Abstract
Purpose
To evaluate changes in clinical outcomes, inflammatory cytokine levels, and tear osmolarity in the tears of patients with moderate to severe dry eye syndrome before and after the application of topical 1% methylprednisolone.
Materials and Methods
Thirty-two patients with moderate to severe dry eye unresponsive to previous aqueous enhancement therapy were enrolled. Five patients were lost to follow up, and twenty-seven patients were eligible for analysis. Patients were instructed to apply topical 1% methylprednisolone four times per day, as well as to continue applying their current therapy of preservative-free 0.1% sodium hyaluronate four times per day. Corneal and conjunctival staining scores, tear film breakup time (TFBUT), Schirmer test, and tear osmolarity were assessed at baseline, 4 weeks, and 8 weeks. Tear samples were collected at every visit for cytokine analysis.
Results
Corneal and conjunctival staining scores and TFBUT showed significant improvement at 4 (p<0.001, <0.001, <0.001 respectively) and 8 (p<0.001, <0.001, <0.001 respectively) weeks. Tear osmolarity decreased significantly at 8 weeks (p=0.008). Interleukin (IL)-1β, IL-8, and monocyte chemoattractant protein-1 were significantly decreased at 8 weeks compared with those at baseline (p=0.041, 0.001, 0.008 respectively).
Conclusion
Short-term treatment with topical 1% methylprednisolone not only improved clinical outcomes, but also decreased tear osmolarity and cytokine levels. By measuring the changes in cytokine levels and tear osmolarity, we could objectively evaluate the anti-inflammatory effects of topical methylprednisolone applied in the treatment of patients with moderate to severe dry eye syndrome.
Dry eye syndrome is a common condition that affects approximately 10-20% of the adult population.1 The disease is associated with subjective symptoms, objective signs, including tear film instability, and ocular surface inflammation.2,3
While the pathogenesis of dry eye syndrome has not been clearly established, there is increasing evidence that ocular surface inflammation plays a key role. Increased levels of osmolarity and inflammatory cytokines have been detected in the tears of dry eye patients,4-8 and immunopathological changes have also been detected in the conjunctiva of patients with dry eye syndrome.9
Clinical evidence has shown that topical anti-inflammatory treatments are effective in the treatment of dry eye syndrome.10-12 Topical methylprednisolone has been reported to reduce the levels of inflammatory cytokines in experimental murine dry eyes.13
Although previous studies have confirmed that the tears of dry eye syndrome patients have increased inflammatory cytokine levels and osmolarity,4-8 few studies have investigated changes in inflammatory cytokine levels and tear osmolarity before and after treatment.14,15 Byun, et al.14 measured changes in proinflammatory cytokines, interleukin (IL)-6, and IL-8, to compare the efficacy of the combined use of methylprednisolone and topical cyclosporine with the use of topical cyclosporine alone. Tear osmolarity measured using a TearLab osmometer showed significant reductions in all groups treated with different artificial tears.15 In this study, we performed an analysis of multiple cytokines including IL-6 and IL-8 using immunobead assay, and simultaneously measured changes in tear osmolarity after treatment with topical corticosteroid.
The aim of this study was to evaluate changes in clinical outcomes, levels of inflammatory cytokines, and tear osmolarity in patients with dry eye syndrome after treatment with topical 1% methylprednisolone.
Thirty-two patients with moderate to severe dry eye syndrome whose signs and symptoms were unresponsive to previous aqueous enhancement therapy with 0.1% sodium hyaluronate for 8 weeks were enrolled in this study. Inclusion criteria were as follows: tear film breakup time (TFBUT) less than 5 seconds, Schirmer I test less than 5 mm, and positive corneal and conjunctival staining. Exclusion criteria included any evidence of acute or chronic infection, any inflammatory condition of the cornea and conjunctiva other than dry eye syndrome, history of ocular surgery, use of contact lenses, use of other topical ocular medications, history of known collagen vascular disease such as patients with secondary Sjögren syndrome or positive serology of autoantibodies, and history of adverse events to the study medication. The study was approved by the Institutional Review Board of Severance Hospital and conducted according to the Declaration of Helsinki and Good Clinical Practices. Informed consent was obtained from all patients.
This study was designed as a prospective study. Patients were instructed to apply a drop of topical 1% methylprednisolone four times per day at six-hour intervals in addition to continuing their previous aqueous enhancement therapy for 8 weeks, which consisted of applying preservative-free 0.1% sodium hyaluronate four times per day. All of the following parameters were evaluated at baseline, 4 weeks, and 8 weeks: fluorescein corneal and conjunctival staining, TFBUT, Schirmer test, tear osmolarity, and tear collection for cytokine analysis. To minimize the effect of other examinations, tear osmolarity was measured first and Schirmer test was performed last.
Topical methylprednisolone was prepared by diluting intravenous methylprednisolone sodium succinate (Solu-medrol®, Pfizer, New York, NY, USA) in non-preserved sterile normal saline at a final concentration of 1%.10
The degree of staining was measured for each of the five regions of the cornea: central, superior, temporal, nasal, and inferior. The degree of staining was based on the following: grade 0 (normal), no staining; grade 1 (mild), superficial stippling and micropunctate staining; grade 2 (moderate), macropunctate staining with some coalescent areas; and grade 3 (severe), numerous coalescent macropunctate areas and/or patches. Each of the five regions was graded on a scale from 0 to 3. The scores of the five areas were added to obtain a total score for each eye.
The degree of staining was separately assessed for the three portions of the temporal conjunctiva and the three portions of the nasal conjunctiva on a scale from 0 to 3. The scores for each of the six areas were added to obtain a total score for each eye.
Fluorescein strip was wet with a drop-volume of non-preserved saline solution and the strip was touched to the inferior palpebral conjunctiva. Patients were asked to blink several times. The investigator monitored the integrity of the tear film with a slit lamp and measured up to the time until one or more dry spots appeared in the precorneal tear film from the last blink. Schirmer I test with topical anesthesia was performed to evaluate basal tear secretion.
Thirty µL of phosphate-buffered saline was instilled into the conjunctival sac, and patients were instructed to blink slightly once. A 20-µL volume of tear fluid and buffer were collected with a micropipette at the lateral canthus, avoiding any additional tear reflex. During collection of tear fluid, patients were instructed not to blink and to keep looking up to avoid damage to the corneal epithelium. The fluid was placed into a 1.5 mL Eppendorf tube and the tube was vortexed briefly to reduce the adherence of tear proteins to the sides of tube, which was stored at -70℃ until further examination.
Cytokine concentrations were measured using both multiplex immunobead assay (BD™ Cytometric Bead Array Human Soluble Protein Flex Set, BD Biosciences, San Jose, CA, USA) and flow cytometry (BD™ FACS LSR II, BD Biosciences, San Jose, CA, USA). The cytokines and chemokines that were analyzed included IL-1β, IL-6, IL-17, interferon gamma (IFN-γ), tumor necrosis factor (TNF)-α, IL-8, and monocyte chemotactic protein-1 (MCP-1).
Thirty-two patients were enrolled in this study; five patients were lost to follow up after their baseline visit. Twenty-seven patients who completed the study were eligible for analysis (22 females, 5 males; mean age±standard deviation 53.85±13.14, range from 27 to 73 years).
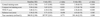
Corneal and conjunctival staining scores and TFBUT showed statistically significant improvement at 4 and 8 weeks compared with baseline. Schirmer test scores were increased at 4 and 8 weeks; however, there were no statistically significant differences. A statistically significant decrease in tear osmolarity was observed at 8 weeks compared with baseline (Table 1).
This study showed that the therapeutic effect of topical 1% methylprednisolone in the treatment of dry eye syndrome could be proven not only by improvements of clinical indices, but also by decreases in tear osmolarity and inflammatory cytokines levels. The important findings, which corroborate previous studies, are that IL-1β and IL-8 in tears were decreased after the treatment with steroid and that tear osmolarity decreases with steroid use.
Tear hyperosmolarity is regarded as the core mechanism causing ocular surface inflammation in dry eye syndrome.3 Hyperosmolarity stimulates a cascade of inflammatory events in the epithelial surface cells, involving mitogen-activated protein kinases (MAPKs), the nuclear factor-kappa B signaling pathway,16 and the generation of inflammatory cytokines (IL-1α, IL-1β, and TNF-α) and MMP-9,13 which activate inflammatory cells at the ocular surface.17,18 Increased levels of multiple pro-inflammatory cytokines in the tears of patients with dry eye syndrome have been confirmed by previous studies.4-6
Tear osmolarity is believed to be a global indicator of the disease3 and has been proposed as the gold standard for diagnosis of dry eyes.19 With technological advances, it is now possible to measure osmolarity using small amounts of tears, and more conveniently, by collecting tear samples from the inferior tear lake with the tip of the test card.
In this study, we intended to propose an objective approach to evaluate the efficacy of topical methylprednisolone in the treatment of patients with dry eye syndrome. Recent studies have shown that inflammatory cytokines and tear osmolarity are increased in dry eye syndrome and that tear osmolarity has a significant correlation with dry eye severity.4-8 By measuring changes in inflammatory cytokine levels and tear osmolarity, we could objectively show an anti-inflammatory effect of methylprednisolone in addition to clinical improvement.
Methylprednisolone has been shown to have great efficacy in preserving corneal epithelial barrier function. De Paiva, et al.13 reported that methylprednisolone decreased levels of IL-1α, IL-1β, and TNF-α transcripts as well as activation of MAPKs. In this study, we confirmed a significant decrease in IL-1β levels after treatment with topical methylprednisolone. The therapeutic effect of methylprednisolone may be the result of indirect MAPKs inhibition by decreasing the production of both IL-1 and TNF-α, MAPKs activators, as corticosteroids have not been recognized as direct MAPKs inhibitors.13,20
IL-17 is a potent pro-inflammatory cytokine, and interaction of IL-17 with its receptor evokes activation of IL-8, resulting in recruitment of neutrophils to the injury site.21 MCP-1 has been identified as a key molecule for the chemotaxis of monocytes to the site of inflammation.22 The results of this study showed that IL-8 and MCP-1 levels were all significantly decreased by topical methylprednisolone. These findings suggest that topical methylprednisolone improved ocular surface inflammation by decreasing the recruitment of inflammatory cells. Other pro-inflammatory cytokines including IL-6, IL-17, and IFN-γ also decreased, but the differences were not statistically significant in this study.
Tear hyperosmolarity arises in situations of low aqueous tear flow, excessive evaporation, or a combination of these events.3 A previous study demonstrated that patients with faster tear film thinning time may be more susceptible to evaporation of the tear film, which may lead to a more concentrated tear film and increased osmolarity.23 In this study, tear film stability (TFBUT) was significantly improved at 4 and 8 weeks, and tear osmolarity significantly decreased at 8 weeks. It is possible that improved tear film stability slowed down tear film thinning time in patients, followed by decreased tear osmolarity.
Tear osmolarity at 4 weeks also showed a decrease from baseline, which was not significant compared to clinical parameters such as corneal and conjunctival staining and TFBUT at 4 weeks. It could mean that epithelial damage and tear film instability were improved relatively faster than a decrease of tear osmolarity in this study. A recent study, which evaluated the efficacy of lubricant eye drops by measuring tear osmolarity, also reported that lubricant eye drops improved TFBUT, Schirmer test values, and fluorescein staining grade; however, tear osmolarity did not change significantly after 30 days of treatment.24 Further investigations would be required to evaluate the relationship between epithelial recovery and decrease of tear osmolarity during the improvement of dry eyes.
Despite its therapeutic effect in the treatment of moderate to severe dry eye, topical methylprednisolone should be used for a short-term period to avoid steroid-related complications such as elevation of intraocular pressure and cataract. In a pervious study which reviewed the efficacy and side effects of topical nonpreserved corticosteroid therapy, there were no complications observed after 2 weeks of therapy; complications including elevated intraocular pressure and cataracts were observed after several months of therapy.10 In another study, which compared the efficacy of topical cyclosporine 0.05% and combined treatment with 1% methylprednisolone acetate, there was no report of elevated intraocular pressure after 3 weeks use of topical steroid in a tapering manner.14 Elevated intraocular pressure was detected in three patients at 8 weeks, but was normalized after stopping the medication in this study. Careful follow-up examination to detect such complications would also be important.
As the therapeutic efficacy of topical steroid is well proven in previous studies,10,11,13 we did not directly compare the efficacy of a topical steroid group with a sodium hyaluronate group. Thus, the results of this study should be interpreted as an effect of topical methylprednisolone in combination with sodium hyaluronate.
Although fluorescein is less ideal for conjunctival staining compared to rose bengal or lissamine green, we graded staining patterns immediately after measuring fluorescein tear breakup time to minimize interactions between tests and to limit the extent of influences of an additional test to the other tests that followed.
Preservatives in topical agents such as benzalkonium chloride excite inflammatory cell markers at the ocular surface, causing epithelial cell damage and a decrease in mucin.3 In this study, topical methylprednisolone was prepared as a non-preserved topical solution to avoid the toxicity associated with a preservative.
In summary, we objectively evaluated the anti-inflammatory effects of topical methylprednisolone applied with non-preserved sodium hyaluronate in the treatment of patients with moderate to severe dry eye syndrome and demonstrated improvements in inflammatory cytokine levels and tear osmolarity after treatment.
Figures and Tables
Fig. 1
Changes in concentration of IL-1β, IL-8, and MCP-1 before and after treatment. IL, interleukin; MCP-1, monocyte chemotactic protein-1.

ACKNOWLEDGEMENTS
This paper was supported by a faculty research grant of Yonsei University College of Medicine for 2013 (6-2013-0036).
We would like to acknowledge Bradford Sgrignoli D.O. for his help with the correction of English and Yura Shin of Hankuk Academy of Foreign Study for her help in analyzing cytokines in the study.
References
1. Johnson ME, Murphy PJ. Changes in the tear film and ocular surface from dry eye syndrome. Prog Retin Eye Res. 2004; 23:449–474.

2. Lemp MA. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J. 1995; 21:221–232.
3. The definition and classification of dry eye disease: report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007; 5:75–92.
4. Massingale ML, Li X, Vallabhajosyula M, Chen D, Wei Y, Asbell PA. Analysis of inflammatory cytokines in the tears of dry eye patients. Cornea. 2009; 28:1023–1027.

5. Lam H, Bleiden L, de Paiva CS, Farley W, Stern ME, Pflugfelder SC. Tear cytokine profiles in dysfunctional tear syndrome. Am J Ophthalmol. 2009; 147:198–205.

6. Yoon KC, Park CS, You IC, Choi HJ, Lee KH, Im SK, et al. Expression of CXCL9, -10, -11, and CXCR3 in the tear film and ocular surface of patients with dry eye syndrome. Invest Ophthalmol Vis Sci. 2010; 51:643–650.

7. Suzuki M, Massingale ML, Ye F, Godbold J, Elfassy T, Vallabhajosyula M, et al. Tear osmolarity as a biomarker for dry eye disease severity. Invest Ophthalmol Vis Sci. 2010; 51:4557–4561.

8. Sullivan BD, Whitmer D, Nichols KK, Tomlinson A, Foulks GN, Geerling G, et al. An objective approach to dry eye disease severity. Invest Ophthalmol Vis Sci. 2010; 51:6125–6130.

9. Stern ME, Gao J, Schwalb TA, Ngo M, Tieu DD, Chan CC, et al. Conjunctival T-cell subpopulations in Sjögren's and non-Sjögren's patients with dry eye. Invest Ophthalmol Vis Sci. 2002; 43:2609–2614.
10. Marsh P, Pflugfelder SC. Topical nonpreserved methylprednisolone therapy for keratoconjunctivitis sicca in Sjögren syndrome. Ophthalmology. 1999; 106:811–816.

11. Lee HK, Ryu IH, Seo KY, Hong S, Kim HC, Kim EK. Topical 0.1% prednisolone lowers nerve growth factor expression in keratoconjunctivitis sicca patients. Ophthalmology. 2006; 113:198–205.

12. Sall K, Stevenson OD, Mundorf TK, Reis BL. CsA Phase 3 Study Group. Two multicenter, randomized studies of the efficacy and safety of cyclosporine ophthalmic emulsion in moderate to severe dry eye disease. Ophthalmology. 2000; 107:631–639.

13. De Paiva CS, Corrales RM, Villarreal AL, Farley WJ, Li DQ, Stern ME, et al. Corticosteroid and doxycycline suppress MMP-9 and inflammatory cytokine expression, MAPK activation in the corneal epithelium in experimental dry eye. Exp Eye Res. 2006; 83:526–535.

14. Byun YJ, Kim TI, Kwon SM, Seo KY, Kim SW, Kim EK, et al. Efficacy of combined 0.05% cyclosporine and 1% methylprednisolone treatment for chronic dry eye. Cornea. 2012; 31:509–513.

15. Tomlinson A, Madden LC, Simmons PA. Effectiveness of dry eye therapy under conditions of environmental stress. Curr Eye Res. 2013; 38:229–236.

16. Li DQ, Chen Z, Song XJ, Luo L, Pflugfelder SC. Stimulation of matrix metalloproteinases by hyperosmolarity via a JNK pathway in human corneal epithelial cells. Invest Ophthalmol Vis Sci. 2004; 45:4302–4311.

18. Lee KY, Rhim JW, Kang JH. Kawasaki disease: laboratory findings and an immunopathogenesis on the premise of a "protein homeostasis system". Yonsei Med J. 2012; 53:262–275.

19. Farris RL. Tear osmolarity--a new gold standard? Adv Exp Med Biol. 1994; 350:495–503.
20. Liacini A, Sylvester J, Li WQ, Zafarullah M. Inhibition of interleukin-1-stimulated MAP kinases, activating protein-1 (AP-1) and nuclear factor kappa B (NF-kappa B) transcription factors down-regulates matrix metalloproteinase gene expression in articular chondrocytes. Matrix Biol. 2002; 21:251–262.

21. Nguyen CQ, Yin H, Lee BH, Chiorini JA, Peck AB. IL17: potential therapeutic target in Sjögren's syndrome using adenovirus-mediated gene transfer. Lab Invest. 2011; 91:54–62.

22. Lagu B, Gerchak C, Pan M, Hou C, Singer M, Malaviya R, et al. Potent and selective CC-chemokine receptor-2 (CCR2) antagonists as a potential treatment for asthma. Bioorg Med Chem Lett. 2007; 17:4382–4386.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download