Abstract
Purpose
The association between autoimmune thyroid diseases (AITDs) and vitamin D deficiency is controversial. We aimed to evaluate the relationship between serum 25-hydroxy-vitamin D3 [25(OH)D3] and anti-thyroid antibody levels.
Materials and Methods
25(OH)D3, anti-thyroid antibodies, and thyroid function measured in 304 patients who visited the endocrinology clinic were analyzed. The patients were subgrouped into the AITDs or non-AITDs category according to the presence or absence of anti-thyroid antibodies. The relationship between anti-thyroid peroxidase antibody (TPOAb) and 25(OH)D3 was evaluated.
Results
The patients with elevated anti-thyroid antibodies had lower levels of serum 25(OH)D3 than those who did not (12.6±5.5 ng/mL vs. 14.5±7.3 ng/mL, respectively, p<0.001). Importantly, after adjusting for age, sex, and body mass index, a negative correlation (r=-0.252, p<0.001) was recognized between 25(OH)D3 and TPOAb levels in the AITDs group, but this correlation did not exist in the non-AITDs group (r=0.117, p=0.127). 25(OH)D3 level was confirmed as an independent factor after adjusting for co-factors that may affect the presence of TPOAb in the AITDs group.
The discovery of vitamin D receptor in most tissues and cells in the human body has provided new insights into the function of vitamin D as a unique hormone.1 Many studies have shown that vitamin D can play a role in decreasing the risk of chronic illnesses, including autoimmune, infectious, and cardiovascular diseases.2-7 Furthermore, the role of vitamin D as an immune-modulator has been reported in recent years, and low levels of vitamin D have been observed in several autoimmune diseases, including autoimmune thyroid diseases (AITDs).8-10 It has been estimated that more than 1 billion people worldwide have vitamin D deficiency {serum 25-hydroxy-vitamin D3 [25(OH)D3] below 20 ng/mL} or insufficiency [25(OH)D3 of 21-29 ng/mL]. Elderly people as well as children and young adults are potentially at high risk for vitamin D deficiency.1,11-14 Furthermore, in South Korea, it is now a greater threat to the younger generation, especially to those in the age of 20-29 and in young adults.15 Females have an especially higher prevalence of AITDs.16,17 Hence, we hypothesized that there may be an association between vitamin D levels and AITDs.
A few studies have examined the relationship between vitamin D insufficiency or deficiency and prevalence of AITDs in humans. However, whether a definite association between these two conditions exists is still controversial. One recent study showed that the prevalence of vitamin D deficiency is higher in patients with AITDs and that the presence of anti-thyroid antibodies is significantly more common in patients with vitamin D deficiency than in those with higher vitamin D levels.8 In contrast, another study performed in India revealed a weak association between low vitamin D levels and AITDs. To elucidate the correlation between vitamin D and AITDs, we analyzed vitamin D levels in thyroid disease patients and evaluated the relationship between anti-thyroid peroxidase antibody (TPOAb) and serum vitamin D levels.
The medical records of Korean patients who visited the endocrinology out-patient clinic of Severance Hospital from March 2010 to June 2011 were reviewed. All patients underwent a thyroid function test and ultrasonography initially for the purpose of thyroid evaluation. Serum anti-thyroid antibodies including TPOAb and thyroid stimulating hormone (TSH) receptor antibody (TSHRAb) representing Hashimoto's thyroiditis and Graves' disease respectively, and 25(OH)D3 were additionally measured in these patients at the first visit. The patients taking anti-thyroid drugs or under thyroid hormone replacement therapy were excluded. Among these patients, 304 were enrolled and subgrouped into either the AITDs or the non-AITDs category according to the presence or absence of anti-thyroid antibodies, regardless of thyroid functional status. This retrospective study was approved by our Institutional Review Board, and informed consent was not required.
Serum TSH, free T4, and T3 were measured by chemiluminescent microparticle immunoassay (Architect System, Abbott Ireland Diagnostic Division, Lisnamuck, Longford, Co. Longford, Ireland). Serum levels of TSHRAb (normal range: 0-1.75 IU/L), and TPOAb (threshold value: 0-13.7 IU/mL) were measured by an electro-chemiluminescence immunoassay according to standard protocols (COBAS, Roche Diagnostics GmbH, Mannheim, Germany).
Serum 25(OH)D3 levels were measured by a radioimmunoassay kit (DiaSorin, Inc., Stillwater, MN, USA; normal range: 9.3-37.6 ng/mL). Quantitative determination of 25(OH)D3 was carried out by a direct, competitive chemiluminescence immunoassay. Specifically, magnetic particles (solid phase) were coated with a specific antibody to vitamin D, and vitamin D was linked to an isoluminol derivative. During the incubation, 25(OH)D3 was dissociated from its binding protein and competed with labeled vitamin D for binding sites on the antibody. After the incubation, the unbound material was removed with a wash cycle, the starter reagents were added, and a flash chemiluminescent reaction was initiated. The light signal was measured by an photomultiplier as relative light units and was inversely proportional to the concentration of 25(OH)D3 present in calibrators, controls, or samples.
Ultrasonographic evaluation of the thyroid gland was performed with an HDI 3000 or HDI 5000 system (Philips Medical Systems, Bothell, WA, USA) or an Acuson Sequoia 512 system (Siemens Medical Solutions, Mountain View, CA, USA). Three well-trained radiologists performed a real-time sonographic exam and interpreted the results. Ultrasonographic features of diffuse thyroiditis were defined using the generally accepted standards of diffuse parenchymal hypoechogenicity or a heterogeneous echogenic pattern of thyroid gland.
Comparison of categorical variables between groups was performed using chi-square test and Fisher's exact test (two-tailed), as appropriate. Continuous variables are expressed as mean±standard deviation. The Student's t-test and Mann-Whitney U test was used for comparison of mean values between groups. Statistical comparisons between groups were performed using the chi-square test. Spearman correlations were used to examine relationships between the log-transformed TPOAb titer and age, body mass index (BMI), 25(OH)D3 and other biochemical variables. Correlations were reported as age- and BMI-adjusted. To examine the differences in 25(OH)D3 and other biochemical parameters between patients with or without TPOAb, a regression model fit the presence of TPOAb as the dependent variable and 25(OH)D3 as the independent variable. p-values <0.05 were considered statistically significant for all tests. All analyses were performed using IBM SPSS software ver. 18.0 (SPSS Inc., IBM company, New York, NY, USA).
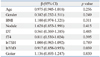
Baseline characteristics of AITDs and non-AITDs patients were compared in Table 1. Among 304 patients, 111 patients were diagnosed as AITDs (65 patients with Hashimoto's thyroiditis, 46 patients with Graves' disease). The mean of age, gender, serum calcium and phosphorus level, and thyroid function test results [except serum triiodothyronine (T3) level] were not significantly different between the two groups. However, the prevalence of hyperthyroidism and hypothyroidism, and mean serum 25(OH)D3 level in the patients with AITDs was significantly lower than in patients with non-AITDs (56.8% vs. 16.1%, 11.9% vs. 16.2%, 12.6±5.5 ng/mL vs. 14.5±7.3 ng/mL, respectively, p<0.001). TPOAb and TSHRAb were also significantly higher in the AITDs group than in the non-AITDs group (298.5±336.7 IU/mL vs. 6.4±2.6 IU/mL, p<0.001 and 5.11±7.97 IU/L vs. 1.40±3.45 IU/L, p<0.001, respectively).
Table 2 shows the correlation between anti-thyroid antibodies and 25(OH)D3. In the AITDs group, the TPOAb level was inversely correlated with 25(OH)D3 (r=-0.252, p<0.001) but not in the non-AITDs group (r=0.117, p=0.127). TSHRAb was not correlateed with 25(OH)D3 levels in either group.
In the multiple regression analysis, only 25(OH)D3 level was a major determinant of the presence of TPOAb (odds ratio: 0.917, 95% confidence interval: 0.858-0.953, p=0.039) after adjusting for age, gender, BMI, presence of nodule, goiter, and diffuse thyroiditis, which were detected on thyroid ulrelattrasonography and thyroid function test (Table 3).
According to the nationally representative study recently performed in Korea, the mean serum vitamin D level in the Korean female population was determined to be 18.2 mg/dL, and the prevalence of vitamin D insufficiency was 64.5%.15 This prevalence is remarkably high compared to that of the male population. AITDs are the most common endocrine disease as well as the most common autoimmune diseases. They have been reported to be prevalent in 1-2% of all males and 7-9% of all females.17 The fact that both vitamin D deficiency and AITDs are predominantly found in women signifies a certain association between these two conditions. For example, one recent study reported a link between vitamin D deficiency and the presence of anti-thyroid antibodies.8 In addition, our study demonstrated a negative association between 25(OH)D3 and TPOAb levels, and have also shown that the low 25(OH)D3 level is a possible risk factor of TPOAb positivity.
The pathophysiology of AITDs is diverse and includes genetic and environmental factors, as well as hormonal influences.18 The relationship between inflammatory cytokines and AITDs is especially well accepted, and the occurrence of AITDs after administration of interferon-alpha has been reported and well known.19 Taking into consideration the regulatory effect of vitamin D on inflammatory responses and autoimmunity, such reports support the possible relationship between AITDs and vitamin D deficiency.20-22 Previous prevalence studies have argued that vitamin D deficiency is one of the features of AITDs, especially that of Hashimoto's thyroiditis.23 Our study not only supports the existing argument on the association between vitamin D and AITDs but also further solidifies the association by revealing that 25(OH)D3 has a statistical correlation with TPOAb titer in AITDs patients.
This study has not shown a difference in vitamin D level related to thyroid function or entity of the disease. This suggests that vitamin D deficiency is more closely related to anti-thyroid antibody titer rather than thyroid function itself in humans, and also agrees with the existing study on patients with Hashimoto's thyroiditis.23 We suggest that vitamin D functions as an immune modulator in autoimmune thyroiditis and that the molecular mechanism should be further investigated to clarify the causal relationship between vitamin D level and autoimmune thyroiditis. It is notable that a significant association between TPOAb and 25(OH)D3 level was only found in the AITDs group. This may be due to an overall low vitamin D level in the Korean population. In fact, the correlation between 25(OH)D3 level and TPOAb is also seen in vitamin D level within the range of vitamin D deficiency as defined by a recent guideline on bone metabolism, suggesting a need of a different reference value of vitamin D for this extra-skeletal effect.
This study did not show a seasonal change in vitamin D levels. Vitamin D levels were the lowest in the winter, as was expected, though the association was not statistically significant. This may have been because the majority of the patients were already in a state of vitamin D insufficiency. (Supplementary Table 1, only online)
Most effects of vitamin D are mediated via the vitamin D3 receptor (VDR).24 The immune modulator properties of vitamin D are ascribed to its effect on T and B lymphocytes, all of which harbor VDRs. Vitamin D has been shown to inhibit dendritic cell-dependent T-cell activation, and promote tolerogenic properties that favor the induction of regulatory rather than effector T cells.25 In addition, in vitro studies have shown that activation of CD4 T cells expressing VDR by vitamin D promotes a Th2 phenotype (with IL-4 and IL-5 production) while suppressing Th1 activity (with interferon-gamma and IL-2 production).26,27 Through such mechanisms, vitamin D is thought to modulate cell-mediated immune responses and regulate inflammatory T-cell activity.28 Low vitamin D may increase the degree of autoimmunity and subsequently increase the prevalence of AITDs, which are the most common autoimmune diseases. Furthermore, the recent surge in prevalence of AITDs may be related to vitamin D deficiency, whose prevalence is also rising.
However, this study does not prove a causal effect of vitamin D insufficiency in the pathogenesis of AITDs. There have been no results of interventional study proving the effect of vitamin D supplements on human subjects with AITDs; furthermore, some argue that vitamin D insufficiency more commonly found in AITDs is the result of the pathogenesis of AITDs and its subsequent effect, such as VDR dysfunction.9,29 Therefore, further studies on this subject are required.
The limitations of this study include the retrospective nature of the study and the pool of patients who visited our tertiary hospital from which our population was sampled. We did not measure anti-thyroglobulin antibody and thyroglobulin. Hence, we could not investigate the relationship between vitamin D and these parameters. Furthermore, clinical parameters associated with thyroid disease, such as cigarette smoking, were not available. Thus, we could not investigate the relationship between smoking and autoimmune disease and AITDs. However, such limitations might not impact on the relationship between TPOAb and vitamin D levels established in this study.
In conclusion, this study found a clear association between 25(OH)D3 and TPOAb levels in AITDs, and confirmed 25(OH)D3 to be an independent factor related with the presence of TPOAb. The causal effects of low vitamin D level on thyroid autoimmunity and whether vitamin D replacement is helpful to the patients with AITDs required future validation.
Figures and Tables
Table 1
Baseline Characteristics of the Patients According to the Presence of Autoimmune Thyroid Diseases

Table 2
Correlation between Anti-Thyroid Antibodies and 25(OH)D3 Levels (Adjusted for Age, Sex, and BMI)

ACKNOWLEDGEMENTS
This work was supported by a Yonsei University College of Medicine Faculty Research Grant 2010 (No. 6-2010-0137).
References
2. Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008; 117:503–511.

3. Zittermann A, Schleithoff SS, Koerfer R. Putting cardiovascular disease and vitamin D insufficiency into perspective. Br J Nutr. 2005; 94:483–492.

4. Kamen DL, Cooper GS, Bouali H, Shaftman SR, Hollis BW, Gilkeson GS. Vitamin D deficiency in systemic lupus erythematosus. Autoimmun Rev. 2006; 5:114–117.

5. Huisman AM, White KP, Algra A, Harth M, Vieth R, Jacobs JW, et al. Vitamin D levels in women with systemic lupus erythematosus and fibromyalgia. J Rheumatol. 2001; 28:2535–2539.
6. Shapira Y, Agmon-Levin N, Shoenfeld Y. Mycobacterium tuberculosis, autoimmunity, and vitamin D. Clin Rev Allergy Immunol. 2010; 38:169–177.

7. Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001; 358:1500–1503.

8. Kivity S, Agmon-Levin N, Zisappl M, Shapira Y, Nagy EV, Dankó K, et al. Vitamin D and autoimmune thyroid diseases. Cell Mol Immunol. 2011; 8:243–247.

9. Proal AD, Albert PJ, Marshall TG. Dysregulation of the vitamin D nuclear receptor may contribute to the higher prevalence of some autoimmune diseases in women. Ann N Y Acad Sci. 2009; 1173:252–259.

10. Goswami R, Marwaha RK, Gupta N, Tandon N, Sreenivas V, Tomar N, et al. Prevalence of vitamin D deficiency and its relationship with thyroid autoimmunity in Asian Indians: a community-based survey. Br J Nutr. 2009; 102:382–386.

11. Lips P, Hosking D, Lippuner K, Norquist JM, Wehren L, Maalouf G, et al. The prevalence of vitamin D inadequacy amongst women with osteoporosis: an international epidemiological investigation. J Intern Med. 2006; 260:245–254.

12. Holick MF. High prevalence of vitamin D inadequacy and implications for health. Mayo Clin Proc. 2006; 81:353–373.

13. Greene-Finestone LS, Berger C, de Groh M, Hanley DA, Hidiroglou N, Sarafin K, et al. 25-Hydroxyvitamin D in Canadian adults: biological, environmental, and behavioral correlates. Osteoporos Int. 2011; 22:1389–1399.

14. Gordon CM, Feldman HA, Sinclair L, Williams AL, Kleinman PK, Perez-Rossello J, et al. Prevalence of vitamin D deficiency among healthy infants and toddlers. Arch Pediatr Adolesc Med. 2008; 162:505–512.

15. Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, et al. Vitamin D insufficiency in Korea--a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab. 2011; 96:643–651.

16. McGrogan A, Seaman HE, Wright JW, de Vries CS. The incidence of autoimmune thyroid disease: a systematic review of the literature. Clin Endocrinol (Oxf). 2008; 69:687–696.

17. Canaris GJ, Manowitz NR, Mayor G, Ridgway EC. The Colorado thyroid disease prevalence study. Arch Intern Med. 2000; 160:526–534.

18. Volpe R. The pathophysiology of autoimmune thyroid disease. Endocr Regul. 1991; 25:187–192.
19. Prummel MF, Laurberg P. Interferon-alpha and autoimmune thyroid disease. Thyroid. 2003; 13:547–551.
20. Arnson Y, Amital H, Shoenfeld Y. Vitamin D and autoimmunity: new aetiological and therapeutic considerations. Ann Rheum Dis. 2007; 66:1137–1142.

21. van Etten E, Mathieu C. Immunoregulation by 1,25-dihydroxyvitamin D3: basic concepts. J Steroid Biochem Mol Biol. 2005; 97:93–101.

22. Cantorna MT. Vitamin D and its role in immunology: multiple sclerosis, and inflammatory bowel disease. Prog Biophys Mol Biol. 2006; 92:60–64.

23. Tamer G, Arik S, Tamer I, Coksert D. Relative vitamin D insufficiency in Hashimoto's thyroiditis. Thyroid. 2011; 21:891–896.

24. Haussler MR, Whitfield GK, Haussler CA, Hsieh JC, Thompson PD, Selznick SH, et al. The nuclear vitamin D receptor: biological and molecular regulatory properties revealed. J Bone Miner Res. 1998; 13:325–349.

25. van Halteren AG, Tysma OM, van Etten E, Mathieu C, Roep BO. 1alpha,25-dihydroxyvitamin D3 or analogue treated dendritic cells modulate human autoreactive T cells via the selective induction of apoptosis. J Autoimmun. 2004; 23:233–239.

26. Boonstra A, Barrat FJ, Crain C, Heath VL, Savelkoul HF, O'Garra A. 1alpha,25-Dihydroxyvitamin d3 has a direct effect on naive CD4(+) T cells to enhance the development of Th2 cells. J Immunol. 2001; 167:4974–4980.

27. van Halteren AG, van Etten E, de Jong EC, Bouillon R, Roep BO, Mathieu C. Redirection of human autoreactive T-cells Upon interaction with dendritic cells modulated by TX527, an analog of 1,25 dihydroxyvitamin D(3). Diabetes. 2002; 51:2119–2125.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download