percutaneous coronary interventions for st-segment elevation myocardial infarction. Am J Cardiol. 2010; 106:143–147.

10. O'Connor RE, Brady W, Brooks SC, Diercks D, Egan J, Ghaemmaghami C, et al. Part 10: acute coronary syndromes: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122:18 Suppl 3. S787–S817.
11. Killip T 3rd, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol. 1967; 20:457–464.
12. Phelan MP, Glauser J, Smith E, Martin C, Schrump S, Mahone P, et al. Improving emergency department door-to-electrocardiogram time in ST segment elevation myocardial infarction. Crit Pathw Cardiol. 2009; 8:119–121.

13. Borden WB, Fennessy MM, O'Connor AM, Mulliken RA, Lee L, Nathan S, et al. Quality improvement in the door-to-balloon times for ST-elevation myocardial infarction patients presenting without chest pain. Catheter Cardiovasc Interv. 2012; 79:851–858.

14. Dreyer RP, Beltrame JF, Tavella R, Air T, Hoffmann B, Pati PK, et al. Evaluation of gender differences in Door-to-Balloon time in ST-elevation myocardial infarction. Heart Lung Circ. 2013; 22:861–869.

15. Kaul P, Armstrong PW, Sookram S, Leung BK, Brass N, Welsh RC. Temporal trends in patient and treatment delay among men and women presenting with ST-elevation myocardial infarction. Am Heart J. 2011; 161:91–97.

16. Angeja BG, Gibson CM, Chin R, Frederick PD, Every NR, Ross AM, et al. Predictors of door-to-balloon delay in primary angioplasty. Am J Cardiol. 2002; 89:1156–1161.

17. Mehta RH, Bufalino VJ, Pan W, Hernandez AF, Cannon CP, Fonarow GC, et al. Achieving rapid reperfusion with primary percutaneous coronary intervention remains a challenge: insights from American Heart Association's Get With the Guidelines program. Am Heart J. 2008; 155:1059–1067.

18. Rathore SS, Curtis JP, Nallamothu BK, Wang Y, Foody JM, Kosiborod M, et al. Association of door-to-balloon time and mortality in patients > or =65 years with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Am J Cardiol. 2009; 104:1198–1203.

19. Benamer H, Tafflet M, Bataille S, Escolano S, Livarek B, Fourchard V, et al. Female gender is an independent predictor of in-hospital mortality after STEMI in the era of primary PCI: insights from the greater Paris area PCI Registry. EuroIntervention. 2011; 6:1073–1079.

20. Eitel I, Desch S, de Waha S, Fuernau G, Gutberlet M, Schuler G, et al. Sex differences in myocardial salvage and clinical outcome in patients with acute reperfused ST-elevation myocardial infarction: advances in cardiovascular imaging. Circ Cardiovasc Imaging. 2012; 5:119–126.

21. Jackson EA, Moscucci M, Smith DE, Share D, Dixon S, Greenbaum A, et al. The association of sex with outcomes among patients undergoing primary percutaneous coronary intervention for ST elevation myocardial infarction in the contemporary era: Insights from the Blue Cross Blue Shield of Michigan Cardiovascular Consortium (BMC2). Am Heart J. 2011; 161:106–112.

22. Gibson CM, Pride YB, Frederick PD, Pollack CV Jr, Canto JG, Tiefenbrunn AJ, et al. Trends in reperfusion strategies, door-to-needle and door-to-balloon times, and in-hospital mortality among patients with ST-segment elevation myocardial infarction enrolled in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008; 156:1035–1044.

23. Flynn A, Moscucci M, Share D, Smith D, LaLonde T, Changezi H, et al. Trends in door-to-balloon time and mortality in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Intern Med. 2010; 170:1842–1849.

24. Bradley EH, Roumanis SA, Radford MJ, Webster TR, McNamara RL, Mattera JA, et al. Achieving door-to-balloon times that meet quality guidelines: how do successful hospitals do it? J Am Coll Cardiol. 2005; 46:1236–1241.
25. Bradley EH, Herrin J, Wang Y, Barton BA, Webster TR, Mattera JA, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006; 355:2308–2320.

26. Willson AB, Mountain D, Jeffers JM, Blanton CG, McQuillan BM, Hung J, et al. Door-to-balloon times are reduced in ST-elevation myocardial infarction by emergency physician activation of the cardiac catheterisation laboratory and immediate patient transfer. Med J Aust. 2010; 193:207–212.

27. Khot UN, Johnson ML, Ramsey C, Khot MB, Todd R, Shaikh SR, et al. Emergency department physician activation of the catheterization laboratory and immediate transfer to an immediately available catheterization laboratory reduce door-to-balloon time in ST-elevation myocardial infarction. Circulation. 2007; 116:67–76.

28. Rathore SS, Curtis JP, Chen J, Wang Y, Nallamothu BK, Epstein AJ, et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ. 2009; 338:b1807.

29. Cannon CP, Gibson CM, Lambrew CT, Shoultz DA, Levy D, French WJ, et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing an gioplasty for acute myocardial infarction. JAMA. 2000; 283:2941–2947.

30. Diercks DB, Kirk JD, Lindsell CJ, Pollack CV Jr, Hoekstra JW, Gibler WB, et al. Door-to-ECG time in patients with chest pain presenting to the ED. Am J Emerg Med. 2006; 24:1–7.

31. Takakuwa KM, Burek GA, Estepa AT, Shofer FS. A method for improving arrival-to-electrocardiogram time in emergency department chest pain patients and the effect on door-to-balloon time for ST-segment elevation myocardial infarction. Acad Emerg Med. 2009; 16:921–927.

32. Shiomi H, Nakagawa Y, Morimoto T, Furukawa Y, Nakano A, Shirai S, et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012; 344:e3257.

33. Heitzler VN, Babić Z, Milicić D, Starcević B, Mirat J, Strozzi M, et al. Evaluation of importance of door-to-balloon time and total ischemic time in acute myocardial infarction with ST-elevation treated with primary percutaneous coronary intervention. Acta Clin Croat. 2012; 51:387–395.
34. Towae F, Juenger C, Mudra H, Glunz HG, Hauptmann E, Grube E, et al. The development of door-to-angiography time in the last 14 years for patients with acute ST-elevation myocardial infarction treated with primary coronary intervention: Determinants and outcome. Results from the MITRAplus and OPTAMI registry. Acute Card Care. 2011; 13:35–39.

35. Song YB, Hahn JY, Gwon HC, Kim JH, Lee SH, Jeong MH, et al. The impact of initial treatment delay using primary angioplasty on mortality among patients with acute myocardial infarction: from the Korea acute myocardial infarction registry. J Korean Med Sci. 2008; 23:357–364.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download