Abstract
Purpose
Estimation of body fluid volume in hyponatremia is useful for diagnosis and therapeutic decision-making. Physical examination has been generally used to estimate body fluid volume, but it depends on the physician's abilities. Bioimpedance spectroscopy has been suggested to be a reliable method for the estimation of body fluid volume. Therefore, this study investigated whether bioimpedance spectroscopy could replace physical examination in hyponatremia.
Materials and Methods
The study included 30 patients with hyponatremia. At the time of the initial visit, body fluid volume was estimated simultaneously by both physical examination and bioimpedance spectroscopy. Estimation of body fluid status by clinical diagnosis was performed as well, which determined body fluid status corresponds with the most likely cause of hyponatremia (clinical body fluid estimation).
Results
The results of body fluid volume estimated by physical examination, bioimpedance spectroscopy, and clinical body fluid estimation showed that 9, 10, and 9 patients, respectively, were hypervolemic; 13, 15 and 16 patients, respectively, were euvolemic; and 8, 5, and 5 patients, respectively, were hypovolemic. Cohen's kappa analysis showed a significant agreement between physical examination and bioimpedance spectroscopy (kappa coefficient, 0.632, p<0.001). In addition, bioimpedance spectroscopy showed a higher level of agreement with clinical body fluid estimation than physical examination (kappa coefficient, 0.602 vs. 0.524).
Conclusion
This study suggests that bioimpedance spectroscopy could replace physical examination for estimating body fluid status in hyponatremia. In addition, bioimpedance spectroscopy might correspond better with clinical diagnosis than physical examination in the estimation of body fluid status in hyponatremia.
Hyponatremia is the most common electrolyte imbalance. Since the etiology of this disease is diverse and complex, the clinical diagnosis of hyponatremia is not clear in many cases. In such cases, the estimation of body fluid status may be useful to diagnose the exact cause of hyponatremia. In addition, it may be important to determine the best method for treatment of hyponatremia, since therapy aims to normalize body fluid status as well as correct the level of sodium.1 Physical examination has been generally used to estimate body fluid status, but it depends on the physician's abilities. Bioimpedance spectroscopy (BIS) has been suggested to be a reliable method for the estimation of body fluid volume.2 Therefore, this study aimed to investigate whether BIS could replace physical examination in patients with hyponatremia.3
This study included 30 patients with hyponatremia. Patients whose weight and height could not be measured were excluded. At the time of the initial visit, medical and drug-use history related to hyponatremia were collected, and laboratory data including hormone levels, such as thyroid, cortisol and ACTH, rennin, and aldosterone, were measured. Body fluid status was estimated simultaneously by both physical examination and BIS. In addition, estimation of body fluid status by clinical diagnosis was performed as well.
Body fluid status by physical examination was determined by gross edema (edema or non-edema), pretibial pitting edema (pitting or non-pitting), and skin turgor (intact or decreased). If a patient had either gross or pretibial pitting edema, the patient was diagnosed as hypervolemic. If a patient had neither gross nor pretibial pitting edema but had intact skin turgor, the patient was diagnosed as euvolemic. If a patient had neither gross nor pretibial pitting edema but had decreased skin turgor, the patient was diagnosed as hypovolemic. In addition, body fluid status by BIS was estimated using the Body Composition Monitor (BCM, Fresenius Medical Care, Germany). The BCM showed excessive body fluid volume with a value indicating overhydration (OH, liter). Positive OH value denotes excess, and negative OH value denotes insufficiency. Considering the reference range of the BCM measurement, OH >1 was diagnosed as hypervolemia, OH <-1 was diagnosed as hypovolemia, and -1≤OH≤1 was diagnosed as euvolemia. Lastly, body fluid status was also estimated by clinical diagnosis, which determined body fluid status corresponds with the most likely cause of hyponatremia (clinical body fluid estimation). The cause of hyponatremia and corresponding body fluid status are presented in Table 1.
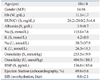
The baseline and clinical characteristics are shown in Table 2 and 3. The mean age of subjects was 68±14 years. Among the patients, there were 14 males and 16 females. The mean concentration of serum sodium was 115.0±7.6 mmol/L, and urine sodium was 50.7±37.9 mmol/L. Serum osmolality was 255.5±19.9 mmol/kg, and urine osmolality was 404.9±188.5 mmol/kg. Mean overhydration by BIS was 0.8±2.1 liters. There were 6 cases of recurrent hyponatremia. The mental statuses of the subjects were as follows: 'alert' 26 patients, 'confused' 3 patients, and 'drowsy' 1 patient. The dietary statuses of the subjects were as follows: 'well' 3 patients, 'normal' 6 patients, and 'poor' 21 patients. Among the subjects, hyponatremia was related to thiazide in 13 patients, psychiatric medication in 6 patients, and other drugs in 22 patients. Five patients were diagnosed with hypothyroidism, 1 patient with hyperthyroidism, and 8 patients with sick euthyroid syndrome. Three patients had adrenal insufficiency. Body fluid status estimated by BIS showed that 10 patients were hypervolemic, 15 patients were euvolemic, and 5 patients were hypovolemic.
Clinical diagnosis for the cause of hyponatremia in each patient is shown in Table 4. The clinical diagnosis indicated the most likely cause of hyponatremia. A few cases had mixed causes.
The results of body fluid status estimated by each method are shown in Table 5. The results by physical examination showed that 9 patients were hypervolemic, 13 patients were euvolemic, and 8 patients were hypovolemic. The results by BIS showed that 10 patients were hypervolemic, 15 patients were euvolemic, and 5 patients were hypovolemic. The results of clinical body fluid estimation showed that 9 patients were hypervolemic, 16 patients were euvolemic, and 5 patients were hypovolemic.
Cohen's kappa analysis showed a significant agreement between physical examination and BIS (kappa coefficient 0.632, p<0.001).
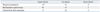
Both physical examination and BIS showed a significant agreement with clinical body fluid estimation. Cohen's kappa coefficient was 0.524 between physical examination and clinical body fluid estimation (p<0.001), and the kappa coefficient was 0.602 between BIS and clinical body fluid estimation (p<0.001). When the two kappa coefficients were compared, the kappa coefficient between BIS and clinical body fluid estimation was higher than that between physical examination and clinical body fluid estimation (Table 6).
In hyponatremia with an uncertain cause, estimating body fluid status could be useful to diagnose the main cause. In addition, the estimation of body fluid status is important to determine the best treatment method for hyponatremia, since therapy for hyponatremia aims at not only achieving an optimal concentration of sodium, but also optimal body fluid status.1 In general, body fluid status is determined by physical examination. However, physical examination is unable to provide an accurate estimate of body fluid status because the estimation depends on the physician's abilities. In contrast, BIS can more objectively estimate body fluid volume. Many studies have investigated the reliability and clinical applications of BIS4-6 and have shown mixed results, especially in regard to measurements of total body fluid and extracellular fluid volumes.7-11 In recent years, however, BIS has improved with the development of suitable models and equations. Therefore, BIS is currently considered a reliable method for estimating body fluid volume.2,12 Moreover, BIS could be an acceptable method for rough estimation of body fluid status such as hypervolemia, euvolemia and hypovolemia.
Our results showed that the estimation of body fluid status by physical examination or BIS agreed significantly. Therefore, we suggest that BIS could replace physical examination for estimating body fluid status in hyponatremia. In addition, we found that the kappa coefficient between BIS and clinical body fluid estimation was higher than that between physical examination and clinical body fluid estimation. Therefore, it is believed that BIS corresponds well with clinical diagnosis compared with physical examination in hyponatremia.
This study has a limitation in that we did not measure body fluid volume using the isotope dilution method. Nonetheless, we believe that this study is still informative because BIS has been validated by many studies for estimating body fluid volume. Also, the aim of this study was to determine the practicality of using BIS for estimating body fluid volume in hyponatremic patients. This is the first report of BIS application for estimating body fluid volume in hyponatremia.
In conclusion, this study suggests that BIS can replace physical examination for estimating body fluid status in hyponatremia. In addition, BIS corresponds well with clinical diagnosis compared with physical examination. It is believed that BIS is an objective and useful method for estimating body fluid status in hyponatremia.
Figures and Tables
Table 1
Clinical Body Fluid Estimation, the Cause of Hyponatremia and Corresponding Body Fluid Status

References
1. Lindner G, Schwarz C. An update on the current management of hyponatremia. Minerva Med. 2012; 103:279–291.
2. López-Gómez JM. Evolution and applications of bioimpedance in managing chronic kidney disease. Nefrologia. 2011; 31:630–634.
3. Bunnag S, Pattanasombatsakul K. N-terminal-pro-brain natriuretic peptide for the differential diagnosis of hypovolemia vs. euvolemia in hyponatremic patients. J Med Assoc Thai. 2012; 95:Suppl 3. S69–S74.
4. Kyle UG, Bosaeus I, De Lorenzo AD, Deurenberg P, Elia M, Manuel Gómez J, et al. Bioelectrical impedance analysis-part II: utilization in clinical practice. Clin Nutr. 2004; 23:1430–1453.

5. Aspromonte N, Cruz DN, Ronco C, Valle R. Role of bioimpedance vectorial analysis in cardio-renal syndromes. Semin Nephrol. 2012; 32:93–99.

6. Machek P, Jirka T, Moissl U, Chamney P, Wabel P. Guided optimization of fluid status in haemodialysis patients. Nephrol Dial Transplant. 2010; 25:538–544.

7. Cox-Reijven PL, Kooman JP, Soeters PB, van der Sande FM, Leunissen KM. Role of bioimpedance spectroscopy in assessment of body water compartments in hemodialysis patients. Am J Kidney Dis. 2001; 38:832–838.

8. Wizemann V, Rode C, Wabel P. Whole-body spectroscopy (BCM) in the assessment of normovolemia in hemodialysis patients. Contrib Nephrol. 2008; 161:115–118.

9. Wabel P, Chamney P, Moissl U, Jirka T. Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif. 2009; 27:75–80.

10. van den Ham EC, Kooman JP, Christiaans MH, Nieman FH, Van Kreel BK, Heidendal GA, et al. Body composition in renal transplant patients: bioimpedance analysis compared to isotope dilution, dual energy X-ray absorptiometry, and anthropometry. J Am Soc Nephrol. 1999; 10:1067–1079.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download