Abstract
Purpose
To evaluate the kinetics of serum testosterone (T) recovery following short-term androgen deprivation therapy (ADT), as the understanding thereof is essential for the proper management of prostate cancer (PCa), especially intermittent ADT.
Materials and Methods
This prospective analysis included male sex offenders who voluntarily received leuprolide acetate in order to alleviate sexual aberrance. Thirty-three and 25 patients who received 3 and 6 months of ADT were assigned to Group A and Group B, respectively. Serum T levels were obtained every week during the on-cycle period, then monthly during the off-cycle period for at least 12 months.
Results
The kinetics of serum T during the on-cycle period were similar in both groups. After flare reaction at week 2, a nadir of 0.45±0.29 ng/mL was achieved. In Group A, an abrupt rebound-upsurge was observed during the first 2 month off-cycle period, which surpassed the baseline level and reached a plateau level of 8.74±2.11 ng/mL during the flare (p<0.001). This upsurge was followed by a gradual decline back to baseline over the following 10 months. In Group B, a gradual increase was observed, and a baseline level of 7.26±1.73 ng/mL was reached at 5 months. Thereafter, an ongoing upsurge that surpassed baseline levels was observed until 12 months (8.81±1.92 ng/mL; p=0.002).
Androgen-deprivation therapy (ADT) is the mainstay of initial treatment of androgen-sensitive, metastatic, or advanced stage prostate cancer (PCa).1 However, long-term ADT is associated with adverse effects such as hot flashes, decreased libido, loss of bone mineral density, depressive mood, and cognitive dysfunction, most of which are the results of deficient serum testosterone (T).2 To alleviate these unwanted effects for patients who are unable to accept such potential risks, intermittent ADT (IADT) is an alternative. A number of randomized clinical trials have observed IADT to reduce side effects and costs, with comparable oncological outcomes to ADT.3 Although its long-term efficacy remains undetermined, the current National Comprehensive Cancer Network guidelines suggest IADT to confer better patient tolerability without altering overall survival, compared to continuous ADT.4
Understanding the kinetics of serum T during the IADT off-cycle period is essential when deciding upon the timing and the duration of on- and off-cycles. Studies of the trends of serum T normalization during the off-cycle have reported highly variable results according to ADT duration, patient age, baseline serum T levels, or previous treatments for PCa [e.g. radical prostatectomy or external beam radiation therapy (EBRT)].1,5,6,7 However, surveys have demonstrated that only a minority of clinicians regularly monitor serum T, and instead base the decision to resume therapy following the off-cycle of prostate-specific antigen (PSA) levels.8 Certainly, understanding the kinetics of serum T recovery according to ADT duration is essential, as PSA is a tissue-specific protein that is strongly androgen dependent and the growth of PCa cells and progression to metastatic disease is dependent on serum T.9 Moreover, serum T above castrated levels following ADT is a reflection of insufficient suppression of androgens, and thus, could serve as an indicator for resuming therapy.10
A broad range of indications for ADT other than PCa includes precocious puberty, ovarian hyperandrogenism, and aberrant sexual behavior. We have previously reported treatment outcomes in a group of sex offenders who received ADT in an attempt to alleviate excessive sexual drive.11 Herein, implications for ADT schedule in regard to the observed patterns of serum T recovery will be newly discussed from a perspective of PCa. To the best of our knowledge, our observation was the first to investigate the kinetics of serum T recovery on a monthly basis following short-term ADT in a treatment-naïve, non-cancerous cohort.
This prospective analysis included sex offenders incarcerated in the National Forensic Hospital who received chemical castration from 2011 to 2013. After a detailed explanation of the therapeutic effects and possible risks, 58 patients volunteered to receive ADT in an attempt to self-alleviate excessive sexual aberrancy. Participation was completely voluntary and not a condition of parole or probation. Written informed consent was obtained from all patients with approval by the institutional ethics committee (1-219577-ABN-01-201306-HR-008).
Laboratory tests, namely complete blood cell count, serum chemistry, PSA, and sex hormones, including T, luteinizing hormone (LH), and follicle-stimulating hormone (FSH), for all patients were within accepted normal ranges (T: 2.65-8.0 ng/mL, LH: 1.8-8.6 mIU/L, and FSH: 1.5-12.4 mIU/mL). Serum T, LH, and FSH were measured using a microparticle enzyme immunoassay (Abbott® laboratories, Chicago, IL, USA). All patients were ADT-naïve without contraindications to receiving ADT, such as, allergy against the drug, osteoporosis, history of thromboembolism, liver failure, or pituitary pathology.12 A one-month formulation of leuprolide acetate (LA) 3.75 mg was injected subcutaneously every month. Thirty three and 25 patients chose to discontinue ADT after 3 and 6 months, and were allocated as Group A and Group B, respectively. With all test results blinded, the decision for ADT cessation was based on the severity of adverse effects or done at the patient's insistence on discontinuation. Measurements of mid-morning serum T, LH, and FSH were obtained every week during the on-cycle period, then monthly during the observational off-cycle period of at least 12 months. The castrate level of serum T was defined as less than 0.7 ng/mL.13
Statistical analysis was performed using SPSS software, version 18, for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to analyze the frequency of events; the Mann-Whitney U test was used to compare differences between groups; and the χ2-test was used for the analysis of two or more variables. Mean values and standard deviations for serum T, LH, and FSH were calculated.
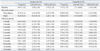
The demographic characteristics of Group A and Group B are shown in Table 1. The mean age of both groups was 35.7 years (range 21-56). The kinetics of serum T during the on-cycle period were similar in both groups, achieving a mean nadir of 0.45±0.29 ng/mL from the baseline level of 5.28±1.43 ng/mL. Flares were observed at 2 weeks, with serum T levels reaching up to 9.71±2.34 ng/mL. Trends in serum T values for each group are presented in Table 2.
Distinct patterns of serum T recovery between the two groups were noted during the off-cycle period. In Group A, an abrupt rebound-upsurge was observed during the first 2 months. This rebound surpassed the baseline level of 4.97±1.21 ng/mL, and almost reached a plateau level of 8.74±2.11 ng/mL, which was observed during the flare (p<0.001). A subsequent gradual decrease was observed over 10 months before serum T reached its baseline levels (Table 2, Fig. 1). In Group B, a slow gradual increase in serum T level was observed throughout the off-cycle period, and a baseline level of 7.26±1.73 ng/mL was achieved at 5 months. The rebound-surge phenomenon seen in Group A was not evident in Group B. However, following normalization at 5 months, an ongoing upsurge was observed until the last off-cycle follow-up at 12 months (8.81±1.92 ng/mL), which significantly surpassed the mean baseline level (p=0.002) (Table 2, Fig. 2). Trends in serum T recovery corresponded to alteration of serum LH levels in all groups.
IADT is an accepted option among multidisciplinary treatments for metastatic or advanced stage PCa, offering a few potential advantages, such as improved sexual function, decreased risk of ADT-related adverse events, and reduced medical cost.14 There is accumulating evidence that preserving the hormone-dependent state of a tumor for an extended period may possibly alter progressive, metastatic disease into a chronic state that is amenable to long-term control.15 A key issue in IADT is that serum T levels should actually recover during the off-cycle in order to alleviate the adverse effects related to castrated levels of T, but at the same time, should not become high enough to stimulate the proliferation of existing PCa cells or exacerbate tumor flares.16 It is surprising that the majority of clinicians assess treatment response during IADT without monitoring serum T, considering that serum T above castrated levels is a reflection of insufficient suppression of androgens, and thus, could serve as an indicator for resuming ADT.
The kinetics of serum T recovery after cessation of ADT vary highly according to treatment settings.7,15 Studies on the recovery trends of serum T following 3 months of neoadjuvant ADT have reported that serum T remains at castrate levels for 3 months following ADT cessation and gradually achieves baseline levels at 7 months.7 However, a major confounder has been the inclusion of patients who received EBRT during the observational period, which may have decreased testicular production of T.16 Hall, et al.17 observed that castrate levels of serum T persist for up to 12 months after discontinuing ADT of more than 2 years duration. The limitation of their study was that the included patients were on ADT at the time of enrollment, and thus baseline serum T levels were unknown. In another study of long-term ADT of more than 4 years, 53% of subjects were reported to remain castrated after 2.5 years.14 Common limitations of previous publications included long intervals between serum T measurements in which time to normalization may have been overestimated, the inclusion of patients receiving concurrent treatment for PCa such as EBRT, and endpoints that focused on time to serum T normalization with no further follow-up thereafter. Our observation was the first to monitor long-term trends in serum T recovery after 3 and 6 months of short-term ADT on a monthly basis, and discerned that at least a 6-month on-cycle period is required for stable normalization of serum T in IADT.
The biology of serum T recovery following administration of LA is unknown. LA initially stimulates gonadotropin-releasing hormone (GnRH) receptors in the pituitary gland, the so-called the 'flare phenomenon', but eventually causes desensitization and downregulation of GnRH receptors, resulting in decreased secretion of LH and FSH. This decreased LH secretion, in addition to downregulation of LH receptors in the testis, leads to decreased stimulation of the Leydig cells of the testes, resulting in reduced synthesis of serum T.18 The most noteworthy finding of our series was the rebound of serum T during the first 2 months of the off-cycle in patients who had received 3 months of ADT. One possible explanation for the fluctuations in serum T that paralleled LH levels is that the rebound is provoked from within the hypothalamic axis. One can also assume that a 3-month on-cycle period was insufficient to fully desensitize and down-regulate GnRH receptors, of which the drug washout may have caused a paradoxical overstimulation or an up-regulation of GnRH receptors. This hypothesis is in agreement with the observations of Bruchovsky, et al.,15 in which the ability of the testis to recover serum T declined according to repeated cycles of ADT. Regardless of its etiology, this preliminary observation has important implications regarding the risk of disease exacerbation after 3 months on-cycle (e.g. the proliferation of existing tumor cells or tumor flare). A 6-month on-cycle period of ADT in our series showed a relatively gradual increase in serum T until reaching a baseline level at 5 months. This data is in accordance with a previous study that showed that a median of 16.6 weeks was needed for serum T normalization after 6 months of treatment with GnRH agonists.19 However, our study extended the observational period to 12 months, and a persistent upsurge in serum T that significantly surpassed the baseline level was recorded. This is of clinical importance because it reveals the potential for the long-term stimulation and growth of PCa cells during a time when many clinicians do not monitor regular serum T measurements, since normalization has already been confirmed.
There are several limitations to our study. First is the relatively young age of the cohort, which may not represent elderly populations that typically receive ADT. Patients aged 70 or older are reported to have a greater likelihood of remaining castrated after ADT than younger patients due to decreased T production, at least in part because of senile testicular atrophy.13 In our series, the trend in serum T recovery in patients aged ≥50 years conformed to that of the younger cohort, implying that differences in age may unlikely influence the results. Nevertheless, consistent findings from an elderly population should be confirmed by additional studies before application to everyday clinical practice. The second limitation is the hypothetical justification of the observed kinetics necessitated by the absence of pharmacological studies documenting serum T recovery after the administration of GnRH agonists. Finally, there is a paucity of evidence relating excessively high levels of serum T to cancer progression. However, the results of the Prostate Cancer Prevention Trial and the REDUCE study indicate that reductions in potent androgens by 5α-reductase inhibitors decrease the relative risk of PCa and indirectly link excessive serum T and PCa oncogenesis.20,21 Additional studies are needed to determine whether the current observation will have clinical significance in the management of PCa patients on IADT.
The kinetics of serum T recovery during the IADT off-cycle varies according to the treatment duration. Precautions should be taken when performing short-term ADT, because an excessive serum T surge during the off-cycle may improve QoL, but hamper treatment efficacy. If confirmed, these preliminary data will have important implications for patient management and future clinical studies, including the discontinuation of GnRH agonists in the setting of neoadjuvant and adjuvant therapy, and especially in IADT.
Figures and Tables
 | Fig. 1Trends of mean serum testosterone (ng/mL), luteinizing hormone (mIU/mL), and follicle-stimulating hormone (mIU/mL) recoveries during on- and off-cycle periods of 3-month androgen deprivation therapy with leuprolide acetate. LH, luteinizing hormone; FSH, follicle-stimulating hormone; ADT, androgen deprivation therapy. |
 | Fig. 2Trends of mean serum testosterone (ng/mL), luteinizing hormone (mIU/mL), and follicle-stimulating hormone (mIU/mL) recoveries during on- and off-cycle periods of 6-month androgen deprivation therapy with leuprolide acetate. LH, luteinizing hormone; FSH, follicle-stimulating hormone; ADT, androgen deprivation therapy. |
Table 1
Demographic Characteristics of Patients Who Had Received 3 Months (Group A) and 6 Months (Group B) of ADT

References
1. Gulley JL, Aragon-Ching JB, Steinberg SM, Hussain MH, Sartor O, Higano CS, et al. Kinetics of serum androgen normalization and factors associated with testosterone reserve after limited androgen deprivation therapy for nonmetastatic prostate cancer. J Urol. 2008; 180:1432–1437.

2. Walsh PC, DeWeese TL, Eisenberger MA. A structured debate: immediate versus deferred androgen suppression in prostate cancer-evidence for deferred treatment. J Urol. 2001; 166:508–515.

3. Sciarra A, Abrahamsson PA, Brausi M, Galsky M, Mottet N, Sartor O, et al. Intermittent androgen-deprivation therapy in prostate cancer: a critical review focused on phase 3 trials. Eur Urol. 2013; 64:722–730.

4. NCCN clinical practice guidelines in oncology (NCCN Guideline® on prostate cancer. NCCN web site 2013. Available at: http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
5. Spry NA, Galvão DA, Davies R, La Bianca S, Joseph D, Davidson A, et al. Long-term effects of intermittent androgen suppression on testosterone recovery and bone mineral density: results of a 33-month observational study. BJU Int. 2009; 104:806–812.

6. Oefelein MG. Time to normalization of serum testosterone after 3-month luteinizing hormone-releasing hormone agonist administered in the neoadjuvant setting: implications for dosing schedule and neoadjuvant study consideration. J Urol. 1998; 160:1685–1688.

7. Nejat RJ, Rashid HH, Bagiella E, Katz AE, Benson MC. A prospective analysis of time to normalization of serum testosterone after withdrawal of androgen deprivation therapy. J Urol. 2000; 164:1891–1894.

8. Teillac P, Bono AV, Irani J, Wirth MP, Zlotta AR. The role of luteinizing hormone-releasing hormone therapy in locally advanced prostate cancer and biochemical failure: considerations for optimal use. Clin Ther. 2005; 27:273–285.

9. Knudsen KE, Penning TM. Partners in crime: deregulation of AR activity and androgen synthesis in prostate cancer. Trends Endocrinol Metab. 2010; 21:315–324.

10. Pathak AS, Pacificar JS, Shapiro CE, Williams SG. Determining dosing intervals for luteinizing hormone releasing hormone agonists based on serum testosterone levels: a prospective study. J Urol. 2007; 177:2132–2135.

11. Koo KC, Ahn JH, Hong SJ, Lee JW, Chung BH. Effects of Chemical Castration on Sex Offenders in Relation to the Kinetics of Serum Testosterone Recovery: Implications for Dosing Schedule. J Sex Med. 2014; [Epub ahead of print].

12. Hill A, Briken P, Kraus C, Strohm K, Berner W. Differential pharmacological treatment of paraphilias and sex offenders. Int J Offender Ther Comp Criminol. 2003; 47:407–421.

13. Oefelein MG, Feng A, Scolieri MJ, Ricchiutti D, Resnick MI. Reassessment of the definition of castrate levels of testosterone: implications for clinical decision making. Urology. 2000; 56:1021–1024.

14. Tsai HT, Penson DF, Makambi KH, Lynch JH, Van Den Eeden SK, Potosky AL. Efficacy of intermittent androgen deprivation therapy vs conventional continuous androgen deprivation therapy for advanced prostate cancer: a meta-analysis. Urology. 2013; 82:327–333.

15. Bruchovsky N, Klotz L, Crook J, Goldenberg SL. Locally advanced prostate cancer--biochemical results from a prospective phase II study of intermittent androgen suppression for men with evidence of prostate-specific antigen recurrence after radiotherapy. Cancer. 2007; 109:858–867.

16. Pickles T, Agranovich A, Berthelet E, Duncan GG, Keyes M, Kwan W, et al. Testosterone recovery following prolonged adjuvant androgen ablation for prostate carcinoma. Cancer. 2002; 94:362–367.

17. Hall MC, Fritzsch RJ, Sagalowsky AI, Ahrens A, Petty B, Roehrborn CG. Prospective determination of the hormonal response after cessation of luteinizing hormone-releasing hormone agonist treatment in patients with prostate cancer. Urology. 1999; 53:898–902.

18. Sethi R, Sanfilippo N. Six-month depot formulation of leuprorelin acetate in the treatment of prostate cancer. Clin Interv Aging. 2009; 4:259–267.
19. Gulley JL, Figg WD, Steinberg SM, Carter J, Sartor O, Higano CS, et al. A prospective analysis of the time to normalization of serum androgens following 6 months of androgen deprivation therapy in patients on a randomized phase III clinical trial using limited hormonal therapy. J Urol. 2005; 173:1567–1571.

20. Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003; 349:215–224.

21. Roehrborn CG, Nickel JC, Andriole GL, Gagnier RP, Black L, Wilson TH, et al. Dutasteride improves outcomes of benign prostatic hyperplasia when evaluated for prostate cancer risk reduction: secondary analysis of the REduction by DUtasteride of prostate Cancer Events (REDUCE) trial. Urology. 2011; 78:641–646.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download