Abstract
Purpose
The effects of an oral hygienic care program (OHCP) have been reported in several diseases. However, no study exists investigating the influence of an OHCP on stroke patients or patients in the intensive care unit (ICU) has been reported, thus we sought to investigate the potential effect of an OHCP.
Materials and Methods
Fifty-six consecutive stroke patients who were admitted to the ICU were randomly assigned to two groups: the intervention (29 patients) and control groups (27 patients). The OHCP included tooth brushing with an inter-dental brush and tongue cleaner and cleaning with chlorhexidine was administered to patients by one dentist once per day during admission in the ICU (mean, 2.2 weeks). The plague index, gingival index, clinical attachment loss, and colonization degree of candida albicans were assessed.
Results
After OHCP, the plaque index, gingival index, and colonization degree of candida albicans in saliva showed a significant decrease in the intervention group compared to those of the control group (p<0.05). However, no significant difference was observed in clinical attachment loss and the colonization degree of candida albicans on the tongue (p>0.05).
Stroke is a leading cause of adult disability. Stroke patients are known to be vulnerable to oral health problems, such as periodontal disease, due to a limitation in their activities of daily living.1 These problems can become worse when patients are admitted to the intensive care unit (ICU) for the following reasons. First, patients are admitted due to low consciousness and difficulty moving, which restrict self-care activities and can lead to deterioration of oral hygiene. Second, patients who cannot take food orally and have reduced secretion of saliva, which can cause dryness in the mouth.2 Third, frequent use of endotracheal and nasogastric tubes can also make the patient's mouth dry and hinder maintenance of oral hygiene.2-5 Fourth, management of oral hygiene tends to be overlooked because patients in the ICU can show unstable vital signs and medical staff in the ICU may not regard oral hygiene as having a direct impact on the patient's life.2,6
Oral health problems include candidiasis, ulcer of the mucous membrane, dental caries due to plaque, periodontitis, and gum inflammation and bleeding.7,8 Periodontitis could trigger systemic infection, such as pneumonia, and facilitate the ability of candida albicans (Candida) to bind with and penetrate the oral mucosa.9 When a patient's mouth is not kept clean, pathogens such as methicilline-resistant staphyloccus aureus or pseudomonas aeruginosa form a cluster inside the mouth that can increase the risk of ventilator-related pneumonia (VAP) and aspiration pneumonia.10,11 With the high fatality rate in the ICU, prevention of VAP is critical to patients' health and recovery.12,13 Therefore, oral hygiene management for patients in the ICU is necessary in order to reduce the risk of secondary hospital infection as well as to prevent oral health problems.
Several studies have reported on the usefulness of an oral hygienic care program (OHCP) in patients with diabetic mellitus,11 pneumonia,14 and cardiovascular disease15 as well as in the dependant elderly.16 However, there has been no study investigating use of an OHCP in stroke patients or patients in the ICU. Therefore, we attempted to investigate the effect of an OHCP on stroke patients during their stay in the ICU.
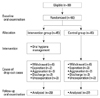
Ninty consecutive stroke patients who had been admitted to the ICU of the neurosurgery department of a university hospital were recruited according to the following inclusion criteria: 1) first-ever stroke, 2) had six or more teeth, and 3) no sign of infection with any contagious pathogen. Patients were assigned randomly to two groups (intervention or control) matched with sex and age by a nurse who managed the ICU and was independently involved in this research. Random number allocation was used to organize patients into either the intervention or control group. Once a patient was allocated into the intervention group, the next patient in the control group was matched by age and sex. Important confounding factors, such plague index and diabetic status, were compared between the two groups at baseline to check comparability before the intervention program started, and the characteristics between the two groups were regularly confirmed as patients dropped out of the program. Out of the 90 patients, 34 patients dropped out of this study within one week after the first oral examination. The reasons for dropping out included: expiration (n=5, 14.7%), aggravation of systemic condition due to systemic infection or recurrence of stroke (n=5, 14.7%), transfer to other hospitals or discharge home from the ICU (n=5, 14.7%), withdrawal of consent during the OHCP (n=14, 41.2%), behavior problems such as irritability (n=5, 14.7%). Finally, 56 stroke patients who were admitted to the ICU were enrolled in this study (Fig. 1). One family member of each patient provided written informed consent before enrollment, and the Institutional Review Board of our university hospital approved the study protocol.
Based on the medical records of the patients, history of smoking, drinking, diabetes, hypertension, and degree of consciousness at the time of admission to the ICU were evaluated. The Glasgow Coma Scale (GCS) was used to assess the degree of consciousness.17
Oral examination was performed twice for each patient after stabilization of vital signs following admission to the ICU, and before discharge from the ICU (mean, 2.2 weeks; range, 1-5 weeks). For the examination of oral hygiene status, one dentist and one hygienist evaluated patients using the decayed missing and filled teeth (DMFT) index, tooth mobility index, the Löe and Silness plaque index (PI) and gingival index (GI), clinical attachment loss (CAL), and the colonization degree of Candida under artificial lighting. Tooth mobility index was scored per tooth according to Lindhes Grading.18 The PI and GI were scored per six teeth, which included the four first-molars, right upper, and left lower central incisors.19,20 The CAL was measured to the nearest millimeter using a periodontal probe (PCP-UNC15 Color-Coded probe) at two sites (mid-buccal, mesio-buccal) in six teeth (four first-molars, right upper and left lower central incisors).21 Mean values were calculated individually. Nickerson's culture media was used for measurement of the colonization degree of Candida on the tongue and in saliva. Unstimulated whole saliva (minimum 20 µm) was collected. Colony count was used for measurement of Candida on the tongue and in saliva. Samples on the tongue were collected with a sterile swap and unstimulated whole saliva (range 20-40 µL) was collected with a disposable spoid. The collected sample was applied on the surface of Nikerson's culture agar plate. After cultivation in an incubator at 36.5℃ for 48 hours, colony counting was performed in order to divide the colony degree into four categories. The categories were 0, 1, 2, or 3 and 0, 103, 104, or >105 (unit: colony forming unit/mL) colonies, respectively.
In the intervention group, oral hygienic management was administered to patients by one dentist once every day for an average of 2.2 weeks (range, 1-5 weeks). For patients without consciousness, a mouth gag for dental care was used to keep the mouth open. A children's toothbrush and an interdental toothbrush were used for removal of plaque on the teeth, while a tongue cleaner was used to get rid of plaque on the tongue. Then, gauze soaked with 0.5% chlorohexidine was used to clean oral mucosa and tooth surfaces and to remove foreign bodies inside the mouth. When many inflammatory substances were found in the mouth, vacuum suction was performed to clean the mouth.
Clinico-demographic data, duration between first and second evaluation, and the parameters of oral health status were analyzed using t-test and χ2-test between the intervention and control groups. Paired-t test was performed in order to examine oral health status, including the PI, GI, and CAL. In addition, analysis of covariance was used to investigate difference between the intervention and control groups for each variable before and after the OHCP. Finally, the Friedmann test was performed for comparison of the prevalence of oral candidiasis between the intervention and control groups. All statistical analyses were implemented using SPSS (SPSS 20.0 for Windows, SPSS Inc., Chicago, IL, USA), and the statistical significance level was set at 0.05.
A summary of demographic and clinical data for each group of patients is shown in Table 1. Among 56 patients, 29 patients were assigned to the intervention group (13 males; mean age 57.38±14.22 years) and 27 patients (14 males; mean age 56.15±14.55) to the control group. No difference in sex, distribution of age, current smoking, current drinking, diabetes, hypertension, type of stoke, GCS, and duration between first and final oral evaluation was observed between the intervention and control groups (p>0.05) (Table 1).
At the first evaluation, we did not observe significant difference in the DMFT index, including the decayed teeth index, missing teeth index, and filling teeth index, PI, GI, CAL, and colonization degree of Candida on the tongue and in saliva between the intervention and control groups (p>0.05). However, the tooth mobility index (0.19±0.30) of the intervention group was significantly higher than that (0.06±0.12) of the control group (p<0.05) (Table 2). A summary of the change of oral health status between the first and second evaluations is shown in Table 3. The PI and GI was significantly lower in the intervention group, compared to those of the control group (p<0.05). By contrast, no significant difference was observed in the CAL of the intervention group (p>0.05) (Table 3). The degree of colonization of Candida on the tongue showed a statistically insignificant decrease in the intervention group (p>0.05); however, a significant decrease was observed in the saliva (p<0.05) (Table 4). None of the patients in the intervention group showed any complications or side effects during the OHCP.
In this study, we investigated the effect of an OHCP administered to stroke patients during their stay in the ICU. We found that the intervention group showed decrement in terms of the PI, GI, and the colonization degree of Candida in saliva, compared with the control group. However, no difference was observed in the CAL and the colonization degree of Candida on the tongue.
The findings of the PI and GI appear to indicate that daily tooth brushing removed plaque on the teeth, consequently resulting in improvement of periodontal health. In addition, these results coincide with the results of a previous study showing that systematic oral care reduced plaque and gingival health in dependent elderly persons in a nursing home.14 Therefore, our results emphasize the importance of regular plaque removal from the teeth and mucous membranes of stroke patients during their stay in the ICU.
The CAL indicates the distance from the cement-enamel junction in an apical direction to the base of the periodontal pocket, and is one of the criteria for establishing the severity of periodontitis.21,22 Considering that periodontitis is a chronic disease, any change of the CAL happens over a long period.23 Therefore, our result showing that the CAL was not improved in the intervention group appeared to be attributed to the fact that our OHCP was performed only an average of 2.2 weeks.
The colonization degree of Candida on the tongue showed a greater decrease in the intervention group than in the control group, without statistical significance. On the contrary, the colonization degree of Candida in saliva showed a significant decrease in the intervention group. These results suggest that our OHCP, in which plaque control using a children's toothbrush and an interdental toothbrush was administered along with use of chlorohexidine, had an effect on the decrease of colonization of Candida in both the tongue and saliva. However, our OHCP was not as effective for the tongue as for as saliva. Therefore, we believe that additional measures to decrease the colonization of Candida on the tongue should be added in future OHCPs. Our results are compatible with those of previous studies showing that plaque control by tooth brushing can decrease the colonization of Candida in saliva.24,25
In the current study, we used a children's toothbrush and an interdental toothbrush for removal of plaque on teeth, tongue cleaner to get rid of plaque on the tongue, and gauze soaked with 0.5% chlorohexidine was used to clean oral mucosa and tooth surfaces. Protocols for oral hygienic management that have been reported until recently are mainly for use of gauze soaked with physiological saline solution,13 hydrogen peroxide, chlorohexidine, betadine, and nystatin in order to wipe off teeth or soft tissue in the mouth or to perform toothbrushing.26-31 Hydrogen peroxide is not recommended because it can be a stimulus to oral mucosa when it is not properly diluted.6,26 Physiological saline solution has frequently been used for the oral hygienic program because it does not change acidity without destruction of granulation tissue. However, it is insufficient for use with critical patients with an endotracheal tube inserted because the solution provides a low antibacterial effect.32 On the contrary, chlorohexidine has recently been employed in the OHCP due to its antibacterial effect. In addition, it inhibits formation of dental plaque or decreases clustering of microorganisms in the mouth. As a result, chlorohexidine is known to have a strong effect in reducing the pneumonia pathogen.29 Yet, tooth brushing is more effective than use of gauze for removal of dental plaque. However, tooth brushing was not recommended as a method of oral hygiene management for patients in the ICU because it may change the location of the endotracheal tube and can cause bleeding by causing injury to the oral mucous membrane.5,33 Instead, a small children's toothbrush was recommended for use with patients in the ICU.34 In this study, we employed a children's toothbrush and an interdental toothbrush, and we did not observe any complication during our OHCP. Therefore, we believe that a children's toothbrush and an interdental toothbrush would be safe for stroke patients in the ICU.
In conclusion, we found that our OHCP was effective and safe in improving the oral hygienic status and periodontal health of stroke patients during their stay in the ICU; therefore, administration is recommended accordingly. We believe that the methods and results of this study can be used as an important basis for development of a more advanced OHCP for patients with stroke or those in the ICU.
To the best of our knowledge, this is the first study to investigate the effect of an OHCP on stroke patients in the ICU. However, some limitations of this study should be considered. First, complete randomization was not performed throughout the entire process of research. Simple randomization often cannot reflect the whole characteristics of target population so allocation was implemented with matching by age and sex in order to get better comparability. In addition, many patients dropped out of this intervention program after allocation, although this study was a kind of randomized controlled intervention trial. However, the distribution of major characteristics between the intervention and control groups at baseline of the two final groups was very likely to be similar. Second, this kind of intervention program provided by a dentist at ICU is not a standard clinical practice. The oral health care program was implemented only for the intervention group so it was impossible for the dentist not to know whether the participant had taken the program or not. However, overestimation of the effect of the intervention may have been minimized because objective clinical parameters measured by a standard assessment protocol were used as outcomes and more intention-to-treat analysis was done as we tried to obtain conservative results. Third, the duration of the OHCP was variable, from one week to five weeks, because the duration of patients' stay in the ICU varied according to the medical state of the patients. This was unavoidable for this kind of study. Yet, we did not observe a difference in terms of duration in the ICU between the intervention and control groups. Fourth, we did not investigate the long-term effect of this OHCP. Finally, we did not evaluate the incidence of systemic infection, which is one of the important goals in administration of an OHCP. Therefore, conduct of further long-term follow up studies for the evaluation of the long-term effect and the incidence of systemic infection should be encouraged.
Figures and Tables
Table 1
Distributions of Clinic-Demographic Data between the Control and Intervention Groups at Baseline

References
1. Yoshida M, Murakami T, Yoshimura O, Akagawa Y. The evaluation of oral health in stroke patients. Gerodontology. 2012; 29:e489–e493.

2. Munro CL, Grap MJ. Oral health and care in the intensive care unit: state of the science. Am J Crit Care. 2004; 13:25–33.

4. O'Neal PV, Brown N, Munro C. Physiologic factors contributing to a transition in oral immunity among mechanically ventilated adults. Biol Res Nurs. 2002; 3:132–139.
5. Ames NJ. Evidence to support tooth brushing in critically ill patients. Am J Crit Care. 2011; 20:242–250.

6. Grap MJ, Munro CL, Ashtiani B, Bryant S. Oral care interventions in critical care: frequency and documentation. Am J Crit Care. 2003; 12:113–118.

7. Chambers MS, Toth BB, Martin JW, Fleming TJ, Lemon JC. Oral and dental management of the cancer patient: prevention and treatment of complications. Support Care Cancer. 1995; 3:168–175.

8. Wehmeyer MM, Corwin CL, Guthmiller JM, Lee JY. The impact of oral health literacy on periodontal health status. J Public Health Dent. 2012:[Epub ahead of print].

9. Offenbacher S, Barros SP, Altarawneh S, Beck JD, Loewy ZG. Impact of tooth loss on oral and systemic health. Gen Dent. 2012; 60:494–500.
10. Scannapieco FA, Stewart EM, Mylotte JM. Colonization of dental plaque by respiratory pathogens in medical intensive care patients. Crit Care Med. 1992; 20:740–745.

11. Mori H, Hirasawa H, Oda S, Shiga H, Matsuda K, Nakamura M. Oral care reduces incidence of ventilator-associated pneumonia in ICU populations. Intensive Care Med. 2006; 32:230–236.

12. Craven DE, Kunches LM, Kilinsky V, Lichtenberg DA, Make BJ, McCabe WR. Risk factors for pneumonia and fatality in patients receiving continuous mechanical ventilation. Am Rev Respir Dis. 1986; 133:792–796.
13. Fagon JY, Chastre J, Domart Y, Trouillet JL, Gibert C. Mortality due to ventilator-associated pneumonia or colonization with Pseudomonas or Acinetobacter species: assessment by quantitative culture of samples obtained by a protected specimen brush. Clin Infect Dis. 1996; 23:538–542.

14. Sumi Y, Nakamura Y, Michiwaki Y. Development of a systematic oral care program for frail elderly persons. Spec Care Dentist. 2002; 22:151–155.

15. Lee HK, Choi SH, Won KC, Merchant AT, Song KB, Jeong SH, et al. The effect of intensive oral hygiene care on gingivitis and periodontal destruction in type 2 diabetic patients. Yonsei Med J. 2009; 50:529–536.

16. Chen ZY, Chiang CH, Huang CC, Chung CM, Chan WL, Huang PH, et al. The association of tooth scaling and decreased cardiovascular disease: a nationwide population-based study. Am J Med. 2012; 125:568–575.

17. Teasdale G, Jennett B. Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974; 2:81–84.
18. Giargia M, Lindhe J. Tooth mobility and periodontal disease. J Clin Periodontol. 1997; 24:785–795.

19. Löe H. The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol. 1967; 38:Suppl. 610–616.

20. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964; 22:121–135.

21. Pihlstrom BL. Measurement of attachment level in clinical trials: probing methods. J Periodontol. 1992; 63:12 Suppl. 1072–1077.

22. Machtei EE, Christersson LA, Grossi SG, Dunford R, Zambon JJ, Genco RJ. Clinical criteria for the definition of "established periodontitis". J Periodontol. 1992; 63:206–214.

23. Newman MG, Takei HH, Carranza FA. Carranza's clinical periodontology. 11th ed. St. Louis, MO.: Elsevier/Saunders;2012.
24. Abe S, Ishihara K, Okuda K. Prevalence of potential respiratory pathogens in the mouths of elderly patients and effects of professional oral care. Arch Gerontol Geriatr. 2001; 32:45–55.

25. das Chagas MS, Portela MB, Cerqueira DF, de Souza IP, Soares RM, Castro GF. Reduction of Candida species colonization in the oral cavity of children infected with human immunodeficiency virus after dental treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:383–388.

26. Tombes MB, Gallucci B. The effects of hydrogen peroxide rinses on the normal oral mucosa. Nurs Res. 1993; 42:332–337.

27. Genuit T, Bochicchio G, Napolitano LM, McCarter RJ, Roghman MC. Prophylactic chlorhexidine oral rinse decreases ventilator-associated pneumonia in surgical ICU patients. Surg Infect (Larchmt). 2001; 2:5–18.

28. Masaki H, Yoshimine H, Degawa S, Asoh N, Tao M, Matsumoto K, et al. [Importance of a cleaning in upper airways by using povidone iodine for the prevention of nosocomial pneumonia]. Kansenshogaku Zasshi. 2001; 75:97–102.

29. Grap MJ, Munro CL, Elswick RK Jr, Sessler CN, Ward KR. Duration of action of a single, early oral application of chlorhexidine on oral microbial flora in mechanically ventilated patients: a pilot study. Heart Lung. 2004; 33:83–91.

30. Normand S, François B, Dardé ML, Bouteille B, Bonnivard M, Preux PM, et al. Oral nystatin prophylaxis of Candida spp. colonization in ventilated critically ill patients. Intensive Care Med. 2005; 31:1508–1513.

31. Kovac M, Mitic G, Kovac Z. Miconazole and nystatin used as topical antifungal drugs interact equally strongly with warfarin. J Clin Pharm Ther. 2012; 37:45–48.

32. Choi SH, Kim YK. The effect of oral care with normal saline on oral state of patients in intensive care unit. J Korean Acad Adult Nurs. 2004; 16:452–459.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download