Abstract
Purpose
The purpose of our study was to investigate the effects of hippotherapy on gross motor function and functional performance in children with spastic cerebral palsy (CP).
Materials and Methods
We recruited 34 children (M:F=15:19, age: 3-12 years) with spastic CP who underwent hippotherapy for 45 minutes twice a week for 8 weeks. Twenty-one children with spastic CP were recruited for control group. The distribution of gross motor function classification system level and mean age were not significantly different between the two groups. Outcome measures, including the Gross Motor Function Measure (GMFM)-66, GMFM-88 and the Pediatric Evaluation of Disability Inventory: Functional Skills Scale (PEDI-FSS), were assessed before therapy and after the 8-weeks intervention as outcome measures.
Results
There were no significant differences between intervention and control groups in mean baseline total scores of GMFM-66, GMFM-88 or PEDI-FSS. After the 8-weeks intervention, mean GMFM-66 and GMFM-88 scores were significantly improved in both groups. However, the hippotherapy group had significantly greater improvement in dimension E and GMFM-66 total score than the control group. The total PEDI-FSS score and the sub-scores of its 3 domains were significantly improved in the hippotherapy group, but not in the control group.
Conclusion
The results of our study demonstrate the beneficial effects of hippotherapy on gross motor function and functional performance in children with CP compared to control group. The significant improvement in PEDI-FSS scores suggests that hippotherapy may be useful to maximize the functional performance of children with CP.
Cerebral palsy (CP) refers to a group of permanent motor disorders attributed to a non-progressive lesion that occurs in the immature brain.1 Children with CP have various degrees of impairment of movement and posture, which can limit physical activity and participation in daily life.2,3
Two types of horseback riding therapy are widely available: hippotherapy and therapeutic horseback riding (THR). In hippotherapy, a physical or occupational therapist controls the horse to influence the child's posture, balance, coordination, strength and sensorimotor systems while the child interacts with the horse and responds to the movement of the horse.4,5,6 In contrast, THR is led by a trained riding instructor with the child actively controlling the horse as a form of exercise to improve coordination, balance and posture, and to encourage development of sensory and perceptual motor skills.5,7,8 Although there are some differences between hippotherapy and THR, their therapeutic goals are essentially the same for children with CP. The warmth and shape of the horse and the rhythmic, three-dimensional movement of horseback riding are believed to improve the flexibility, posture, balance and mobility of the rider.
The potential for horseback riding therapy to promote gross motor function in children with CP has been investigated previously with mixed results. Some reports demonstrated the benefits of horseback riding therapy on reducing abnormal tone, promoting motor performance, creating symmetric alignment and improving postural awareness, gait and mobility.9,10,11,12 However, other reports found no significant effects of horseback riding therapy.10,13,14,15 This discrepancy of results may be due to differences in study design, participant characteristics and functional level, sample size, and intensity and duration of therapy given. Most studies on this subject had small sample sizes, ranging from 3 to 17 cases without control groups for comparison.5 There are, however, two randomized controlled trials with 72 participants and 19 participants, respectively. However, both found no significant benefits of horseback riding therapy for children with CP.10,13 A published meta-analysis concluded that there was insufficient evidence to support the benefits of horseback riding therapy on gross motor function.16
Despite this lack of consistent evidence on the benefit, horseback riding therapy is often recommended by clinicians for children with CP to improve gross motor function. Further evidence is required to support this practice. In addition, the ultimate therapeutic goal for children with CP is to enhance functional performance in daily life. However, the effects of horseback riding therapy on functional performance in particular have rarely been studied. Therefore, the aim of this study is to evaluate the effects of additional hippotherapy on gross motor function and functional performance in daily life of children with CP.
Children with spastic CP who met the inclusion and exclusion criteria were recruited for this study. The inclusion criteria were as follows: 1) age 3 to 12 years, 2) body weight less than 40 kg, and 3) gross motor function classification system (GMFCS) level I to IV. The exclusion criteria were as follows: 1) chemodenervation therapy in the previous 6 months, 2) selective dorsal rhizotomy within the past year, 3) moderate to severe intellectual disability, 4) uncontrolled seizure, 5) poor visual or hearing acuity, and 6) previous participation in hippotherapy or THR.
We asked the parents of the recruited children who met inclusion and exclusion criteria whether they desired hippotherapy for their children and could feasibly attend riding sessions. The parents of 45 children agreed to participate. During this study, 5 children dropped out for various reasons, such as acute illness or injury unrelated to hippotherapy. Another 6 children did not complete the Gross Motor Function Measure (GMFM) assessment after hippotherapy. Thus, data from a total of 34 children (15 boys and 19 girls) were used to investigate the effects of hippotherapy.
As controls, we recruited 21 children with CP who were waiting to begin hippotherapy or whose parents could not attend hippotherapy for various reasons such as scheduling problems. The children in both experimental and control groups had been attending a 30-minute session of outpatient physical and occupational therapy once a week. This study was approved by the Institutional Review Board and Ethics Committee of Severance Hospital (#4-2010-0069).
Sample size was selected on the basis of a previous report by Sterba, et al.,17 which demonstrated significant gains in GMFM scores after horseback riding therapy in children with CP. A sample size of 13 would achieve 80% power to detect a difference of 8.6 with a known standard deviation of 11 and with a significance level (α) of 0.05 using a two-sided one-sample t-test. Assuming a 20% loss to follow-up, at least 19 children were needed for each group.
The GMFM and the Pediatric Evaluation of Disability Inventory-Functional Skills Scale (PEDI-FSS) were selected as outcome measures because both are commonly used in children with CP18 and meet the criteria for reliability and validity with respect to responsiveness to change.19 The GMFM assesses the capacity of the International Classification of Function (ICF), while the PEDI-FSS measures performance in functional activities of daily life. When used together, the GMFM and PEDI provide a comprehensive picture of a child's functional abilities at the ICF activities level.19
The GMFM is a tool used to measure the child's capacity for gross motor function. Capacity refers to a person's underlying ability to perform in a standardized environment.20 It has been widely used to measure changes in gross motor function over time and the effectiveness of interventions. Items on the GMFM-88 are grouped into five dimensions: A: lying and rolling (17 items); B: sitting (20 items); C: crawling and kneeling (14 items); D: standing (13 items); and E: walking, running and jumping (24 items). The GMFM-66 was developed using Rasch analysis of the GMFM-88, whereby 22 of the original 88 items were deleted to improve reliability and validity.21 Of the 22 items deleted, 13 were from the lying and rolling dimension, 5 were from the sitting dimension and 4 were from the kneeling and crawling dimension. The GMFM-66 represents the unidimensional construct of gross motor ability according to task difficulty and thus is recommended for research purposes when comparing changes in gross motor function over time in children with CP.22 However, the GMFM-66 is much less useful when scoring children with a severe disability.23 Therefore, both the GMFM-66 and GMFM-88 were used to assess gross motor function in this study.
The PEDI is an internationally recognized, validated parental report measure used for assessing a child's capability and performance in daily life. Capability describes what a person potentially can do, whereas performance describes what a person actually does in their environment.20 Capability is measured by identifying mastery of functional skills in three domains: self-care, mobility and social functioning. Performance is measured by parental reports of whether the child is capable of performing each of 197 tasks in these 3 domains in daily environments, such as home and kindergarten or school.18 In this study, we used only the PEDI-FSS to measure the child's actual performance in those three domains. The PEDI-FSS evaluation was performed by trained occupational therapists through a structured interview with the parent or caregiver. All items were checked as either capable (score 1) or unable (score 0). No items were left blank. Both the GMFM and PEDI-FSS were assessed within the week before and again within 2 months after completion of the 8-week intervention in both groups.
On review of the literature, hippotherapy intervention protocols vary between studies in intensity and duration. In the studies cited, session length ranged from 30 minutes to 1 hour with a frequency ranging from 1-2 sessions per week and the total duration of horseback riding ranged widely from 8 min and 26 hours. According to a recent systematic review, a weekly 45-min session of either THR or hippotherapy for 8-10 weeks was correlated with positive effects on gross motor function in children with CP.5 Given these results, we administered 45-minutes sessions twice per week for 8 weeks in this study.
Hippotherapy was performed at the riding center in Seoul Race Park of the Korea Racing Authority. The sessions were conducted by a trained occupational therapist accredited by the American Hippotherapy Association while the horse was led by a trained assistant. A volunteer walked along either side of the horse to assist the child. The therapist followed target objectives aimed to develop the child's sensorimotor and perceptual-motor skills. The child was seated astride the horse wearing a helmet and was encouraged to perform various activities designed to emphasize movement in a forward and upward reaching direction to encourage active postural control, trunk strength, balance and trunk/pelvic dissociation.
Statistical analysis was performed using SPSS 19.0 for Windows (SPSS Inc., Chicago, IL, USA). The independent t-test was used to compare the difference in mean age between groups. The chi-squared test was used to compare the differences in distributions of GMFCS level and age between groups. Paired and independent t-tests were used to assess differences within and between groups, respectively. A p-value less than 0.05 was considered statistically significant.
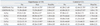
Patient characteristics are summarized in Table 1. Of the 34 children in the intervention group, 32 had bilateral spastic CP and 2 had unilateral CP. There was no significant difference in mean age, distribution, or GMFCS level between groups. Young children aged 3 to 7 years comprised 22 individuals in the hippotherapy group and 10 in the control group. The proportion of younger or older children was not significantly different between groups.
At the initial baseline evaluation, there were no significant differences in total GMFM-66 or GMFM-88 score between hippotherapy and control groups. However, GMFM-88 scores in the B and C dimensions were significantly higher in the hippotherapy group than the control group. After the 8-week intervention, both GMFM-66 and GMFM-88 scores were significantly improved in both groups. The improvements in GMFM-66 scores were significantly greater in the hippotherapy group than in the control group. GMFM-88 scores were significantly improved in all dimensions in the hippotherapy group, but only in dimension B in the control group. Changes in dimension E of the GMFM-88 over the course of the study were significantly greater in the hippotherapy group than in the control group (Table 2).
PEDI-FSS evaluations were missing in 6 children in the hippotherapy group because their parents could not be interviewed for various reasons. Thus, PEDI-FSS was assessed in 28 children in the hippotherapy group and 21 in the control group. At the initial baseline evaluation, there were no significant differences in total score or sub-scores of any domain between groups. After the 8-week intervention, significant improvements in the total score and the sub-scores of all 3 domains were achieved in the hippotherapy group, but not in the control group. In addition, changes in the total score and sub-scores of all 3 domains after the 8-week study period were significantly greater in the hippotherapy group than the control group (Table 3).
The GMFM is commonly used to measure changes in gross motor function as a result of horseback riding therapy. Previous studies have used the total or dimension scores of the GMFM-88 more often than the GMFM-66.11,13,14 Repeated measures analysis among participants demonstrated significant gains in GMFM-88 scores after horseback riding therapy in most published studies.11,17,24 In contrast, two randomized controlled trial (RCT) studies did not demonstrate any significant gains in the GMFM-88 or GMFM-66.10,13,14
In our study, significant gains in the GMFM-88 and GMFM-66 were demonstrated in both groups. In children with CP, the most rapid improvements in GMFM scores occur during the first 4 years of age, with children reaching a plateau between 5 and 6 years, depending on the severity of their disability.1 A proportion of children in each group were aged from 3 to 7 years, making it possible that gains were naturally occurring. In the present study, however, the significantly greater gains in GMFM-66 score and dimension E of GMFM-88 in the hippotherapy group suggest the beneficial effects of hippotherapy on gross motor function.
Of the previous studies showing significant gains in the GMFM, 3 studies reported significant improvement only in dimension E17,24,25 and one study reported significant gains in all dimensions except A.11 The dimension of GMFM improved by horseback riding therapy may vary according to the initial functional level of participants. To the best of our knowledge, only 5 reports have been published describing the GMFCS level of participants.13,14,15,17,25 Among those studies, the GMFM was used as an outcome measure in 3 studies.13,17,25 A RCT study in which all participants were at GMFCS level I to III13 did not find any significant improve-ments in the intervention group compared to controls. In contrast, a repeated measure within-participant study reported significant gains in total GMFM-88 and dimension E scores.17 In that study, 12 of the 17 participating children were GMFCS level I to III and only 5 were level IV to V. Another study in which all participants were GMFCS level I to II reported significant improvements in GMFM dimension E in the hippotherapy group, compared to control group.25 These cumulative data suggest that horseback riding therapy leads to improvements in dimension E of the GMFM, especially in higher functioning children.
Our study demonstrated significantly greater improvement in GMFM-66 and dimension E scores in the hippotherapy group and no significant difference in GMFM-88 scores gains between groups. The deletions from the GMFM-88 to create the GMFM-66 (13 items from dimension A, 5 items from dimension B and 4 items from dimension C) may have influenced the greater gain observed in GMFM-88 dimension E and GMFM-66 in the hippotherapy group. Our findings are consistent with the hypothesis that hippotherapy is more beneficial in higher-functioning children with CP. Unfortunately, however, the sample size of our study was too small to divide into groups according to GMFCS level, thus preventing us from analyzing changes in the GMFM according to functional level. Further study is warranted with larger sample sizes to explore changes in gross motor function according to GMFCS level.
The PEDI-FSS has been widely used to evaluate the daily functional performance of children with CP.18 The PEDI is intended for children up to 7.5 years of age, but this can be extended to children with functional disabilities.26 In our study, the PEDI-FSS was used to measure the actual performance in daily life of children older than 7.5 years. On review of the literature, the PEDI was used as an outcome measure in only one study by Casady and Nichols-Larsen.11 In that study, significant improvement was found in the total PEDI score as well as its 3 domains of self-care, mobility and social functioning. However, the small sample size (n=10), lack of a control group and large variability in the frequency of physical, occupational and speech therapy (none-10 weeks) limits the applicability of these results.
Our study demonstrated significant improvements in all 3 PEDI domains of self-care, mobility and social functioning in the hippotherapy group, but not in the control group. These findings suggest some positive effects of hippotherapy on the child's actual performance in daily life. The mobility domain is closely related to gross motor function based on GMFCS level,27 while the self-care domain is related to both GMFCS level and hand function based on Manual Ability Classification System score.28 According to a previous report, hippotherapy improved dynamic trunk stability and functional reach in children with spastic diplegia.12 Those beneficial effects of hippotherapy seem likely to contribute the significant gains of self-care and mobility domains in our study.
The social functioning domain is influenced by various factors such as education, socioeconomic status, cognition, communication abilities and motor function.27 The opportunity to use or practice communication, listening and language skills during hippotherapy may have resulted in the improvements observed in PEDI social functioning, in line with Casady and Nichols-Larsen's11 report.
On the other hand, actual performance in daily life is influenced not only by physical environment, but also by personal and social factors.20,29 The significant PEDI gains suggest that hippotherapy enhances the child's motivation and willingness for participation in an activity.11
Although functional level may affect the gross motor outcome after hippotherapy, our sample size was insufficient to group children according to GMFCS level. This stratification would be important to select children who would benefit most from the therapy. In addition, the benefits of hippotherapy on the GMFM observed in our study were modest. This may be due to the wide range of functional disability levels of the participants.
Although there was no significant difference in mean age between groups, nor in the ratio of younger to older children between groups, the proportion of children aged from 3 to 7 years was slightly higher in the hippotherapy group, which may have biased the results. Age likely affects gross motor improvements, as young children may have greater potential for improvement. Further study is needed to examine the effect of age on positive gains in hippotherapy.
Another limitation of our study is that we did not control extraneous therapeutic interventions except physical and occupational therapy. We also did not control for socioeconomic status, cognition or communication level. Each of these factors could affect PEDI scores. Further research is needed to ascertain the effect of hippotherapy on PEDI scores.
In conclusion, hippotherapy has become a popular modality for children with CP that is believed to enhance gross motor function, although there is insufficient evidence to support its benefits. This study has demonstrated modest but significant benefits in gross motor function over physical and occupational therapy, indicating that its clinical application in this area may be limited. The relatively greater improvements in PEDI scores observed suggest that hippotherapy helps children to engage more meaningfully in the functional activities of daily life. Investigation is warranted into the effects of hippotherapy on the child's self-confidence, motivation and other emotional areas. Further studies to determine who would benefit most from hippotherapy would be useful to expand the use of hippotherapy as a therapeutic intervention to maximize gross motor function and functional performance in children with CP.
References
1. Rosenbaum P, Paneth N, Leviton A, Goldstein M, Bax M, Damiano D, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007; 109:8–14.
2. Beckung E, Carlsson G, Carlsdotter S, Uvebrant P. The natural history of gross motor development in children with cerebral palsy aged 1 to 15 years. Dev Med Child Neurol. 2007; 49:751–756.

3. Wright FV, Rosenbaum PL, Goldsmith CH, Law M, Fehlings DL. How do changes in body functions and structures, activity, and participation relate in children with cerebral palsy? Dev Med Child Neurol. 2008; 50:283–289.

4. Debuse D, Gibb C, Chandler C. Effects of hippotherapy on people with cerebral palsy from the users' perspective: a qualitative study. Physiother Theory Pract. 2009; 25:174–192.

5. Whalen CN, Case-Smith J. Therapeutic effects of horseback riding therapy on gross motor function in children with cerebral palsy: a systematic review. Phys Occup Ther Pediatr. 2012; 32:229–242.

7. Snider L, Korner-Bitensky N, Kammann C, Warner S, Saleh M. Horseback riding as therapy for children with cerebral palsy: is there evidence of its effectiveness? Phys Occup Ther Pediatr. 2007; 27:5–23.
8. Sterba JA. Does horseback riding therapy or therapist-directed hippotherapy rehabilitate children with cerebral palsy? Dev Med Child Neurol. 2007; 49:68–73.

9. Bertoti DB. Effect of therapeutic horseback riding on posture in children with cerebral palsy. Phys Ther. 1988; 68:1505–1512.
10. Mackinnon JR, Noh S, Lariviere J, Macphail A, Allan DE, Laliberte D. A study of therapeutic effects of horseback riding for children with cerebral palsy. Phys Occup Ther Pediatr. 1995; 15:17–34.

11. Casady RL, Nichols-Larsen DS. The effect of hippotherapy on ten children with cerebral palsy. Pediatr Phys Ther. 2004; 16:165–172.

12. Shurtleff TL, Standeven JW, Engsberg JR. Changes in dynamic trunk/head stability and functional reach after hippotherapy. Arch Phys Med Rehabil. 2009; 90:1185–1195.

13. Davis E, Davies B, Wolfe R, Raadsveld R, Heine B, Thomason P, et al. A randomized controlled trial of the impact of therapeutic horse riding on the quality of life, health, and function of children with cerebral palsy. Dev Med Child Neurol. 2009; 51:111–119.

14. Hamill D, Washington KA, White OR. The effect of hippotherapy on postural control in sitting for children with cerebral palsy. Phys Occup Ther Pediatr. 2007; 27:23–42.

15. McGee MC, Reese NB. Immediate effects of a hippotherapy session on gait parameters in children with spastic cerebral palsy. Pediatr Phys Ther. 2009; 21:212–218.

16. Tseng SH, Chen HC, Tam KW. Systematic review and meta-analysis of the effect of equine assisted activities and therapies on gross motor outcome in children with cerebral palsy. Disabil Rehabil. 2013; 35:89–99.

17. Sterba JA, Rogers BT, France AP, Vokes DA. Horseback riding in children with cerebral palsy: effect on gross motor function. Dev Med Child Neurol. 2002; 44:301–308.

18. Steenbeek D, Gorter JW, Ketelaar M, Galama K, Lindeman E. Responsiveness of Goal Attainment Scaling in comparison to two standardized measures in outcome evaluation of children with cerebral palsy. Clin Rehabil. 2011; 25:1128–1139.

19. Ketelaar M, Vermeer A, Helders PJ. Functional motor abilities of children with cerebral palsy: a systematic literature review of assessment measures. Clin Rehabil. 1998; 12:369–380.

20. Smits DW, Gorter JW, Ketelaar M, Van Schie PE, Dallmeijer AJ, Lindeman E, et al. Relationship between gross motor capacity and daily-life mobility in children with cerebral palsy. Dev Med Child Neurol. 2010; 52:e60–e66.

21. Lundkvist Josenby A, Jarnlo GB, Gummesson C, Nordmark E. Longitudinal construct validity of the GMFM-88 total score and goal total score and the GMFM-66 score in a 5-year follow-up study. Phys Ther. 2009; 89:342–350.

22. Russell DJ, Avery LM, Rosenbaum PL, Raina PS, Walter SD, Palisano RJ. Improved scaling of the gross motor function measure for children with cerebral palsy: evidence of reliability and validity. Phys Ther. 2000; 80:873–885.

23. Alotaibi M, Long T, Kennedy E, Bavishi S. The efficacy of GMFM-88 and GMFM-66 to detect changes in gross motor function in children with cerebral palsy (CP): a literature review. Disabil Rehabil. 2014; 36:617–627.

24. McGibbon NH, Andrade CK, Widener G, Cintas HL. Effect of an equine-movement therapy program on gait, energy expenditure, and motor function in children with spastic cerebral palsy: a pilot study. Dev Med Child Neurol. 1998; 40:754–762.

25. Kwon JY, Chang HJ, Lee JY, Ha Y, Lee PK, Kim YH. Effects of hippotherapy on gait parameters in children with bilateral spastic cerebral palsy. Arch Phys Med Rehabil. 2011; 92:774–779.

26. James S, Ziviani J, Boyd R. A systematic review of activities of daily living measures for children and adolescents with cerebral palsy. Dev Med Child Neurol. 2014; 56:233–244.

27. Kwon TG, Yi SH, Kim TW, Chang HJ, Kwon JY. Relationship between gross motor function and daily functional skill in children with cerebral palsy. Ann Rehabil Med. 2013; 37:41–49.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download