Abstract
Purpose
Hypothermia adversely affects the coagulation that could be of clinical significance in patients receiving clopidogrel. We evaluated the influence of hypothermia on transfusion requirements in patients undergoing isolated off-pump coronary artery bypass surgery (OPCAB) who continued clopidogrel use within 5 days of surgery.
Materials and Methods
Protocol-based, prospectively entered data of 369 patients were retrospectively reviewed. The time-weighted average of intraoperative temperatures and the temperature upon ICU admission (TWA-temp) was assessed. Patients were divided into normothermia (≥36℃, n=224) and hypothermia (<36℃, n=145) group. The transfusion requirement for perioperative blood loss was assessed and compared.
Results
Patients with hypothermia were older and had lower body surface area (BSA) than patients with normothermia. Age and BSA adjusted transfusion requirement was significantly larger in the hypothermia group [patients requiring transfusion: 64% versus 48%, p=0.003; number of units: 0 (0-2) units versus 2 (0-3) units, p=0.002]. In multivariate analysis of predictors of perioperative multiple transfusion requirements, hypothermia was identified as an independent risk factor along with age, female gender, BSA, chronic kidney disease, and congestive heart failure.
Conclusion
Hypothermia was associated with increased transfusion requirement in patients undergoing OPCAB who received clopidogrel in proximity to surgery. Considering the high prevalence and the possibility of hypothermia being a modifiable risk factor, aggressive measures should be undertaken to maintain normothermia in those patients.
With an increasing amount of evidence suggesting an ischemic benefit of some degree of platelet inhibition at the time of coronary artery bypass graft surgery (CABG), off-pump coronary artery bypass surgery (OPCAB) is gaining renewed interest in patients who continue clopidogrel as it is devoid of platelet dysfunction or thrombocytopenia inherent to cardiopulmonary bypass (CPB).1-3 Still, continued dual antiplatelet therapy carries the risk of hemorrhagic complications. Notwithstanding the clear association between the transfusion of allogeneic blood products and adverse outcome in cardiac surgical patients, any modifiable risk factors should be sought and corrected.4
Hypothermia is frequently encountered during and/or after surgical procedures requiring admission to the intensive care unit (ICU).5 Although hypothermia is known to decrease the metabolic demand of the body and provide tolerance to ischemia, it is also associated with deleterious physiologic alterations. Hypothermia results in coagulopathy,6 acidosis with a leftward shift of the oxygen-hemoglobin dissociation curve,7 impaired immune function/infectious complications,8 and arrhythmias/hemodynamic instability.9 Indeed, previous studies depicted the predictive role of hypothermia at the time of ICU admission on adverse outcomes after CABG.10,11
However, no previous study has addressed the relationship between hypothermia and transfusion requirement in patients undergoing OPCAB. This is of interest since hypothermia is potentially modifiable risk factor of bleeding and transfusion requirement. The core temperature of a post-surgical patient at the time of ICU admission should be influenced by intraoperative temperature changes considering the temporal relation. As most of the perioperative bleeding and transfusion usually occur within a few hours after surgery, the time-weighted average of intraoperative temperatures and the temperature upon ICU admission (TWA-temp) may be associated with an increased transfusion requirement.
The aim of this retrospective study was to evaluate the influence of TWA-temp on perioperative transfusion requirement in patients undergoing OPCAB who continued clopidogrel use within 5 days of surgery.
After approval by the Institutional Review Board, we retrospectively reviewed electronic medical records of 768 consecutive patients who underwent elective, isolated OPCAB between January 2009 and February 2012 at the Cardiovascular Hospital of Yonsei University College of Medicine. The need to obtain written consent from patients was waived by the Institutional Review Board. Exclusion criteria for patients were as follows: discontinued clopidogrel therapy >5 days before surgery (n=166), preexisting hypothermia (<36℃) or hyperthermia (>38℃, n=1), already enrolled in another randomized controlled trial (n=207), required emergent or salvage operations (n=21), required emergent conversion to an on-pump procedure (n=2), a postoperative temperature >38℃ (n=2). After careful examination of the clinical data, 369 patients were enrolled and analyzed.
All patients received standard perioperative care, which was described previously.12 Briefly, standard monitoring included a pulmonary artery (PA) catheter and transesophageal echocardiography. Anesthesia consisted of sufentanil and sevoflurane, and a median sternotomy was performed in all surgical procedures. A cell salvage device was used intraoperatively in all patients and the salvaged blood was returned to the patient before the end of surgery. In all patients, a fluid warmer, a warm mattress, and a forced warm-air blanket were used to maintain blood temperature between 36℃ and 37℃ which was measured by the PA catheter. During grafting, activated coagulation time was maintained around 250 sec using heparin (80 U/kg), and was neutralized using protamine after completion of the graft. After surgery, all patients were transferred to the ICU. During the perioperative period, packed erythrocytes were transfused when the hematocrit was less than 25%. Patients received fresh frozen plasma when the postoperative international normalized ratio was ≥1.5 with a rate of bleeding >200 mL/hr for two consecutive hours. Platelet concentrates were transfused when the postoperative platelet count was below 50000/mm3 with a same rate of bleeding as described above. All data were retrieved from a protocol-based, and the prospectively entered institutional OPCAB database.
Assessed preoperative variables included demographic data; the presence of diabetes mellitus (DM), hypertension, congestive heart failure (New York Heart Association class III or IV), left ventricular ejection fraction (LVEF), chronic kidney disease (serum creatinine >1.4 mg/dL), or left main disease (>70% stenosis); history of recent myocardial infarction (MI) within the past week of surgery; as well as hematocrit level and medications. The number of patients who received clopidogrel within 2 days of surgery was also assessed.
Assessed operative variables included the duration of surgery, number of grafts performed, use of saphenous vein grafts, vasopressor requirement (amount of norepinephrine hyinfused and number of patients requiring vasopressin), and transfusion requirement. The amount of re-infused blood volume from the cell salvage device was considered as the intraoperative blood loss.
Assessed postoperative variables included highest creatine kinase-MB, number of patients who required milrinone, amount of blood loss, transfusion requirement, length of stay in the ICU and hospital. Composite morbidity/mortality endpoints were also assessed and were defined as having more than one of the following: MI (an increase in creatine kinase-MB 5 times or greater over the upper normal limit, when associated with newly developed Q wave or left bundle branch block on electrocardiogram),13 permanent stroke, acute kidney injury (increase of serum creatinine to >2.0 mg/dL, 2 times higher than most recent preoperative creatinine level or a new requirement for dialysis), hemostatic re-exploration, deep sternal wound infection, ventilator care >48 hr, and in-hospital mortality.14
The TWA-temp for each patient was calculated as the area under the curve divided by the time from first to last measurement. The time points included were: after anesthetic induction, Y-graft construction, during grafting, sternal closure, and upon arrival at the ICU.
The primary endpoint was to compare the amount of perioperative blood loss and transfusion requirement between patients with hypothermia (TWA-temp <36℃) and normothermia (TWA-temp ≥36℃). Independent risk factors of multiple transfusion requirements (≥2 units of packed erythrocytes) were also analyzed.
The secondary endpoint was to compare the incidence of composite morbidity/mortality endpoints between patients with hypothermia and normothermia. Independent risk factors of composite of morbidity/mortality endpoints were also analyzed.
All analyses were performed with SPSS 15.0 (SPSS Inc., Chicago, IL, USA). Intergroup comparisons were done with t-test, Mann-Whitney U test, ANCOVA (for adjustment of age and body surface area), and χ2 test or Fisher's exact test as appropriate. To identify independent predictors of a multiple transfusion requirements, logistic regression models were used. Variables demonstrating a p value of <0.05 between patients who required multiple transfusions or not were first introduced to a univariate logistic regression analysis. Variables with a p value of <0.05 in the univariate analysis were further introduced to multivariate logistic regression analysis to identify independent risk factors. Odds ratios and associated 95% confidence interval were estimated. The same methods were applied to identify risk factors of composite of morbidity/mortality endpoints. Continuous variables are shown as mean±standard deviation (SD) or median (interquartile range), categorical variables were shown as number (percentage). A p value of <0.05 was considered significant.
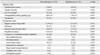
Of the 369 patients, 145 patients were classified as having hypothermia (range; 34.2-35.9℃) based on their TWA-temp measured by the PA catheter during the surgery and upon arrival at the ICU. Accordingly, 224 patients were classified as having normothermia (range; 36-37.5℃). Comparisons of preoperative variables between patients with hypothermia and normothermia are listed in Table 1. Patients with hypothermia were older and had lower body surface area than patients with normothermia. Other characteristics including the presence of co-morbid diseases and left ventricular ejection fraction were all similar between the groups.
Operative characteristics and postoperative outcome variables are listed in Table 2. Operative data including the number of grafts performed were all similar between the groups. In-hospital mortality rate was significantly higher in the hypothermia group (4 vs. 0), two patients died due to aspiration pneumonia and two patients due to cardiac failure. However, we found no difference between other outcome variables including the endpoints of composite morbidity/mortality between the groups. The trend towards a longer length of hospital stay in the hypothermia group was observed when compared with the normothermia group.
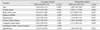
Age and body surface area adjusted comparisons of perioperative blood loss and transfusion requirement are listed in Table 3. Overall, a significantly larger percentage of patients in the hypothermia group required packed erythrocytes transfusion compared with the normothermia group. In addition, significantly more units of packed erythrocytes were transfused in the hypothermia group compared with the normothermia group. The percentage of patients requiring multiple transfusions was significantly higher in the hypothermia group compared with the normothermia group.
In the multivariate analysis of predictors of perioperative multiple transfusion requirements, hypothermia was identified as an independent risk factor along with age, female gender, body surface area, chronic kidney disease and congestive heart failure (Table 4).
In the multivariate analysis of predictors of composite of morbidity/mortality endpoints, recent MI and chronic kidney disease were identified as independent predictors (Table 5).
In the current retrospective study, we found that hypothermia (TWA-temp measured during the intraoperative period and upon arrival at the ICU) was associated with an increased perioperative transfusion requirement in patients undergoing OPCAB who continued clopidogrel use within 5 days of surgery. Moreover, hypothermia was also found to be an independent risk factor of perioperative multiple transfusion requirements. Although the mortality rate was higher in the hypothermia group, no association was observed between hypothermia and a composite of morbidity/mortality endpoints.
Dual antiplatelet therapy comprised of aspirin and clopidogrel has long been accepted as an essential therapy for patients with coronary artery disease.15 Accordingly, an increasing number of patients presenting for CABG are exposed to platelet inhibition and are at increased risk of hemorrhagic complications. Yet, considering the existence of an ischemic and even a mortality benefit imposed by the antiplatelet therapy outweighing the bleeding risk, recent literature advocates the importance of some degree of platelet inhibition at the time of CABG.1,3 In order to maximize the ischemic benefit and minimize the bleeding risk, OPCAB has been proposed as an alternative technique to on-pump CABG, as it is associated with limited deterioration in platelet function and counts frequently observed after CPB.16 However, several studies backed the safety of OPCAB in patients who continued clopidogrel in terms of bleeding and transfusion requirement, thus transfusion is not uncommon in OPCAB.2,17,18
Transfusion of allogeneic blood products is known to be associated with adverse outcomes that carry risks far beyond that of transmitting infectious diseases.4 Thus identification of risk factors would be of major clinical importance not only for risk stratification, but also for the future development of therapeutic measures aimed at modifying the identified risk factors resulting in improved patients' outcome. Previously known risk factors of bleeding and transfusion requirement in patients undergoing CABG are multiple. These include age, female gender, weight, DM, chronic kidney disease, poor LVEF, preoperative hematocrit value, and a history of MI.18,19 Yet, most of these factors are not readily amenable to modifications at the time of CABG.
Hypothermia is a frequently accompanied phenomenon in patients undergoing major surgical procedures. In the case of OPCAB, 46.7% of the patients were reported to be hypothermic after leaving the operating room.11 Apart from its beneficial influence of providing organ protection against ischemia-reperfusion injury, hypothermia is associated with a multitude of adverse physiologic alterations. In terms of coagulation, hypothermia has been shown to be associated with platelet dysfunction as well as a mild decrease in platelet counts.20 Proposed mechanisms include impaired thromboxane A2 release and inhibited exposure of P-selectin on the platelet surface.21 Moreover, hypothermia has been shown to inhibit coagulation enzyme activities delaying the onset of thrombin generation.22 Hypothermia is also often accompanied by acidosis, which in turn results in profound inhibition of thrombin generation in the propagation phase.22,23 These adverse influences of hypothermia, especially on platelet function, may exert significant clinical influence in coronary patients presenting for surgery with some degree of platelet inhibition to maximize the ischemic benefit of antiplatelet therapy. Mild hypothermia was shown to counteract the platelet-inhibitory effect of clopidogrel, when clopidogrel was administered concomitantly in the presence of hypothermia.24,25 However, binding of clopidogrel to the P2Y12 receptor is irreversible and the influence of hypothermia on the clopidogrel's platelet-inhibitory function in patients who already reached steady-state by previous continuous administration remains elusive.
In a previous study, even mild hypothermia (<0.5℃) has been shown to be associated with increased blood loss and transfusion requirement in patients undergoing hip arthroplasty although none of the patients studied were exposed to antiplatelet therapy in proximity to surgery.26 Of particular interest, a follow-up study reported that aggressive warming reduced blood loss during the same surgical procedure implicating that hypothermia may be a modifiable risk factor of perioperative bleeding and transfusion requirement.27 As of yet, no comprehensive data exist regarding the influence of hypothermia on bleeding and transfusion requirement in patients undergoing OPCAB who continued dual antiplatelet therapy within 5 days of surgery.
In the current study, despite the application of a fluid warmer, warm mattress, and a forced warm-air blanket in all patients, 39% of the patients were hypothermic. The amount of the perioperative blood loss was greater in the hypothermia group; however, this finding was without statistical significance. This may be attributable to the inaccurate assessment of intraoperative blood loss. In the current study, intraoperative blood loss was assessed only as the amount of blood salvaged by a cell salvage device not accounting for the other unmeasured and insensible blood loss. Still, transfusion requirement was significantly greater in patients with hypothermia despite that other risk factors of bleeding and transfusion requirement including the baseline hematocrit values. In addition, the number of grafts performed was similar between patients with normothermia and hypothermia. Moreover, hypothermia was found to be an independent risk factor of multiple transfusion requirements along with the previously known factors such as age, female gender, body surface area, chronic kidney disease, and congestive heart failure. Thus, the results of the current study clearly implicate the association between hypothermia and transfusion requirement in patients undergoing OPCAB who continued dual antiplatelet therapy.
Of interest and in contrast to the findings of the previous studies, we did not observe any association between hypothermia and the composite morbidity/mortality endpoints in the current study. These conflicting results may be attributable to the fact that the previous studies only used a single measurement of temperature upon arrival at the ICU and that patient management was not according to a standardized protocol.10,11,28 In addition, a recent study involving the largest cohort of cardiac surgical patients depicted that transient hypothermia was not associated with adverse outcome.29 In that study, only persistent postoperative hypothermia was associated with increased mortality, whereas none of the patients in the current study were persistently hypothermic in the postoperative period by way of active warming. Thus, addressing the influence of postoperative hypothermia on outcome was not possible in the current trial. Although we observed a significantly higher mortality rate in the hypothermia group, the sample size is too small to draw a definite conclusion regarding the association between hypothermia and death from the current study.
The strengths of this study are that all of the data were collected from a prospectively enrolled database and that temperature measurements were protocol-based using the TWA-temp instead of a single measurement. Due to the temporal continuity, intraoperative temperatures essentially influence the temperature upon ICU arrival, and only the latter had been validated in most of the previous studies.10,11,28 Postoperative persistent hypothermia may affect bleeding as well, however, it was not possible to address this relationship, as all of the patients were normothermic within 2 hr after the surgery. Also, considering that most of the postoperative bleeding occurs within the first 4 hr after the surgery, TWA-temp seems to be the ideal variable to address the influence of hypothermia on perioperative bleeding and transfusion requirement. Nonetheless, the retrospective nature of this study is a significant limitation. Another limitation is that we did not assess the inter-individual variability of clopidogrel responsiveness. This may also affect the bleeding and transfusion requirement.30 Yet, there is currently no standardized test assessing the clopidogrel responsiveness with enough clinical evidence to support its association with hemorrhagic complications. Another limitation is that we could not accurately assess the amount of intraoperative blood loss, instead we used the volume of salvaged blood as a surrogate. Despite significant differences in transfusion requirements, intraoperative blood loss was similar among patients, whereas postoperative blood loss only slightly greater in the hypothermia group. Considering that the baseline hematocrit level was similar between both groups and that all other operative data were similar, we can only speculate that intraoperative blood loss may have been greater in the hypothermia group.
In conclusion, perioperative hypothermia assessed by TWA-temp was associated with an increased transfusion requirement in patients undergoing OPCAB who continued dual antiplatelet therapy until 5 days of surgery. Considering the high prevalence of hypothermia and the possibility of hypothermia being a modifiable risk factor of transfusion requirement, more aggressive measures should be undertaken to maintain normothermia in those patients.
Figures and Tables
References
1. Montalescot G, Hulot JS, Collet JP. Antiplatelet therapy and coronary artery bypass graft surgery a fallow land. J Am Coll Cardiol. 2010; 56:2003–2005.
2. Shim JK, Choi YS, Oh YJ, Bang SO, Yoo KJ, Kwak YL. Effects of preoperative aspirin and clopidogrel therapy on perioperative blood loss and blood transfusion requirements in patients undergoing off-pump coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2007; 134:59–64.

3. Mehta SR, Yusuf S. Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) Study Investigators. The Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) trial programme; rationale, design and baseline characteristics including a meta-analysis of the effects of thienopyridines in vascular disease. Eur Heart J. 2000; 21:2033–2041.

4. Hajjar LA, Vincent JL, Galas FR, Nakamura RE, Silva CM, Santos MH, et al. Transfusion requirements after cardiac surgery: the TRACS randomized controlled trial. JAMA. 2010; 304:1559–1567.
5. Karalapillai D, Story D. Hypothermia on arrival in the intensive care unit after surgery. Crit Care Resusc. 2008; 10:116–119.
6. Krause KR, Howells GA, Buhs CL, Hernandez DA, Bair H, Schuster M, et al. Hypothermia-induced coagulopathy during hemorrhagic shock. Am Surg. 2000; 66:348–354.
7. Frank SM, Higgins MS, Fleisher LA, Sitzmann JV, Raff H, Breslow MJ. Adrenergic, respiratory, and cardiovascular effects of core cooling in humans. Am J Physiol. 1997; 272(2 Pt 2):R557–R562.

8. Ishikawa K, Tanaka H, Shiozaki T, Takaoka M, Ogura H, Kishi M, et al. Characteristics of infection and leukocyte count in severely head-injured patients treated with mild hypothermia. J Trauma. 2000; 49:912–922.

9. Frank SM, Higgins MS, Breslow MJ, Fleisher LA, Gorman RB, Sitzmann JV, et al. The catecholamine, cortisol, and hemodynamic responses to mild perioperative hypothermia. A randomized clinical trial. Anesthesiology. 1995; 82:83–93.

10. Insler SR, O'Connor MS, Leventhal MJ, Nelson DR, Starr NJ. Association between postoperative hypothermia and adverse outcome after coronary artery bypass surgery. Ann Thorac Surg. 2000; 70:175–181.

11. Hannan EL, Samadashvili Z, Wechsler A, Jordan D, Lahey SJ, Culliford AT, et al. The relationship between perioperative temperature and adverse outcomes after off-pump coronary artery bypass graft surgery. J Thorac Cardiovasc Surg. 2010; 139:1568–1575.

12. Oh SY, Shim JK, Song JW, Kim JC, You KJ, Kwak YL. Cardiac displacement-induced hemodynamic instability during off-pump coronary artery bypass surgery and its predictors. Acta Anaesthesiol Scand. 2011; 55:870–877.

13. Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, et al. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. Circulation. 2007; 116:2634–2653.
14. Antunes PE, de Oliveira JF, Antunes MJ. Risk-prediction for postoperative major morbidity in coronary surgery. Eur J Cardiothorac Surg. 2009; 35:760–766.

15. Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE Jr, et al. ACC/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-Elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007; 50:e1–e157.
16. Casati V, Gerli C, Franco A, Della Valle P, Benussi S, Alfieri O, et al. Activation of coagulation and fibrinolysis during coronary surgery: on-pump versus off-pump techniques. Anesthesiology. 2001; 95:1103–1109.
17. Maltais S, Perrault LP, Do QB. Effect of clopidogrel on bleeding and transfusions after off-pump coronary artery bypass graft surgery: impact of discontinuation prior to surgery. Eur J Cardiothorac Surg. 2008; 34:127–131.

18. Frankel TL, Stamou SC, Lowery RC, Kapetanakis EI, Hill PC, Haile E, et al. Risk factors for hemorrhage-related reexploration and blood transfusion after conventional versus coronary revascularization without cardiopulmonary bypass. Eur J Cardiothorac Surg. 2005; 27:494–500.

19. Kapetanakis EI, Medlam DA, Petro KR, Haile E, Hill PC, Dullum MK, et al. Effect of clopidogrel premedication in off-pump cardiac surgery: are we forfeiting the benefits of reduced hemorrhagic sequelae? Circulation. 2006; 113:1667–1674.

20. Valeri CR, Khabbaz K, Khuri SF, Marquardt C, Ragno G, Feingold H, et al. Effect of skin temperature on platelet function in patients undergoing extracorporeal bypass. J Thorac Cardiovasc Surg. 1992; 104:108–116.

21. Michelson AD, MacGregor H, Barnard MR, Kestin AS, Rohrer MJ, Valeri CR. Reversible inhibition of human platelet activation by hypothermia in vivo and in vitro. Thromb Haemost. 1994; 71:633–640.

22. Martini WZ, Pusateri AE, Uscilowicz JM, Delgado AV, Holcomb JB. Independent contributions of hypothermia and acidosis to coagulopathy in swine. J Trauma. 2005; 58:1002–1009.

23. Romsi P, Heikkinen J, Biancari F, Pokela M, Rimpiläinen J, Vainionpää V, et al. Prolonged mild hypothermia after experimental hypothermic circulatory arrest in a chronic porcine model. J Thorac Cardiovasc Surg. 2002; 123:724–734.

24. Bjelland TW, Hjertner Ø, Klepstad P, Kaisen K, Dale O, Haugen BO. Antiplatelet effect of clopidogrel is reduced in patients treated with therapeutic hypothermia after cardiac arrest. Resuscitation. 2010; 81:1627–1631.

25. Högberg C, Erlinge D, Braun OO. Mild hypothermia does not attenuate platelet aggregation and may even increase ADP-stimulated platelet aggregation after clopidogrel treatment. Thromb J. 2009; 7:2.

26. Schmied H, Kurz A, Sessler DI, Kozek S, Reiter A. Mild hypothermia increases blood loss and transfusion requirements during total hip arthroplasty. Lancet. 1996; 347:289–292.

27. Winkler M, Akça O, Birkenberg B, Hetz H, Scheck T, Arkiliç CF, et al. Aggressive warming reduces blood loss during hip arthroplasty. Anesth Analg. 2000; 91:978–984.

28. Lahtinen J, Biancari F, Ala-Kokko T, Rainio P, Salmela E, Pokela R, et al. Pulmonary artery blood temperature at admission to the intensive care unit is predictive of outcome after on-pump coronary artery bypass surgery. Scand Cardiovasc J. 2004; 38:104–112.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download