Abstract
Purpose
To investigate chemosensitivity with an adenosine triphosphate-based chemotherapy response assay in patients with epithelial ovarian or peritoneal cancer according to tumor histology, grade, and disease status.
Materials and Methods
One hundred specimens were collected during primary or secondary debulking from 67 patients with primary ovarian cancer, 24 patients with recurrent ovarian cancer, 5 patients with primary peritoneal cancer, and 4 patients with recurrent peritoneal cancer; samples were collected between August 2006 and June 2009. Tumor cells were isolated and cultured for 48 hours in media containing chemotherapy. The chemosensitivity index (CI) was calculated as 300 minus the sum of the cell death rate at 0.2×, 1×, and 5× drug concentrations, and the CI values were compared.
Results
CI values were obtained from 93 of 100 patients. The most active agents against primary disease were ifosfamide and paclitaxel. For primary serous adenocarcinoma, paclitaxel and irinotecan were the most active, followed by ifosfamide. For clear cell carcinoma, ifosfamide was the most active, followed by paclitaxel and irinotecan. Although not statistically significant, the CIs of cisplatin, carboplatin, paclitaxel, and docetaxel decreased as tumor grade increased. In 14 cases of recurrent disease, paclitaxel was the most active, followed by ifosfamide and cisplatin.
The chemosensitivity test is an in vitro predictive assay for assessing the sensitivity of cancer cells to various chemotherapeutic agents. Since the development of the human tumor stem cell assay by Hamburger and Salmon in the 1970s, various chemosensitivity assays have been created to predict chemotherapy response. These assays include titrated thymidine incorporation, fluorescent cytoprint, the 5-diphenyltetrazolium bromide assay, and the differential staining cytotoxicity assay.1,2,3,4,5 The adenosine triphosphate (ATP)-based chemotherapy response assay (ATP-CRA) is a sensitive assay that evaluates tumor cell viability by measuring the intracellular ATP levels of drug-exposed cells and untreated controls. The ATP-based chemosensitivity test is reported to have many advantages, such as feasibility, reproducibility, low cost, small patient sample requirement, and high positive and negative predictive values.6,7,8 The recently developed ATP-CRA adopted new methods, including the use of ultra-low attachment culture plates, to inhibit the growth of normal cells and reduce the turnaround time of the test. The ATP-CRA has a high success rate in primary culture and requires only a small number of cells. In addition, ATP-CRA results correlate well with clinical outcomes in patients with breast or lung cancer.9,10 Furthermore, Han, et al.11 report that the ATP-CRA has a high sensitivity and a positive predictive value, accurately predicting response to chemotherapy in ovarian cancer.
The purpose of this study was to investigate chemosensitivity in epithelial ovarian or peritoneal cancer tissues using the ATP-CRA according to tumor histology, grade, and disease status. We selected 10 chemotherapeutic agents, including one alkylating agent (ifosfamide), three platinum analogues (cisplatin, carboplatin, and oxaliplatin), two taxanes (paclitaxel and docetaxel), three camptothecin analogues (topotecan, irinotecan, and belotecan), and gemcitabine. We measured the chemosensitivity index (CI) of these agents in cancer tissues using the ATP-CRA. The CI and CI rank were compared according to histological type, tumor grade, and disease status.
One hundred fresh, sterile tumor specimens were collected during primary or secondary debulking from 67 patients with primary ovarian cancer, 24 patients with recurrent ovarian cancer, 5 patients with primary peritoneal cancer, and 4 patients with recurrent peritoneal cancer. Samples were obtained according to the guidelines of the Institutional Review Board of Yonsei University College of Medicine, Seoul, Korea, between August 2006 and June 2009. All tumor specimens for the ATP-CRA were removed as part of the normal treatment procedure. The histological types of tumor tissues and qualitative and quantitative analyses of cancer cells were evaluated by pathologists.
The ATP-CRA was performed as described previously.10,12 Briefly, fresh tumor specimens were obtained during surgery and transferred to HBSS (Gibco BRL, Rockville, MD, USA) transport media. Cell suspensions were prepared enzymatically by incubating with dispase (Sigma, St. Louis, MO, USA), pronase (Sigma), and DNase (Sigma) at 37℃ for 12-16 hours. Isolated cells were separated from tissue fragments by passing through a cell strainer (BD Falcon, Bedford, MA, USA). Tumor cells were purified using Ficoll (1.077 g/mL) density gradient centrifugation to remove red blood cells, dead cells, and residual cell debris. If a sufficient amount of cells was isolated, blood-derived normal cells were removed using anti-CD45 antibody-conjugated magnetic beads (Miltenyi Biotech, Auburn, CA, USA).13 The final tumor cell preparation was suspended in Iscove's Modified Dulbecco's Media (IMDM; Gibco BRL) containing 10% fetal bovine serum (FBS). Separated tumor cells were diluted to 2000-20000 viable cells per 100 µL using IMDM containing 10% FBS. Cells were seeded in triplicate in a 96-well ultra-low attachment microplate (Costar, Cambridge, MA, USA), which restricted the growth of normal cells, such as fibroblasts. For treatment groups, 100 µL of chemotherapeutic agent was added to cells and cultured for 48 hours in a 5% CO2 incubator. In the control groups, 100 µL of IMDM was added to 3-6 wells without chemotherapeutic agents. For quality control purposes, a negative control group of 3-6 wells with seeding media only (no cells) and two positive control groups were included in the culture plate. Each positive control group was composed of three wells that contained minimal (105 pg ATP) or median (280 pg ATP) amounts of ATP, as determined from 1000 tumor cells harvested from tumor tissues. Treated drug concentrations (TDC) were derived from preliminary experiments, which exhibited a scattered distribution of cell death for each specimen.14,15 Drugs were used in triplicate at three concentrations (0.2×, 1×, and 5× TDC). The 1× TDCs were belotecan, 0.11 µg/mL; carboplatin, 12 µg/mL; cisplatin, 2.5 µg/mL; docetaxel, 3.7 µg/mL; irinotecan, 4.7 µg/mL; gemcitabine, 16.9 µg/mL; oxaliplatin, 2.9 µg/mL; paclitaxel, 8.5 µg/mL; ifosfamide, 0.4 µg/mL; and topotecan, 0.0325 µg/mL. Because ifosfamide requires in vivo hepatic activation, we used the active metabolite 4-hydroxy ifosfamide (NIOMECH, Bielefeld, Germany). The untreated control group consisted of primary culture cells from each patient that were cultured without chemotherapeutic agents, while the treated group consisted of primary culture cells cultured with each chemotherapeutic agent. At the end of the incubation, the cells were exposed to reagents to measure ATP content according to the manufacturer's instructions (ATP Bioluminescence assay kit HS II, Roche, Mannheim, Germany). The ATP content of each well was quantified according to the amount of ATP-dependent light emitted using the Victor 3 multi-label counter (PerkinElmer, Boston, MA, USA). Raw data in Excel was analyzed with Report Maker version 1.1 (ISU ABXIS, Seoul, Korea). Briefly, the cell death rate (CDR) for each drug was calculated as follows: CDR (%)=[1-(mean luminescence in treated group/mean luminescence in untreated control group)]×100. We also calculated the CI as the sum of the percentage cell death for all concentrations tested 300-sum of % inhibition at 0.2×, 1×, and 5× TDC. The CI rank of the 10 anticancer drugs in each cancer tissue was determined according to the CI. To calculate the intra-assay mean coefficient of variation (CV), luminescence values of each specimen were measured 3-6 times in both negative and positive control groups. We determined whether the measured values at 280 pg of ATP were higher than those at 105 pg of ATP. If microorganism contamination or an inadequate number of cells was discovered, or if the intra-assay mean CV exceeded 30, the test was considered a failure. If measured values in the untreated control group were lower than those in the positive group (105 pg of ATP), the specimen was considered to have unacceptable viability.
The data were analyzed using parametric and nonparametric statistics with SPSS 12.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used for quantitative experimental data. The Mann-Whitney U test was performed for comparisons of CIs in primary and recurrent disease. Comparison of CI according to histological grade was performed with the Kruskal-Wallis test.
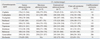
Patient characteristics are summarized in Table 1. The median age was 52 years (range, 22-71 years). There were 72 patients with primary epithelial ovarian or peritoneal cancer and 28 patients with recurrent cancers. Serous adenocarcinoma was the most common (67.0%), followed by mucinous (9.0%) and endometrioid (9.0%) adenocarcinomas. Clear cell carcinoma represented 4.0% of cases. Stage III disease was present in 44 of 67 patients (65.7%), and stage I was in 13 of 67 (19.4%). Stage II and IV disease was in 5 of 67 (7.5%) and 5 of 67 (7.5%), respectively. The median intra-assay mean CV was 5.45 (range: 2.5 periton one primary ovarian cancer tissue failed to obtain an acceptable CV in 1× concentration, and four primary and three recurrent cancer tissues produced insufficient cells at all concentrations; thus, the CI values were obtained from 67 primary and 25 recurrent cases.
The CI according to histological type is shown in Table 2. The CI of the three platinum analogues (cisplatin, carboplatin, and oxaliplatin) did not show statistically significant differences among the serous, mucinous, and endometrioid adenocarcinoma groups. However, these three platinum analogues showed decreased CI values with marginal statistical significance in clear cell carcinoma compared with those of serous adenocarcinoma, especially cisplatin (median CI; clear cell: 145; serous: 176; p=0.052) and carboplatin (median CI; clear cell: 178; serous: 204; p=0.076). These results indicate that, at least in vitro, cisplatin and carboplatin may be more active against clear cell carcinoma than serous adenocarcinoma. Two taxanes (paclitaxel and docetaxel), three camptothecin analogues (topotecan, irinotecan, and belotecan), and gemcitabine showed no significant differences among histological types, with the exception of docetaxel in endometrioid adenocarcinoma. Docetaxel showed an increased CI in endometrioid carcinoma compared to that in serous adenocarcinoma (median CI; endometrioid: 215; serous: 171; p=0.034). The CIs of topotecan (median CI; clear cell: 148; serous: 185; p=0.070) and ifosfamide (median CI; clear cell: 122; serous: 174; p=0.074) were lower in clear cell carcinoma compared with those in serous adenocarcinoma with marginal statistical significance.
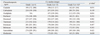
In primary serous adenocarcinoma, ifosfamide was the most active drug, followed by paclitaxel, irinotecan, and cisplatin. Furthermore, ifosfamide was the most active drug in mucinous adenocarcinoma, followed by paclitaxel. However, in endometrioid adenocarcinoma, irinotecan was the most active drug, followed by cisplatin and paclitaxel. In clear cell carcinoma, cisplatin and ifosfamide were the most active drugs, followed by docetaxel and paclitaxel. For most anticancer drugs, the CIs in clear cell carcinoma and undifferentiated carcinoma were not higher than that of serous adenocarcinoma. The CI values for cisplatin, carboplatin, paclitaxel, and docetaxel, which are the most commonly used anticancer drugs for primary epithelial ovarian cancer, were not higher in clear cell carcinoma compared to serous adenocarcinoma. The CI according to tumor grade is shown in Table 3. Although not statistically significant, the CIs of cisplatin, carboplatin, and paclitaxel decreased as tumor grade increased. However, oxaliplatin showed an increased CI as tumor grade increased (p=0.072). The CI of each chemotherapeutic agent in primary or recurrent disease is shown in Table 4 and Supplementary Fig. 1(only online). In recurrent disease, the CI (especially of cisplatin, carboplatin, topotecan, irinotecan, and belotecan) was higher compared to that of primary disease. The CI rank of each anticancer drug in primary or recurrent disease is shown in Table 4. In primary disease, ifosfamide ranked first, followed by paclitaxel and irinotecan. In recurrent disease, paclitaxel ranked first, followed by ifosfamide and cisplatin.
Increased CIs in recurrent disease were found for two platinum analogues, cisplatin (median CI; primary: 174; recurrent: 220; p=0.001) and carboplatin (median CI; primary: 201; recurrent: 241; p=0.001). The CI rank of carboplatin was lower in recurrent disease (median CI rank; primary: 7; recurrent: 8; p=0.010), but the CI rank of cisplatin was the same in primary and recurrent disease (median CI rank; primary: 4; recurrent: 4), as shown in Table 3. The median CI values of oxaliplatin in primary and recurrent disease were 189 and 200, respectively (p=0.117). In addition to the increase seen in recurrent disease, the CI rank of oxaliplatin was higher for recurrent disease (median CI rank: 6) compared to that of primary disease (median CI rank: 7).
The median CI values of 2 taxanes (paclitaxel and docetaxel) were similar in primary and recurrent disease for both paclitaxel (primary: 168; recurrent: 176; p=0.318) and docetaxel (primary: 190; recurrent: 189; p=0.522). The CI rank of paclitaxel was higher in recurrent disease, but the difference was not statistically significant (median CI rank; primary: 3; recurrent: 2; p=0.491). The CI rank of docetaxel did not change in recurrent disease (median CI rank; primary: 5; recurrent: 5).
Three camptothecin analogues (topotecan, irinotecan, and belotecan) showed decreased CI values in recurrent disease. The median CI value in primary or recurrent disease for topotecan was 185 and 215, respectively (p=0.049); for irinotecan, 171 and 217 (p=0.001); and for belotecan, 183 and 248 (p=0.008). The median CI rank of topotecan in primary and recurrent disease was the same, but irinotecan and belotecan had lower CI ranks in recurrent disease (5 and 6, respectively) compared to those of primary disease (3 and 5, respectively) (Fig. 1). The median CI of ifosfamide in primary and recurrent disease was 165 and 173, respectively (p=0.221). The median CI rank of ifosfamide in primary and recurrent disease was 2 and 3, respectively.
The current study examined the CI and CI ranks of 10 chemotherapeutic agents that are used in the treatment of ovarian and peritoneal cancers. This study showed a trend toward an increased CI in recurrent disease compared with those in primary disease for most anticancer drugs. These results suggest that recurrent disease is more resistant to most chemotherapeutic agents than primary disease. In particular, two commonly used platinum analogues (cisplatin and carboplatin) showed statistically significant increases in CI in recurrent disease. The CI rank of carboplatin was reduced in recurrent cases, indicating that recurrent disease becomes more resistant to carboplatin than to other chemotherapeutic agents. This might be due to previous exposure of patients to platinum agents. In contrast to the platinum agents, two taxanes (paclitaxel and docetaxel), which are also commonly used for primary ovarian cancer, did not show significant increases in CI in recurrent disease. Furthermore, the CI ranks of paclitaxel and docetaxel did not change in recurrent disease, suggesting that taxanes may be effective for recurrent and primary disease.
The newly developed oxaliplatin showed a slightly decreased CI in recurrent disease; however, the CI rank increased in recurrent disease compared with that of other chemotherapeutic agents.
Three camptothecin analogues, as well as irinotecan and belotecan, showed decreased chemosensitivity in recurrent disease. In addition, the median CI ranks of irinotecan and belotecan were lower in recurrent disease compared with that of other chemotherapeutic agents. These results suggest that irinotecan and belotecan may be less effective than other chemotherapeutic agents for recurrent disease.
Ifosfamide maintained a high CI rank (median CI rank: 3) in recurrent disease, and the CI also increased slightly.
Among 10 chemotherapeutic agents, the most effective drugs in primary disease were ifosfamide and paclitaxel, followed by cisplatin and irinotecan. These results strongly suggest that ifosfamide could be a first-line combination chemotherapeutic agent for primary disease. Although paclitaxel and platinum combination chemotherapy has been used in patients with primary ovarian or peritoneal cancer, the addition of ifosfamide may be more effective for primary disease. Several reports support the combination of ifosfamide with paclitaxel and platinum as a primary chemotherapeutic regimen in ovarian cancer.16,17,18 Fruscio, et al.17 reported the feasibility and efficacy of ifosfamide and epirubicin in combination with first-line chemotherapy containing cisplatin and paclitaxel. In this study, patients with histologically proven epithelial ovarian cancer were randomly assigned to receive first-line polychemotherapy with cisplatin, paclitaxel, and epirubicin or paclitaxel, ifosfamide, and cisplatin (TIP) for 6 cycles every 21 days. Although more than 50% of patients were suboptimally debulked after the first surgery, the median overall survival with TIP was 51 months, and 5-year survival rates were 43%. This report supports the use of ifosfamide with the combination of paclitaxel and platinum in patients with primary ovarian cancer.
In recurrent disease, the most effective drug was paclitaxel, followed by ifosfamide, cisplatin, and topotecan. These results suggest that paclitaxel might be the most effective drug for recurrent disease, and ifosfamide may be an effective second-line chemotherapeutic agent for recurrent disease. As a result, the TIP regimen may be considered a second-line option for platinum-sensitive recurrent disease. Polyzos, et al.19 reported the activity and toxicity of a paclitaxel-ifosfamide-cisplatin combination (paclitaxel 175 mg/m2 as a 3-hour IV on day 1, cisplatin 75 mg/m2 IV over 2 hours fractionated over days 1 and 2, and ifosfamide 5 mg/m2 IV over 1 hour fractionated on days 1-2 with mesna uroprotection, every 3 weeks) in 35 patients with ovarian cancer previously treated with platinum compounds and paclitaxel. In this report, three drug combinations demonstrated significant efficacy against potentially platinum-sensitive tumors and moderate efficacy in platinum-resistant tumors with tolerable myelotoxicity levels.
In the current study, clear cell carcinoma and undifferentiated carcinoma, which usually have poor prognosis, demonstrated no difference in CI values. These histological types showed increased chemosensitivity. Furthermore, high-grade disease demonstrated increased sensitivity to most chemotherapeutic agents. These results were the opposite of our expectation, which was that tumors with poor prognostic histological types and grades would be more resistant to chemotherapeutic agents.
In conclusion, our study demonstrated that primary or recurrent ovarian and peritoneal cancer tissues were the most sensitive to ifosfamide and paclitaxel. Although this was an in vitro study, the results suggest that an ifosfamide-containing combination may be beneficial as a first-line chemotherapy regimen for primary and recurrent disease. Therefore, we recommend a TIP combination chemotherapy regimen for recurrent and primary disease.
Figures and Tables
Fig. 1
Box-and-whisker plots of the CI rank of 10 chemotherapeutic agents in primary (A) and recurrent disease (B). The bottom and top edges of the box represent the 25th and 75th percentiles, respectively, whereas the horizontal line corresponds to the median value. The vertical lines show the range of values. The agents that were ranked with the first and second CI values in primary and recurrent disease were paclitaxel and ifosfamide. CI, chemosensitivity index.

ACKNOWLEDGEMENTS
This study was supported by the Brain Korea (BK) 21 Project for Medical Sciences, Yonsei University and a faculty research grant of Yonsei University College of Medicine in 2012 (6-2012-0073).
References
1. Cree IA, Kurbacher CM. Individualizing chemotherapy for solid tumors--is there any alternative? Anticancer Drugs. 1997; 8:541–548.
2. Kern DH, Drogemuller CR, Kennedy MC, Hildebrand-Zanki SU, Tanigawa N, Sondak VK. Development of a miniaturized, improved nucleic acid precursor incorporation assay for chemosensitivity testing of human solid tumors. Cancer Res. 1985; 45(11 Pt 1):5436–5441.
3. Bird MC, Bosanquet AG, Forskitt S, Gilby ED. Semi-micro adaptation of a 4-day differential staining cytotoxicity (DiSC) assay for determining the in-vitro chemosensitivity of haematological malignancies. Leuk Res. 1986; 10:445–449.

4. Pieters R, Loonen AH, Huismans DR, Broekema GJ, Dirven MW, Heyenbrok MW, et al. In vitro drug sensitivity of cells from children with leukemia using the MTT assay with improved culture conditions. Blood. 1990; 76:2327–2336.

6. Andreotti PE, Cree IA, Kurbacher CM, Hartmann DM, Linder D, Harel G, et al. Chemosensitivity testing of human tumors using a microplate adenosine triphosphate luminescence assay: clinical correlation for cisplatin resistance of ovarian carcinoma. Cancer Res. 1995; 55:5276–5282.
7. Sevin BU, Peng ZL, Perras JP, Ganjei P, Penalver M, Averette HE. Application of an ATP-bioluminescence assay in human tumor chemosensitivity testing. Gynecol Oncol. 1988; 31:191–204.

8. O'Meara AT, Sevin BU. Predictive value of the ATP chemosensitivity assay in epithelial ovarian cancer. Gynecol Oncol. 2001; 83:334–342.
9. Kim HA, Yom CK, Moon BI, Choe KJ, Sung SH, Han WS, et al. The use of an in vitro adenosine triphosphate-based chemotherapy response assay to predict chemotherapeutic response in breast cancer. Breast. 2008; 17:19–26.

10. Moon YW, Choi SH, Kim YT, Sohn JH, Chang J, Kim SK, et al. Adenosine triphosphate-based chemotherapy response assay (ATP-CRA)-guided platinum-based 2-drug chemotherapy for unresectable nonsmall-cell lung cancer. Cancer. 2007; 109:1829–1835.

11. Han SS, Choi SH, Lee YK, Kim JW, Park NH, Song YS, et al. Predictive value of individualized tumor response testing by ATP-based chemotherapy response assay in ovarian cancer. Cancer Invest. 2008; 26:426–430.

12. Kang SM, Park MS, Chang J, Kim SK, Kim H, Shin DH, et al. A feasibility study of adenosine triphosphate-based chemotherapy response assay (ATP-CRA) as a chemosensitivity test for lung cancer. Cancer Res Treat. 2005; 37:223–227.

13. Iinuma H, Okinaga K, Adachi M, Suda K, Sekine T, Sakagawa K, et al. Detection of tumor cells in blood using CD45 magnetic cell separation followed by nested mutant allele-specific amplification of p53 and K-ras genes in patients with colorectal cancer. Int J Cancer. 2000; 89:337–344.

14. Weisenthal LM, Dill PL, Finklestein JZ, Duarte TE, Baker JA, Moran EM. Laboratory detection of primary and acquired drug resistance in human lymphatic neoplasms. Cancer Treat Rep. 1986; 70:1283–1295.
15. Bird MC, Bosanquet AG, Gilby ED. In vitro determination of tumour chemosensitivity in haematological malignancies. Hematol Oncol. 1985; 3:1–10.

16. Zylberberg B, Dormont D, Madelenat P, Daraï E. First-line intraperitoneal cisplatin-paclitaxel and intravenous ifosfamide in Stage IIIc ovarian epithelial cancer. Eur J Gynaecol Oncol. 2004; 25:327–332.
17. Fruscio R, Colombo N, Lissoni AA, Garbi A, Fossati R, Ieda' N, et al. A phase II randomised clinical trial comparing cisplatin, paclitaxel and ifosfamide with cisplatin, paclitaxel and epirubicin in newly diagnosed advanced epithelial ovarian cancer: long-term survival analysis. Br J Cancer. 2008; 98:720–727.

18. Papadimitriou CA, Kouroussis C, Moulopoulos LA, Vlahos G, Rodolakis A, Kiamouris C, et al. Ifosfamide, paclitaxel and cisplatin first-line chemotherapy in advanced, suboptimally debulked epithelial ovarian cancer. Cancer. 2001; 92:1856–1863.

19. Polyzos A, Kosmas C, Tsavaris N, Toufexi H, Lagadas A, Gogas H, et al. Paclitaxel-ifosfamide-cisplatin as salvage chemotherapy in ovarian cancer patients pretreated with platinum compounds and paclitaxel. Anticancer Res. 2007; 27:1645–1651.
Supplementary Fig. 1
Box-and-whisker plots of the CI values of 10 chemotherapeutic agents in primary and recurrent disease. The bottom and top edges of the box represent the 25th and 75th percentiles, respectively, whereas the horizontal line corresponds to the median value. The vertical lines show the range of values. The CI appeared to be higher in recurrent disease than in primary disease for most anticancer drugs. *p<0.05. CI, chemosensitivity index.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download